What it is
The placenta is a unique organ. It appears only during pregnancy and disappears after the birth of the child. The task of the placenta is to provide the baby with nutrition and the delivery of all substances, vitamins, and oxygen necessary for its normal growth and development. At the same time, the placenta helps excrete the baby’s metabolic products into the mother’s body.
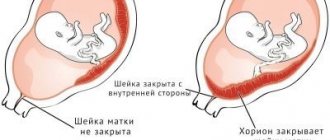
Placenta previa is a concept that refers to the location of this temporary and very necessary organ in the uterine cavity. Presentation is always a pathology, because the term itself has the meaning of finding the placenta on the path along which the baby will need to pass during childbirth.
Normally, the placenta insertion site should be such that the baby’s “baby place” does not interfere with being born. If we are talking about presentation, this means that the placenta is located low, partially or completely blocked the exit to the pelvis.
Low placentation occurs quite often in early pregnancy. Before the 20th week of pregnancy, partial or marginal presentation is registered in approximately 10% of pregnant women. But the placenta has the ability to rise above the cervical region following the walls of the uterus growing along with the fetus. Therefore, by the 30th week of pregnancy, only 3% of pregnant women have a presentation, and by the 40th week - only 0.5-1% of expectant mothers. The process of the placenta moving higher is called migration.
The placenta is finally formed only by 10-12 weeks of pregnancy. Before this, the place where the fertilized egg “grows” into the endometrium is called the chorion. There are three types of presentation.
- Complete - the internal os is completely blocked by the placenta. This is a very dangerous, threatening condition in which spontaneous childbirth is impossible and there is a high probability of death of the fetus or mother as a result of spontaneous massive bleeding.
- Incomplete - the placenta partially covers the internal os of the cervix. In most cases, independent natural childbirth is also impossible; the danger for the baby and mother is great.
- Low or lower - the placenta is located above the entrance to the cervical canal, but the distance from it to the “baby place” does not exceed 7 centimeters. The internal os is not covered by the placenta. If the “child’s place” is located too low and affects the edge of the pharynx, the presentation is called marginal.
Natural childbirth with such placenta previa is quite possible, however, it will require special attention from doctors, and extreme caution from pregnant women during the process of bearing the fetus.
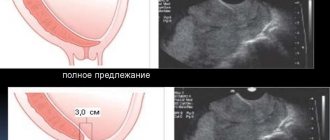
Doctors can determine the type and degree of presentation using ultrasound scanning. During each routine ultrasound, close attention is paid to the placenta. Its localization is determined along the anterior or posterior wall of the uterus, and the distance from the internal os (entrance to the cervical canal) to the edge of the “child’s place” is measured.
If it is at least 3 centimeters, a diagnosis of “low placentation” or “first degree of placenta previa” is made.
It should be noted that the lower presentation is the safest of all three types of presentations. Doctors’ prognoses are more favorable with it, but this arrangement of the “children’s place”, of course, is not a variant of the norm. Certain hazards and risks exist.
Diagnostics
Low placentation is detected by ultrasound. During the examination, the doctor evaluates several parameters:
- The distance from the edge of the placenta to the internal os of the uterus.
- Condition of the placenta, its thickness, the presence of calcifications.
- Correspondence of the degree of maturity of the placenta to the gestational age.
- Condition of chorionic villi in the endometrium.
Ultrasound examination is carried out over time at 18-21 and 32-34 weeks, as well as before birth. If bleeding develops, an ultrasound is performed to assess the condition of the placenta and exclude its abruption.
Causes of low placentation
By and large, it is almost impossible to somehow influence the place where the placenta is formed. It will appear where the fertilized egg manages to attach itself at the time of implantation.
The fertilized egg is implanted into the uterine cavity approximately 8-9 days after fertilization, from this moment the chorion is formed, which subsequently becomes the placenta. It is impossible to determine exactly where the fertilized egg will “float”. But there are risk factors that increase the likelihood that the blastocyst will implant too low.
First of all, such factors include pathologies of the structure of the uterus, diseases of the woman’s reproductive system, and the consequences of surgical interventions.
Thus, women who suffer from inflammatory processes of the endometrium, have had abortions or other curettages, and have a history of cesarean section have a higher chance of low placentation in subsequent pregnancies. Such causes are called uterine or intrauterine. These include:
- endometriosis;
- operations performed on the uterus - (abortion, removal of fibroids, diagnostic curettage, cesarean section);
- complicated previous births;
- uterine fibroids;
- underdevelopment and abnormal congenital structure of the uterine body;
- incompetence of the cervix (isthmic-cervical insufficiency);
- pregnancy with several fetuses at the same time.
The reason for the fixation of the fertilized egg in the lower part of the uterus may also be an enzyme deficiency of the membranes themselves. Such reasons for the development of a low placenta are called fetal. These include:
- hormonal disorders in women;
- inflammatory diseases of the appendages, fallopian tubes, ovaries.
With a second pregnancy, a low-lying placenta is more likely than with a first pregnancy. The more women give birth, the higher the likelihood of developing inferior placentation with each subsequent pregnancy.
It is believed that the risk group includes both overweight women and women who were unable to quit smoking after pregnancy. If during a previous pregnancy the placenta was located low, it is highly likely, according to experts, that the “baby place” will be located low in the subsequent pregnancy.
In addition, there is a certain genetic dependence - a woman can inherit a tendency to lower placentation from her own mother.
Low placentation during pregnancy at 20-21 weeks
The placenta connects mother and baby, providing the latter with nutrition and oxygen. If pregnancy proceeds normally, it is located on the back or front wall of the uterus, but there are exceptions to its location.
Causes of low placentation during pregnancy at 20 weeks
Sometimes there are deviations in the location of the placenta in the uterine cavity; its location is determined using ultrasound. It turns out that it is located in the lower part of the uterus and, in some cases, can block the internal os.
