Placenta accreta: what is it?
The placenta is a temporary organ that forms during gestation in the functional layer (called the decidua during pregnancy) of the endometrium. The decidua contains a spongy layer that separates the placenta from the muscular wall of the uterus. In the third stage of labor, the placenta is separated along with the decidua at the level of the spongy layer. There is a contraction of the uterine vessels in the spongy layer, which prevents the occurrence of uterine bleeding. Placenta accreta is caused by the complete or partial absence of the spongy layer and the growth of chorionic villi deep into the uterus and even into nearby organs.
The incidence of pathology has increased 10-fold over the last 50 years. In the 60s of the last century, deep chorionic invasion occurred in one woman in labor out of 30,000 pregnant women; in 2007, the incidence of placenta accreta increased to 1:2500, which was due to an increase in the number of abdominal births.
note
Placenta accreta is often combined with placenta previa, which in turn is explained by lower implantation of the embryo in the presence of a scar on the uterus.
It has been established that the risk of deep chorionic invasion increases by 10% after the first cesarean section, and after the 4th or more operations by 60%.
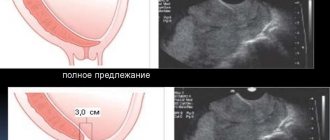
Low placenta previa
What is low placenta previa during pregnancy, what threatens the condition of the expectant mother and child - aspects of interest for study.
A low position implies that the amniotic sac is located at a level of less than 7 cm
from the beginning of the cervical canal. There is no overlap of the placenta with the internal cervical os.
This is interesting! What should the thickness of the placenta be by week?
This situation is not considered a contraindication
to natural delivery. Among existing pathologies, it is considered the most favorable for the period of gestation and childbirth.
There is the following classification of low location:
- 1st degree (distance to the cervical canal – 3 cm);
- 2nd degree (there is fixation of the fertilized egg near the beginning of the cervical canal without blocking the entrance);
- 3rd degree (partial or complete overlap is noted, as well as placental displacement along the vault);
- 4th degree (expressed by complete blocking
).
With the first two degrees, natural delivery is possible. The latter degrees require surgical intervention.
Causes of placenta accreta
Factors that cause pathological ingrowth of chorionic villi are divided into 3 groups:
- Scars on the uterus. Previous surgical interventions and invasive procedures on the fetal place (caesarean section, removal of myomatous nodes, hysteroscopy, surgical abortion, manual separation of the placenta and diagnostic curettage) contribute to the occurrence of local endometrial atrophy and the disappearance of the spongy layer of the decidua. As a result, the chorionic villi come into direct contact with the myometrium and grow into it.
- Diseases of the uterus. The structure of the uterine mucosa is disrupted with the development of an inflammatory process in it (nonspecific and specific endometritis, penetration of hidden sexually transmitted infections), the presence of intrauterine synechiae, submucosal myomatous nodes and endometrioid foci (adenomyosis).
- Increased proteolytic activity of the chorion. In some cases, deep invasion of chorionic villi is caused by a disorder of the enzymatic balance between the embryo and the decidua (the production of hyaluronidase and hyaluronic acid is impaired).
The following factors increase the risk of placenta accreta:
- low placentation, placenta previa (there is no functional layer of the endometrium in the isthmus and cervix);
- multiple births;
- malformations of the uterus (intrauterine septum, changes in its shape: bicornuate, saddle-shaped);
- post-maturity;
- parity (numerous pregnancies and births);
- age (after 35);
- severe gestosis;
- chronic glomerulonephritis.
note
The risk of chorionic villi growing into the myometrium and deeper increases significantly in the presence of a scar on the uterus after previous operations and placenta previa.
Causes and risk factors
Most often, placenta accreta develops as a result of scar changes in the mucous membrane (endometrium) after cesarean section or other surgery. This allows placental vessels to penetrate deep into the uterine wall. In some cases, the causes remain unknown.
Risk factors:
- previous surgery on the uterus (placenta accretion to the scar is more likely the more surgical interventions there were);
- placenta previa, when it partially or completely covers the internal uterine os, or its low location;
- mother's age over 35 years;
- numerous births;
- submucosal fibromyoma with an arrangement of nodes that deform the internal wall of the organ.