The reasons for this phenomenon during pregnancy may be the following:
- Multiple pregnancy.
- Problems with the uterus, for example, such as underdevelopment of this organ.
- Consequences of abortion or any infectious diseases.
- The patient’s age also influences – the risk of this pathology increases after 35 years.
Most often, this pathology can occur in those women who have not had their first pregnancy, for example, they have already had two or more; there is also a risk of a low location of the placenta due to endometritis and the presence of cesarean section scars.
The exact cause of this pathology in pregnant women has not yet been identified, but we can say with full confidence that a low placenta can lead to a number of complications, including termination of pregnancy.
Doctors place women with this pathology under special control and, in some cases, admit them to a hospital for constant monitoring. But the expectant mother should not panic if this pathology is detected at week 20, as a rule, due to the growth of the fetus, its attachment rises, and until the moment of birth, it should be at a normal level.
What are the risks of low placentation during pregnancy (video)
Now it is clear why this situation and this position of the placenta are dangerous, why the uterus has dropped, what type of placenta is (for example, extrachorionic), what does a high placenta mean and what needs to be done for it to return to normal.
Source: https://mamafm.ru/beremennost/bolezni/nizkaya-platsentatsiya-pri-beremennosti
Diagnosis and symptoms
Low placenta previa can be indicated by spotting at any stage of pregnancy. The doctor may be confused by the increased height of the uterine fundus, which is ahead of the actual gestational age, as well as the incorrect position of the fetus in the uterine cavity - pelvic or transverse presentation of the baby is often accompanied by low placentation.
Bloody discharge from the genital tract with inferior placenta previa usually first appears after 12-13 weeks of pregnancy. They may be more or less abundant. They often continue until childbirth.
But the most common bleeding is in the last trimester of pregnancy, when the walls of the uterus are stretched so much that partial microdetachments of the “baby place” from the uterine endometrium occur.
In a third of pregnant women with low placentation, such bleeding is observed after 35 weeks of pregnancy. Six out of ten women experience fairly heavy bleeding during childbirth. Even careless severe coughing, laughter, sex, constipation, physical activity and severe stress can provoke bleeding in pregnant women with a low position of the placenta. Any tension in the uterine muscles is dangerous due to small detachment and exposure of blood vessels.
Clinical picture
The fact that a woman has a placenta that has grown into a scar on the uterus can only be understood during childbirth, when the placenta does not come out on its own. The umbilical cord is visible from the genital tract, but the “baby spot” itself does not appear. The following specific signs indicate this:
- Kustner-Chukalov - by pressing above the womb, the umbilical cord is retracted.
- Alfelda - the clamp placed on the umbilical cord does not lower.
- Klein - when straining, the umbilical cord does not come out of the genital slit.
- Strassmann - with the hand grasping the umbilical cord, one feels the pulsation of blood that occurs when the uterus is beaten.
In addition, there is no Schroeder sign: changes in the contours of the uterus, its compaction and elongation of the body, deviation of the fundus to the right. But the most important and dangerous symptom of placental rotation is bleeding in the third stage of labor. Since in some places the villi do not penetrate as deeply, certain areas still separate. And through the gaping vessels the mother’s blood begins to flow out. And the situation can be very dangerous, since in the absence of adequate correction, complications develop in the form of hemorrhagic shock and disseminated intravascular coagulation syndrome.
Danger and risks
It is not difficult to guess what threatens a low placental location. In the early stages, this is dangerous with the threat of spontaneous miscarriage, and at a more advanced stage of gestation - with the threat of premature birth. Women with this problem often develop preeclampsia at the end of the second and third trimesters, which only increases the risk of an unfavorable outcome. Half of pregnant women have iron deficiency anemia.
If the placenta has formed in the early stages and is attached low, then the likelihood that the baby will take an incorrect position in the uterine cavity increases by 50%. The baby will instinctively choose a position in which its head will not come into contact with anything, including the placenta.
The baby will most likely adopt a pelvic rather than a cephalic presentation, which will greatly complicate the birth process or even be an indication for a cesarean section.
For a baby, a low-lying placenta is a risk factor for the likelihood of developing hypoxia. Prolonged chronic oxygen starvation can cause the death of the baby and irreversible changes in the structures of its brain.
Also, placental insufficiency, which develops if the “baby place” is omitted, can lead to delayed fetal development. The lower part of the uterus is less well supplied with blood than the body and fundus of the uterus, which is why the baby will receive less of the nutrients it needs.
The abnormal location of the organ feeding the baby is dangerous. If the placenta is attached low, the woman may at any time experience bleeding, which can have very sad consequences.
Causes of placental abruption
There are cases when the placenta is damaged and placental abruption begins, then its functions are disrupted. The placenta can be damaged by infections (chlamydia during pregnancy, ureaplasma, anaerobes during bakvaginosis, etc.), various intoxications, including nicotine, antibodies during Rh conflict. The placenta functions worse in hypertension, diabetes mellitus, and vegetative-vascular dystonia, since these diseases are characterized by vasospasm. A damaged placenta during pregnancy cannot perform its functions.
- Because of this, the fetus begins to receive less oxygen. Chronic intrauterine fetal hypoxia develops. If the unborn baby is seriously limited in oxygen and nutrition, then his growth slows down, and this condition is called “fetal growth retardation syndrome.” If such violations are not corrected in time, the consequences can be tragic. During childbirth, the lack of oxygen sometimes worsens, and the doctor may decide to perform a caesarean section to save the child; you can also resort to hyperbaric oxygenation, but if not everything is so serious.
- A damaged placenta produces fewer hormones that relax the uterus. Because of this, there may be a risk of miscarriage.
- In a placenta experiencing starvation, special substances begin to be produced that trigger the development of gestosis. With this disease, swelling of the arms and legs occurs during pregnancy, protein appears in the urine and blood pressure rises, and there may also be more serious complications.