Past endometritis, frequent endometrial curettage, developmental defects of the internal genital organs, syphilis, malaria, and glomerulonephritis contribute to the formation of pathology.
Mechanism of formation: true and false placenta accreta
The pathogenesis of the pathology is based on the replacement of the spongy layer by the decidua with connective tissue due to inflammation, dystrophic or cicatricial changes in the uterine wall. Chorionic villi grow into the scar, which makes it impossible to independently separate the placenta from the wall of the fetal sac in the third period. This defect is called tight placenta.
With atrophy (that is, complete or partial absence) of the spongy layer, chorionic villi grow into the decidua and penetrate into the muscular layer of the uterus and deeper, until they grow into neighboring organs. This pathology is called true placenta accreta.
With increased production of hyaluronidase (an enzyme that dissolves the endometrial epithelium) by the chorion, hyaluronic acid (produced in the uterus), which prevents deep germination of chorionic villi, quickly dissolves, which causes pathological deep invasion of the chorion.
What is the placenta attached to: the decidua layer
The embryo enters the uterus at the blastocyst stage. This is no longer just a fertilized egg, but several hundred cells, divided into outer and inner layers. But even the blastocyst is too small to easily attach to the wall of the uterus. This requires special conditions and a “particularly hospitable” internal environment.
That is why, on days 25-27 of the cycle, the endometrium - the inner layer of the uterus - begins to change dramatically. The cells become larger, glycogen accumulates in them - this is the main way our body stores nutritious glucose, which is what the embryo will feed on in the first days after implantation. An increase in the level of the hormone progesterone in the blood, which occurs during successful fertilization, spurs changes in endometrial cells - they form the so-called decidual layer. After implantation of the embryo, it is literally everywhere: between the wall of the uterus and the embryo (basal membrane), around the embryo (capsular membrane) and on the entire surface of the uterus (parietal membrane).
“The last two gradually become thinner and merge with each other as the baby grows, but the basal membrane, located under the placenta, grows, thickens and becomes two-layered. A compact layer (stratum compactum) faces the inside of the uterine cavity, in which the excretory ducts of the glands pass. Behind it is a spongy (porous) layer (stratum spongiosum), which consists of many hypertrophied glands.
The basal decidua is not smooth: by the third month of pregnancy, outgrowths-septa (septa) appear on it, which form peculiar “cups” where maternal blood flows. The chorionic villi are immersed in these cups (the chorion is the embryonic part of the placenta, and its villi are structures formed by the blood vessels of the fetus). They seem to “line” the cups from the inside.
Classification
The pathology is systematized based on the following criteria: the area of placenta attachment and the depth of its germination into the uterine layers. There are several types of abnormal growth of the chorion:
- False, dense or intimate accretion (attachment of the placenta) - placenta adhaerens. The most favorable and common option. It is formed due to cicatricial deformation of the spongy layer. Chorionic villi grow quite tightly into the decidua, penetrating the basal layer of the endometrium, but without damaging the myometrium. Separation of the placenta does not occur in the third stage of labor; manual removal is required.
- True increment. Caused by the disappearance of the spongy layer. There are three subtypes of pathology:
- placenta accreta (accreta placenta) – the spongy layer is absent, chorionic villi reach the uterine muscle, but grow into it, observed in 78% of all cases of true accreta;
- placenta increta (ingrown placenta) – chorionic villi grow into the muscular layer of the organ and disrupt its structure, occurs in 15% of all cases of pathology;
- placenta percreta (sprouted placenta) - invasion of chorionic villi into the myometrium, serous membrane of the organ and beyond, the frequency of pathology is 7%.
There is also a distinction between complete placenta accreta and incomplete (partial). In the first case, the baby's place is fused to the entire muscular layer of the uterus. In the second case, areas of normal placentation alternate with areas of abnormal chorion invasion.
What are the symptoms and complications of central presentation?
Perhaps the most common symptom of central presentation is vaginal bleeding. This is a complication of placenta previa and its main symptom.