To prevent placental disorders, antenatal clinics during pregnancy prescribe several courses of metabolic therapy, including vitamins and substances that improve fetal-placental blood flow, for example chimes. These drugs help the placenta perform its functions better, which means they prevent the development of various complications.
Functions of the placenta
The condition of the placenta during pregnancy can be assessed according to the second (at 20-24 weeks) and third (at 32-34 weeks) ultrasound screening. At these times, structural changes can be detected: calcifications, cysts, premature aging of the placenta, its swelling (placentomegaly). Calcifications in the placenta do not appear at all from excess calcium, as many people think. Simply, under the influence of damaging factors, small areas of the placenta die off, and then calcium salts are deposited at the site of damage. If we see similar changes on ultrasound, we usually make a diagnosis of “fetoplacental insufficiency”.
At the third screening, it is also possible to detect a lag in the size of the fetus from the norm, which sometimes indicates a syndrome of delayed development. True, if both you and your husband have a fragile physique, then a lag of 1-2 weeks can be considered acceptable. If, along with changes in the placenta, ultrasound also revealed hyperechogenic intestines in the fetus, suspension in the amniotic fluid, high or low water levels, then we can talk about the presence of an intrauterine infection, which caused damage to the placenta. However, the presence of structural changes in the placenta does not mean that it does not fulfill its functions. To check placental blood flow, it is necessary to do a Doppler ultrasound. This study is performed using an ultrasound machine. And the influence of ultrasound on pregnancy does not have any negative effect, you should not be afraid of it. It can be used to see blood flow in the uterine arteries and umbilical cord arteries. If you suspect intrauterine hypoxia of the fetus, you can also look at the blood flow in its middle cerebral artery. The condition of the fetus, which is assessed using CTG cardiotocography during pregnancy, also indirectly indicates a dysfunction of the placenta.
The method is based on recording the fetal heartbeat for 10 minutes. There are special devices that perform computer processing of results according to special criteria. If such a device concludes that the Dawes-Redman criteria are met by the 10-12th minute, then everything is in order. If they are not met within an hour, then the fetus has a lack of oxygen. True, not all hospitals have such devices. In some large clinics, to study the function of the placenta, they also determine the level of hormones that it produces. If the doctor finds that you have dysfunction of the placenta and offers inpatient treatment, do not neglect his recommendations, they will help you avoid complications in the further course of pregnancy.
Low placenta previa during pregnancy
Low placentation during pregnancy is a serious complication that requires constant monitoring of the woman and emergency care if necessary.
The placenta is a temporary organ that forms by the second week of pregnancy, woven from the vessels of the mother and fetus. It attaches to the wall of the uterus, grows, develops and reaches maturity. Functions of the organ:
- saturation of the child’s blood with oxygen and removal of carbon dioxide;
- delivery of nutritional components to the fetus and removal of waste products;
- synthesis of hormones necessary for the normal development of pregnancy and preparing the female breast for milk production;
- immune protection of the baby in the womb.
The norm is that the placenta is attached to the posterior or lateral wall of the uterus. But if it is located too low, problems may begin.
Low placenta previa is an abnormality during pregnancy. It is characterized by attachment in the lower part of the uterus, which completely or slightly covers the internal pharynx. This means that complications are possible during pregnancy and childbirth.
Schematic representation of the problem
The condition often resolves spontaneously as the upper uterus moves out of place. This phenomenon is called placental migration. But in general, the risk of fetal death is quite high: from 7 to 25%.
The cause of the baby's death may be acute hypoxia due to insufficient placental blood supply or premature birth.
This pathology is also dangerous for a pregnant woman. Bleeding that occurs with placenta previa causes death in 1-3% of women.
The exact location of the attachment can be determined by ultrasound in the 3rd trimester. Normally, the location of the organ is located at a distance of 5 or more centimeters from the internal os of the uterus.
Most causes of low placentation are due to diseases and conditions that occurred before pregnancy.
What causes deviation:
- inflammatory and infectious processes in the genital organs;
- damage to the uterine mucosa;
- previous miscarriages or abortions;
- gynecological interventions;
- multiple pregnancy. Women with twins or triplets are automatically at risk;
- birth by caesarean section;
- fibroids, endometritis and other diseases of the uterus;
- smoking, excessive alcohol consumption;
- many births;
- anomalies of the structure and development, functioning of the uterus;
- woman's age over 35 years.
The most common cause of low presentation is a previous uterine curettage. The procedure damages the mucous membrane, which prevents the fertilized egg from attaching to the upper part of the organ.
Consult a doctor
The insidiousness of deviation is that it practically does not manifest itself. Symptoms appear already at an advanced stage, when irreversible processes take place in the body, for example, exfoliation. These signs:
- heaviness in the lower abdomen, nagging pain;
- bloody issues. When they appear, you need to call an ambulance;
- death of the fetus in the womb or its excessive activity due to hypoxia - lack of oxygen;
- severe toxicosis - 30% of women with this diagnosis suffer from it;
- In approximately half of the cases of pathology, ultrasound reveals a breech presentation of the fetus.
A pregnant woman herself cannot suspect an anomaly until clear symptoms appear. The condition is monitored during routine ultrasounds. The study allows not only to identify the problem, but to determine its extent and severity.
Types of low presentation depending on the location of the placenta:
- rear This arrangement of the organ is the most favorable option. In most cases, in later stages, the baby's place moves upward, freeing the birth canal. Pregnancy is relatively comfortable;
- front In this case, you need to prepare for difficulties. If the baby is large and active, he will put pressure on the placenta. This will cause problems with the umbilical cord, the risk of entanglement and compression. Such a presentation rarely changes before childbirth, which means that the birth canal will not be free;
- complete or partial, when the organ obscures the os of the uterus. Deviation requires great caution. It is important to discuss all the details with your doctor before giving birth and prepare for the fact that you will have to give birth by cesarean section.
Causes of placenta accreta
Increased strength of the connection between the wall of the uterus and the placenta, as well as an unevenly strong connection between them, is observed when the placenta is located entirely or partially on the wall of the uterus, altered by the inflammatory process (metro-endometritis), a scar (postoperative, after too vigorous curettage of the mucous membrane). lining of the uterus), neoplasm (submucosal fibroid) or malformation of the uterus (location of the placenta on the septum of the bicornuate uterus).
The same can be observed in diseases of the woman in labor that contribute to the development of degenerative processes in the placenta: chronic nephritis, severe forms of toxicosis of pregnancy, chronic infections with a long course, significant post-term pregnancy, etc. In such cases, changes are observed in the placenta itself, usually having a nested character. But these changes can affect the entire placenta. In such cases, the placenta can be enlarged in size and thickened or, conversely, thinned (leathery placenta), has additional lobules, the placental areas of which may be located at a distance from the main one.
Finally, the connection between the placenta and the uterus can be excessively strong if the villi, which have grown into the compact layer of the falling membrane, have completely sprouted it or even gone beyond it and penetrated the muscular layer of the uterus. In such cases, overgrown villi can penetrate right up to the serous membrane covering the uterus. This ingrowth occurs due to an increase in the proteolytic ability of the chorion in the absence of resistance to this from the mother’s body.
If the chorionic villi do not extend beyond the spongy layer of the falling membrane, they speak of relative placenta accreta (placenta adhaerens). In the case of their penetration into the muscle layer, they speak of true accretion, (ingrowth) of the placenta or its tight attachment (placenta accreta s. increta).
Such a pathologically strong connection can extend to the entire maternal surface of the placenta or only to the surface of its individual lobules.
True placenta accreta is an extremely serious but rare complication of childbirth: it occurs once in 10,000 births.
The incidence of placenta accreta has increased from 1/30,000 in the 1950s to 1/500-2000 in the 1980s and 90s. The risk for women who have had placenta previa increases by 10% to 25% if they have had one cesarean section and by 50% to 67% if they have had >four cesarean sections.
Other factors include:
- Mother's age >35 years.
- History of multiple births.
- Submucosal uterine fibroids, Smoking.
- Pathology of the uterus, for example, Asherman's syndrome.
What to do
- analysis of symptoms: discharge, abdominal pain;
- Ultrasound is the main type of diagnosis, safe and informative. Carried out at 12, 19-20 and 30 weeks;
- bimanual examination of the vagina (provided there is no bleeding).
After confirming the diagnosis of low placenta previa, the doctor prescribes treatment and gives recommendations to correct the situation. If desired and competent actions are taken, the location of the organ can be changed.
If the pregnancy is proceeding normally, and the term has not reached 35 weeks, treatment is conservative. Strict bed rest, monitoring of the fetus and the intensity of bleeding are indicated. Any exertion or sexual contact is prohibited.
Regular examinations are recommended
There are no medications that elevate the placenta. Medicines are prescribed to help improve the condition of the pregnant woman and promote migration of the baby's place. This:
- tocolytics, antispasmodics - stimulate stretching of the lower parts of the uterus;
- agents that reduce myometrial tone;
- iron-containing drugs - prescribed to women with bleeding to prevent iron deficiency anemia;
- medications that activate placental blood circulation - to avoid the development of hypoxia in the fetus;
- magnesia, intravenous glucose, vitamins.
How does this condition affect pregnancy?
Often the baby's place is attached to the back wall of the uterus. The norm is considered to be its attachment to the bottom (at the top). But sometimes it is attached to the front wall. If its location is very low, less than 6 cm from the edge of the exit from the uterus, this is fraught with consequences. After 23–27 weeks, the baby begins to move, and after 31, movements become more active. During this period, it can damage the placental organ or the umbilical cord, especially with breech presentation.
The second disadvantage of this feature is the poor blood supply to the lower part of the uterus, which threatens the fetus with a lack of oxygen.
If at 18–19 weeks low placentation is recorded along the posterior wall, then the placental organ by the end of the period in most cases migrates higher. But with a front attachment, the opposite may be true, since migration is directed in the opposite direction.
Another danger is the extrachorionic type of placentation, where the placenta is shifted to the center, creating a kind of shelf. This arrangement requires close monitoring of the pregnant woman throughout the entire period of gestation.
Why is it dangerous?
The consequences can be dire
Low placenta previa during pregnancy is a condition that is dangerous for both the woman and the fetus. Among the unpleasant consequences:
- the baby can damage the placenta with active movements. This is especially true for later stages, when a large baby puts pressure on the organ and is able to catch the placenta membrane;
- with low placentation, the cervix is not intensively supplied with blood, which is fraught with the development of fetal hypoxia;
- the anomaly threatens complications during childbirth, since the baby’s place prevents the baby from leaving the womb;
- insufficient placental blood circulation can cause increased activity of the fetus, which is fraught with twisting and clamping of the umbilical cord;
- Placental abruption is a dangerous condition that leads to the death of the fetus, and sometimes the woman. When complications occur, the stomach begins to ache and bleeding appears;
- Pregnant women with this diagnosis often experience low blood pressure and develop late gestosis.
With low presentation, the blood supply to the lower part of the uterus deteriorates. Consequently, the fetus is not fully fed with useful components. This increases the risks of intrauterine growth retardation and hypoxia.
If placental insufficiency and deterioration of blood flow are diagnosed, maintenance therapy is prescribed to compensate for the lack of nutrients in the fetus.
This is what low placentation threatens. A child can suffer from an anomaly at any stage of pregnancy. Caution and strict adherence to the doctor’s recommendations will help protect him and yourself from complications.
Organ pathologies
The placenta, like any other organ, is at risk of developing pathologies under the influence of external factors. Its pathological condition in most cases can provoke a threat to the normal intrauterine development of the fetus. Pathology of the placenta has a detrimental effect on the growth and development of the fetus and threatens with irreversible consequences in the future. Since the main function of the placenta is to protect the baby and provide it with nutrients until birth, dysfunction of the organ is a serious cause for concern.