If the presentation is complete, then bleeding usually begins in the second trimester, it occurs periodically and lasts until childbirth. Indeed, as the gestational age increases, the placenta literally fuses with the uterus. The fetus develops, the uterus enlarges, and this is especially noticeable in its lower part - the place where the placenta is attached. Since the placental tissue is almost inelastic, it does not have time and cannot stretch behind the rapidly growing uterus. Therefore, partial placental abruption occurs. The vessels begin to bleed, the contents flow out of the genital tract through bleeding. Sometimes it gives way to spotting. As a rule, this happens the first time when a woman is sleeping or just lying down. However, she does not experience pain at all. This is the distinguishing feature of such bleeding from bleeding during a miscarriage, when severe cramping pain in the lower abdomen is bothersome.
If such bleeding, as a complication of presentation, occurs at 30 weeks, then it can be caused by sex or physical activity, sometimes by an examination by a gynecologist.
Symptoms of complete (central) presentation may include pain in the lower abdomen, lower back, low blood pressure, and uterine tone. Hypotension can be expressed in weakness and drowsiness, dizziness.
Clinical manifestations
The pathology does not manifest itself in any way during the gestational period. Characteristic clinical signs appear in the third stage of labor, when for 30 minutes after expulsion of the fetus there are no signs of separation of the placenta. External signs of child seat separation:
- the umbilical cord protruding from the birth canal does not lengthen; when the placenta separates, the umbilical cord lengthens by 10 cm or more (Alfred’s symptom);
- the fundus of the uterus does not rise above the navel (Schroeder's symptom);
- lengthening of the umbilical cord when straining and retracting it back when relaxing; if the placenta is separated, the umbilical cord does not retract back (Klein's symptom);
- retraction of the umbilical cord on inspiration (Dovzhenko's symptom);
- shortening of the umbilical cord with pressure above the womb (when the placenta is separated, the umbilical cord does not retract).
Complete attachment or growth of the placenta is characterized by the absence of bleeding and signs of separation of the child's place. With partial accretion or when trying to separate the baby's place, with its complete accretion, profuse bleeding from the uterus occurs.
The growth of a child's place into the peritoneum, rectum or bladder is characterized by pain in the lower abdomen and the appearance of blood in the urine/stool.
Important
Profuse uterine bleeding can lead to the death of the woman in labor and requires immediate surgical intervention (hysterectomy). Conservative treatment methods are used as preparation for surgery.
Tight attachment of the placenta: how to determine
Unlike true placenta accreta, placenta accreta is rarely detected by antenatal ultrasound. Suspicion may arise if changes appear in the placenta itself. It is thickened or, on the contrary, thinned (leathery placenta), it has additional lobules, sometimes remote from the main placental site. But more often the obstetrician makes a diagnosis during childbirth if:
within 30 minutes after the birth of the baby there are no signs of placental separation and no bleeding;
blood loss exceeded 250 ml, and there were no signs of placental separation.
” Although it is believed that spontaneous separation of the placenta can be expected within two hours, this rule only applies if there are no signs of bleeding; the loss of 400 ml of blood is considered critical, and the loss of a liter of blood already carries the risk of developing hemorrhagic shock.
If the placenta does not separate, the obstetrician has two tasks. First, understand whether the placenta is still attached to the wall of the uterus or simply cannot leave its cavity. There are a number of clinical tests for this. If the placenta is still attached to the wall of the uterus, then:
Alfeld's sign - the outer part of the umbilical cord does not lengthen;
Dovzhenko's sign - the umbilical cord is retracted into the vagina with a deep breath;
Klein's sign - the umbilical cord lengthens when straining, but after pushing it retracts back;
Küstner-Chukalov sign - when pressing with the edge of the palm on the abdominal wall slightly above the pubis, the umbilical cord does not retract into the vagina, but, on the contrary, comes out even more.
Secondly, the doctor must determine whether this is a true placenta accreta, which was not noticed during prenatal care, or a false one. Unfortunately, this is only possible when attempting to manually separate the placenta.
Diagnostics
Ultrasound diagnostic methods allow identifying pathology:
- Ultrasound scanning of the uterus and fetus. It is possible to detect deep chorionic invasion at 18–20 weeks. The detection of cysts and hyperechoic areas in the child's place, the absence of an intermediate layer (spongy) between the tissue of the placenta and the myometrium, visualization of placental lacunae, the thickness of the uterine muscle less than 1 mm at the placenta localization indirectly indicate placenta accreta.