A pregnant woman should not neglect routine examinations, tests and ultrasound. Most problems associated with the functioning of the placenta can be eliminated with the help of drug therapy, subject to timely consultation with a specialist. A pregnant patient should be very attentive to changes in health status. Painful sensations localized in the lower part of the abdominal cavity, bleeding, general weakness, tachycardia, nausea and chills should be a reason to immediately consult a doctor. Common pathologies of the placenta include:
- placental abruption, threat of miscarriage;
- intraplacental blood flow disorders, thrombus formation;
- anomalies in the structure of the organ;
- inflammatory processes;
- germination into the wall of the uterus;
- thickening of the placental walls;
- neoplasms of the placenta;
- placental infarction;
- incorrect placement near the os of the uterus.
To eliminate problems with placental abnormalities, the doctor needs to identify the cause of their occurrence.
What provokes pathological deviations of this vital organ for the child? All of the above pathologies arise due to:
- severe toxicosis;
- diabetes mellitus, atherosclerosis, history of chronic somatic diseases;
- gestosis in the third trimester;
- various infections (flu, toxoplasmosis, etc.);
- conflict between the Rhesus of mother and baby;
- iron deficiency anemia;
- age of a pregnant woman over 35 years old;
- history of abortion;
- nervous fatigue, stress;
- bad habits, poor diet;
- large weight gain or anorexia;
- congenital anomalies of the fetus.
Pregnancy is an amazing time in a woman's life. A new life appears and grows in her body - in comparison with this miracle, the fact that at the time of pregnancy new body organs appear in her does not seem particularly strange. And the main one of these organs is the placenta.
The baby is completely dependent on the condition of the mother’s placenta: it is his only source of nutrition and breathing.
When it rises
- 1st trimester. The first planned ultrasound is performed at 12-13 weeks, at which time the anomaly is detected. There is no need to worry during this period, since in 70% of cases the placenta rises by 20-21 weeks;
- 2nd trimester. By the period of twenty weeks, placental blood circulation is improved, but with low presentation it is disrupted, especially if the fetus is large and puts pressure on the organ from above. In this case, the gynecologist admits the pregnant woman to the hospital with strict adherence to bed rest and drug therapy. Usually by 22-23 weeks the baby's place rises up. If the situation does not change, the doctor gives the woman recommendations regarding lifestyle and continues to try to improve the situation;
- 3rd trimester. Mostly by 32-34.5 weeks the placenta moves upward under the pressure of the growing uterus. Then the problem disappears. If during pregnancy it does not come into place, at 36 weeks the issue of caesarean section is decided. This is especially important with complete presentation.
The cause could be curettage of the uterus
Depending on the trimester and the nature of the location of the placenta, different actions are taken to correct the anomaly. It is important for a woman to be patient and not panic.
In most cases, the placenta rises towards the end of pregnancy. If this does not happen, but the woman and baby feel well, a caesarean section is performed.
What happens to the placenta in the 3rd stage of labor
In a normal birth, contractions do not stop after the baby is born. The uterus is rounded and becomes smaller. The placenta (baby place) does not have such properties, so the mechanisms of its separation are triggered. Blood accumulates between it and the wall of the uterus, which completes this process. Alternatively, the separation may occur from the edge to the center.
To assess the condition of a woman, they focus on external signs of abruption of the fetal place:
- The uterus rises above the navel.
- The outer end of the umbilical cord gradually lengthens.
- The separated baby's place forms a protrusion above the symphysis.
- If a woman in labor strains, the end of the umbilical cord will lengthen and will not retract back.
- When pressing on the abdomen, the umbilical cord does not shorten.
A combination of several of these symptoms indicates separation. If this does not happen within 30 minutes, then placenta accreta to the uterus is suspected.
What not to do
Pregnant women with low placentation must be constantly monitored by a doctor. If you follow his recommendations exactly, everything will be fine. What you shouldn't do:
- worry. Modern medicine successfully treats pregnant women with low placental attachment. In 90% of cases, a woman gives birth to a healthy baby. Moreover, 60% of births are carried out naturally, and only 40 - by cesarean section;
- have sexual intercourse. Sex at any stage can damage the organ and lead to detachment. This only applies to women with low placenta previa;
- play sports, do abdominal exercises, lift weights, walk a lot. Decide what is more important, an active lifestyle or the health of the child;
- do douching and any other vaginal manipulations so as not to harm the pregnancy;
- worry, get nervous, get irritated. This will lead to an unhealthy emotional atmosphere and aggravate the condition. Develop stress resistance;
- travel on public transport, visit places with large crowds of people. They can push there, which will cause even greater prolapse of the organ;
- Ignore the doctor's recommendations and do not go on conservation when necessary.
You have to be patient
Low placentation is not a disease, but a special condition. The situation requires, first of all, not treatment, but correction. Much depends on the mood of the pregnant woman, her actions, and how accurately they correspond to the advice of doctors.
Preventive measures will help to avoid anomalies. These include:
- prevention of infectious and inflammatory diseases, their timely treatment;
- maintaining a healthy lifestyle: proper nutrition, adherence to work and rest schedules, avoiding alcohol and tobacco abuse;
- protection against unwanted pregnancy, so that there is no history of abortion;
- performing a caesarean section only in cases where there are vital indications;
- performance of gynecological manipulations and operations in trusted clinics by experienced doctors.
About the author : Borovikova Olga
What causes the condition
The main reasons for low placentation during pregnancy lie in changes in the structure of the body and cervix. Most often this happens in the following cases.
- Uterine fibroids. Any neoplasms, especially in the area of the lower segment and cervix, provoke improper attachment of the chorion due to abnormal blood supply to these areas and deformation of the uterine cavity due to their submucosal location.
- Scar on the uterus. Most often it remains after a cesarean section or removal of myomatous nodes. As the tissues heal, a rich blood vascular network is formed in them, which “attracts” the fertilized egg.
- Cervical pathology. Chronic inflammatory processes in the cervix lead to tissue restructuring, including in the lower parts of the body. Every third woman with low placentation during pregnancy did not have the necessary treatment for erosion, ectopia, and cicatricial deformities during the planning period.
- Chronic inflammation. Infectious processes inside the uterine cavity (endometritis), in the area of the appendages lead to pathological changes in the endometrium, as a result of which it becomes “unattractive” to the amniotic sac.
- Intrauterine interventions. Previous abortions or miscarriages, an intrauterine device for some time, diagnostic procedures (eg, curettage, hysteroscopy) also increase the risk of low placentation.
- Neuroendocrine disorders. Hypoplasia (underdevelopment), disturbances in the secretion of hormones by the ovaries, as well as changes in the functioning of the pituitary gland and hypothalamus (brain structures) lead to the fact that the endometrium does not have time to mature by the time of implantation of the fertilized egg, which leads to its fixation in the lower sections.
- Poor circulation in the pelvis. All diseases associated with stagnation of blood in the pelvic vessels also provoke low placentation. These include pathology of the cardiovascular system (for example, heart failure, arterial hypertension), liver and kidney diseases.
What is placenta previa
Often, when examining a pregnant woman’s condition, placenta previa is diagnosed. There is a need to study what it is and how it manifests itself.
The bladder ensures interaction between the body of mother and child. This body performs the following functions:
- gas exchange;
- nutritious;
- immunoprotective;
- hormonal.
The physiological location of the fertilized egg suggests its location on:
- fundus of the uterus;
- posterior and lateral walls of the uterine body.
This area is least subject to change. It is also the area of best vascularization.
Attachment to the posterior wall ensures that the embryo is protected from unexpected damage. When the bubble is attached from the pharynx, then a violation occurs.
Placenta previa is a pathological location
amniotic sac.
As a result, the embryo develops in the wrong place. It should be borne in mind that this condition directly affects the outcome of labor.
Placenta and its role during pregnancy
The placenta (the so-called baby's place) is a temporary organ that exists only during pregnancy. It begins to form after the implantation of the fertilized egg into the uterine mucosa, and its growth ends at the 8th week of pregnancy.
By the end of the waiting period, the placenta ages and fades, and it leaves the body some time after the birth of the baby. The “children’s place” is a unique organ because it belongs to both mother and baby at the same time.
During the development and maturation of the fetus, it performs the following functions:
- Respiratory: thanks to the placenta, oxygen is supplied to the baby from the mother’s blood, and carbon dioxide is transported back through its vessels;
- Nutritional: this organ filters the necessary nutrients, vitamins, minerals from the mother’s blood and supplies them to the fetus;
- Immune: the “baby place” provides the child with protective substances, forming his immunity, and also protects the fetus from the aggressive effects of antibodies in case of Rh conflict;
- Hormonal: forms hormones that ensure the normal course of pregnancy and protect against miscarriage - estrogens, progesterone, human chorionic gonadotropin and others.
Causes of placenta previa
There is still no consensus on what influences the appearance of pathology. There is also no way to influence placental formation. In general, the reasons for presentation
Placentas can be divided into the following categories:
- Aspects of embryonic development.
- Aspects that determine the health of a pregnant woman.
To the features of the embryonic structure
it is customary to refer to:
- trophoblast implantation failure;
- weak enzymatic action;
- delay in the development of the fertilized egg.
The presence of these factors makes it impossible for the fetus to implant in the upper section.
The state of the maternal body is determined by the following phenomena:
- inflammation in the endometrial area (often frequent);
- processes of endometrial atrophy;
- diseases of infectious nature;
- stagnant processes
in the reproductive organs (resulting from chronic pathologies of the cardiovascular and endocrine systems, as well as slow blood supply); - surgical intervention in the uterine area;
- cases of abortive interruption
of the gestation period; - complications after previous labor;
- abnormal structure
of the uterus; - detection of endometriosis and uterine fibroids;
- underdevelopment of the uterus;
- the presence of isthmic-cervical insufficiency;
- the presence of endocervicitis;
- pathological processes in the cervical area;
- neuro-endocrine disorders;
- previously diagnosed facts of pathological location;
- exposure to addictions (systematic use of nicotine, alcohol-containing liquids and narcotic substances);
- multiple births;
- hormonal imbalance.
These causes of placenta previa affect the formation of the mucous membrane in the uterine area. If it is underdeveloped, the lower part of the cavity is an acceptable place.
How to give birth
If a woman is regularly examined during the period of bearing a child, then you can count on a successful natural resolution.
The course of labor depends on the following factors:
- location of the child's seat;
- the presence or absence of complications during pregnancy;
- accompanying pathologies.
If the placenta does not cover the uterine os, the amniotic sac is punctured during childbirth. When passing through the birth canal, the fetus presses the head of the organ against the uterus, which prevents its detachment.
If the baby is breech, a caesarean section is indicated.
We recommend reading the article about uterine fibroids during pregnancy. From it you will learn about the peculiarities of bearing a child with a diagnosed tumor, possible complications, pregnancy management tactics, and how childbirth occurs.
Why is Utrozhestan prescribed during pregnancy? Read here.
Placenta previa: types
In medical practice, it is customary to distinguish various types
violations
_
Their classification is based on the following factors:
- determining the location of the ovum using transvaginal ultrasound;
- identification of the location of the ovum during labor (the condition for fulfillment is the presence of a 4-centimeter cervical dilatation or more).
The results of transvaginal examination allow us to divide pathology into the following types:
Data obtained during delivery determine the existence of the following types of disorders:
Complete placenta previa
Complete presentation is presented in the form of a thorough overlap of the uterine pharynx with placental tissue.
This position of the amniotic sac creates restrictions for natural delivery. Even with the cervix fully dilated, the fetus will not be able to continue
movement along the birth canal.
Full presentation is also known as centric position.
Its peculiarity is the need for a caesarean section.
Other types of pathology do not exclude the possibility that the amniotic sac will move. In the case of the central type, such an outcome of events does not exist.
Central placenta previa is dangerous due to the following consequences:
- complete placental abruption long before labor;
- the occurrence of embryonic hypoxia;
- slow development of the child;
- ovum accretion;
- early rupture of membranes.
This attachment provides for the complete exclusion of intimacy
and minimizing physical stress.
Incomplete placenta previa
Incomplete placenta previa is a partial overlap
internal opening of the cervix. With this arrangement, a small area remains free.
Incomplete placenta previa is also known as partial placenta previa. A subtype of this pathology is the marginal and lateral location.
The marginal location determines the presence of the lower part of the fertilized egg near the edge of the internal opening of the cervix. In this case, it can be either along the front wall or along the rear arch. A single level is noted for the cervix and placental edge. When positioned sideways, there is partial overlap.
This violation determines the impossibility of passing the child's head into the neck. This feature necessitates a caesarean section.
Regional placenta previa can be diagnosed by the anterior wall.
Attaching the placenta to the anterior wall is a variant of the gynecological norm.
Such a case is not usually classified as a pathological attachment.
This is due to the likelihood of stretching the uterus under the weight of the fetus and its further movement along the anterior wall.
Marginal presentation of the placenta along the posterior wall is usually classified as low or incomplete attachment of the membranes. It manifests itself as being on the posterior fornix.
This option is less dangerous than placing it on the front wall. This is explained by the difference in the load on the uterine area. However, bleeding may occur.
More on the topic Norms and pathologies of placenta attachment
Placenta previa.
Placenta previa.. Medical issues. Pregnancy and childbirth. All indicators are normal, only placenta previa was diagnosed at 2 cm, closing the pharynx. I didn’t even expect that it could be serious and didn’t check all the details with the doctor.
Placenta previa(((
the placenta can rise in literally a week, that’s what the doctor told me at one time, so everything will be fine. Well, as a last resort, if it doesn’t rise, then they’ll just cut it down and that’s it!
placenta previa
placenta previa. Analyzes, studies, tests, ultrasound. Pregnancy and childbirth. But the diagnosis is no longer presentation, but low placentation, and somehow it even went away a little, otherwise...
marginal placenta previa
marginal placenta previa. LCDs, maternity hospitals, courses, honey. centers. Pregnancy and childbirth. marginal placenta previa. Well, before I could get enough of our vacation, I got...
Placenta previa
Placenta previa. Analyzes, studies, tests, ultrasound. Pregnancy and childbirth. I had complete placenta previa, by 30 weeks it had risen by 2 cm, by 4 cm by labor and delivery, and I gave birth on my own.
Marginal attachment of the umbilical cord to the placenta
Marginal attachment of the umbilical cord to the placenta. Analyzes, studies, tests, ultrasound. I just had an ultrasound and they also installed the marginal attachment of the umbilical cord to the placenta, they said it was interesting, but...
34 weeks - marginal placenta previa.
in the clinic, after two ultrasounds, they wrote that the placenta was marginally previa, and another paid doctor measured 2, then 2, 5 cm both times - this is low placentation, not previa...
Placenta previa
Placenta previa. Medical issues. Pregnancy and childbirth. placenta previa. The result is stunning - 2 cm above the pharynx, or the placenta has risen (and let me remind you, I’m in my fourth birth, and she The doctor wrote in the conclusion that it’s a bit low, but...
Regional placenta previa
Regional placenta previa. Medical issues. Pregnancy and childbirth. Regional placenta previa. What kind of animal is Etta? It sounded today at the 32-week ultrasound. I don’t deliberately go anywhere (in the sense of reading) - you know less, you sleep better (for now).
Sex and breech
But tell me, if there is placenta previa (at first it was complete, now it’s marginal), then it’s a no-no to have sex at all? (whine:)) One doctor told me this, now I’m tormented by my conscience... I’m 19 weeks. Or maybe I should take something after sex (just not noshpa, my blood pressure is low) for safety?
Regional placenta previa
Regional placenta previa. Analyzes, studies, tests, ultrasound. Pregnancy and childbirth. Marginal presentation is very common. Usually the placenta rises towards birth. Caesarean section is when the placenta completely covers the pharynx, but this is not the case.
placenta along the edge of the internal os
Girls, please enlighten me, marginal placenta previa - what kind of animal is this? If the placenta is on the front wall, then 99% of it will rise, if on the back wall, then maybe not...
placenta previa
placenta previa. Ailments, diseases, toxicosis. Pregnancy and childbirth. The first time I had complete placenta previa, it rose by 30 weeks. in this low position initially, first along the edge of the external pharynx, at 19 weeks - 1 cm above the external pharynx, soon...
marginal attachment of the placenta
marginal attachment of the placenta. It was discovered yesterday on an ultrasound. I met a doctor in the corridor, she was in a hurry, but she said that this was not very good and to keep me sexually rest for now...
Short neck and low presentation
I visited Dr. Donov for an ultrasound today. Everything is fine with the baby, I looked at all the organs, measured the bones - everything corresponds to the deadline, without pathologies. But, here, he measured my cervix 3.7 cm long and the lower edge of the placenta at the level of the internal os:(((He says I need to put stitches. Who has already encountered this? Is this really so necessary and how does this procedure go?
Placenta location and cesarean section.
Placenta location and cesarean section.. Medical issues. Pregnancy and childbirth. Placenta previa. Pregnancy and childbirth: conception, tests, ultrasound, toxicosis, childbirth, caesarean section, birth. But my ultrasound says that I have an anterior placenta...
Placenta previa
Placenta previa. Medical issues. Pregnancy and childbirth. Partial placenta previa - 4 cm from the cervix - share your experience if you have had this (what happens during childbirth).
Regional placenta previa
Regional placenta previa. Ailments, diseases, toxicosis. Pregnancy and childbirth. I was immediately taken to an ultrasound, where they revealed “marginal placenta previa (the placenta is located on the anterior wall), an area of contracted myometrium on the anterior wall in...
Low placenta previa
What is low placenta previa during pregnancy, what threatens the condition of the expectant mother and child - aspects of interest for study.
A low position implies that the amniotic sac is located at a level of less than 7 cm
from the beginning of the cervical canal. There is no overlap of the placenta with the internal cervical os.
This is interesting! What should the thickness of the placenta be by week?
This situation is not considered a contraindication
to natural delivery. Among existing pathologies, it is considered the most favorable for the period of gestation and childbirth.
There is the following classification of low location:
- 1st degree (distance to the cervical canal – 3 cm);
- 2nd degree (there is fixation of the fertilized egg near the beginning of the cervical canal without blocking the entrance);
- 3rd degree (partial or complete overlap is noted, as well as placental displacement along the vault);
- 4th degree (expressed by complete blocking
).
With the first two degrees, natural delivery is possible. The latter degrees require surgical intervention.
Where does the fertilized egg implant
Normally, implantation of the fertilized egg should occur in an area above 3-5 cm from the internal os. Ideally, along the back wall with a transition to the bottom of the uterus. It is these places that are least susceptible to excitability during gestation; there is a special vascular network here, which is necessary for normal nutrition of the fetus and the functioning of the “baby place”.
The fertilized egg “looks” for the most comfortable area for its further development, using some landmarks.
- A developed network of blood vessels. Normally, in the area of the lower segment of the uterus (the transition between the body and the cervix), the vessels do not approach the endometrium as closely as in other parts. But scars after operations (including cesarean section), fibroids, endometriosis, and cervical erosion have a pathological circulatory network. This is a kind of “trap” for the amniotic sac.
- Prepared endometrium. The insufficient degree of maturity of the inner layer of the uterus along the anterior and posterior walls pushes the fertilized egg to implantation in the area of the lower segment. This often happens during atrophic processes in the endometrium against the background of inflammation, with genital infantilism.
In addition, the fetal sac itself (until implantation is in the blastocyst stage) may have developmental abnormalities that lead to implantation near the cervix.
Low placentation during pregnancy means the location of the placenta below 3 cm from the internal os at 18-21 weeks, but each period has its own norms. If the “child’s place” reaches the internal pharynx, this is considered to be a partial presentation, if it overlaps it, it is considered complete. The closer the placenta is to the cervix, the higher the likelihood of a pathological course of pregnancy and childbirth.
The danger of low presentation
Experts often diagnose low placenta previa during pregnancy. What threatens this condition is the main question for pregnant women.
Among the complications that arise against the background of this arrangement, it is customary to highlight:
- The risk of spontaneous abortion
(occurs as a result of partial placental abruption; accompanied by increased tone in the uterine area, systematic bleeding and lack of nutrients). - Decreased blood pressure (accompanied by headaches, dizziness, fatigue).
- Anemia (caused by blood loss; is the root cause of hemorrhagic shock).
- Incorrect attachment of the embryo (response to insufficient space in the lower part of the organ).
- Hypoxia and the risk of delayed development
of the child (impaired blood flow causes a limitation in the oxygen volume and nutrients supplied to the fetus). - The risk of placental displacement during natural labor with the impossibility of normal delivery.
The low location determines the importance of systematic monitoring of the course of pregnancy.
Types of placenta attachment
- Low presentation. The egg is attached 5 cm from the os of the uterus, or even closer to it. However, if an ultrasound showed you this presentation early - in the 2nd trimester - there is a chance that the situation will change for the better by the time you give birth. The baby grows, and the uterine tissues stretch, “migrating” upward. So the placenta has every chance to lie perfectly.
- Partial placenta previa (also incomplete, also marginal). As the name suggests, in this case the uterine os is partially blocked. The above-mentioned bleeding can indicate it, and an ophthalmologist can confirm it. The gynecologist always holds such patients in special regard. If the blood does not “smear”, but is released very intensely, the pregnant woman will be prescribed iron supplements. They will protect the body of the “waiting woman” from anemia.
- Central or complete presentation. This is the most complex pathology. In this case, the internal os is completely “clogged” with the placenta - when examined in the chair, the doctor cannot find the membranes, feeling only the placenta. Its very center is located near the pharynx.
Partial presentation occurs most often - in 75% of women in labor. And this is good, since such a case is not the most dangerous. But more on that below.
Full presentation is a sign that the woman will be admitted to the hospital (even if there is no bleeding). This is a very serious pathology, so the patient needs constant medical monitoring and care.
Caesarean section for pathology
C-section
in case of placenta previa it is carried out if there is:
- anamnesis in the form of diseases with a pronounced inflammatory nature;
- detection of polycystic disease or uterine fibroids;
- previous abortive interruption of the gestation period;
- multiple births
; - pregnancy at a late age;
- early surgical intervention with violation of the integrity of the uterus;
- systematic blood loss in a volume exceeding 0.2 l;
- complete low location of the amniotic sac;
- leg or pelvic
position of the fetus.
The above aspects serve as the basis for planned surgical intervention. If there are no indications for a cesarean section with placenta previa, natural delivery occurs. If there is a threat to the life of the expectant mother or child, emergency intervention is carried out.
What are the prohibitions?
The presence of pathology imposes certain responsibilities on a woman. In order not to harm yourself and your unborn child, it is important to strictly follow all doctor’s prescriptions.
If the pathology is diagnosed, you cannot:
- overload yourself physically, lift weights;
- make sudden movements;
- expose yourself to stress and overwork.
Recommendations: Sex with low placentation is contraindicated in the presence of symptoms such as bleeding, pain, or if there is a threat of miscarriage.