- Color Doppler karyotyping. Allows you to determine the location of pathological vascular zones. A characteristic sign is the detection of an enlarged subplacental complex of veins. Allows you to assess the depth of invasion of chorionic villi into the muscular layer of the uterus. It is considered the gold standard in prenatal diagnosis of pathology.
If placenta accreta is suspected in doubtful situations, MRI pelviometry is performed. The method makes it possible to evaluate the uterine wall (roughness, heterogeneity of the myometrium and placental tissue). Additionally, determination of the level of alpha-fetoprotein is prescribed (for pregnant women at high risk). An increase in AFP indirectly indicates the presence of placenta accreta.
Differential diagnosis between true accretion and intimate attachment of placenta is carried out in the third stage of labor. When manually separating the placenta, the tightly attached placenta can be separated; to stop the bleeding, the uterus is massaged on the fist. With true increment, it is impossible to manually separate the placenta. The pathology is also differentiated from uterine hypotension, disseminated intravascular coagulation syndrome, blood diseases and a normally attached baby's place in the tubal angle with a malformation of the uterus.
Location options
The location of attachment largely depends on which part of the uterus the fertilized egg was implanted in. But this is not the final version. Until complete formation has occurred, the chorion is able to migrate in search of more suitable conditions. Also, the change in the position of the fetal place is determined by the nature of the growth of the uterus: its tissues gradually stretch and carry the placenta with them.
The location along the posterior wall closer to the fundus of the uterus is considered normal. Less common are attachments on the side walls. Low placentation is a condition when the distance from the edge of the placenta to the internal os of the uterus is less than 6 cm. The baby's place in this situation is located along one of the walls of the uterus. If it is attached to the back surface, it is still capable of migrating higher. With placentation along the anterior wall, the prognosis is unfavorable. As the uterus enlarges, the organ moves not upward, but downward, and can block the internal os.
Dynamic ultrasound provides evidence of the migration of a temporary organ. When examined in the early stages, the incidence of low placentation is ten times higher than before birth.
Of particular danger is low placentation, which has developed into placenta previa. In this case, there are several types of position of the fetal place:
- marginal - the baby's place is attached at the border of the internal pharynx;
- partial - the temporary organ somewhat overlaps the internal pharynx;
- complete - the baby's place completely covers the exit from the uterus.
Low placentation is not a threatening condition. If you follow your doctor's recommendations, complications rarely occur.
Complications
Violation of placental attachment is often combined with congenital anomalies of fetal development, which are not the cause of blastogenesis disorders. The gestational period in women with this pathology is complicated by fetoplacental insufficiency, hypoxia and malnutrition of the fetus, and premature aging of the placenta. During childbirth, placenta accreta is fraught with the occurrence of profuse uterine bleeding, leading to hemorrhagic shock and death of the woman in labor. Rare complications of this anomaly include disseminated intravascular coagulation syndrome, air embolism of large vessels, and respiratory distress syndrome in the fetus.
Treatment for placenta accreta
Therapeutic tactics are determined by the type of abnormal deep chorionic invasion. If true placenta accreta is detected during pregnancy, the woman undergoes a planned cesarean section at 37–38 weeks, followed by a hysterectomy. If pathology is detected during childbirth, emergency hysterectomy is performed.
When the placenta is tightly attached, under intravenous anesthesia, it is manually separated from the wall of the uterus (with one hand the obstetrician fixes the uterus through the anterior wall of the abdomen, with the other he makes sawing movements, separating the placental tissue and the uterine wall). After removing the placenta and examining it, the doctor, without removing his hand from the uterine cavity, removes clots and fragments of membranes from it, then massages the uterus with his fist to stimulate contraction of the organ. After labor is completed, uterotonics, hemostatics, antibiotics, and, if indicated, infusion therapy and blood transfusion are prescribed.
For true placenta accreta, hysterectomy is indicated. The scope of the operation (supravaginal amputation of the uterus or its extirpation depends on the location of the placenta). In case of low placentation or placenta previa, hysterectomy is performed. In case of invasion of chorionic villi into the bladder or rectum, a combined surgical intervention (uro- or proctogynecological) is performed, the purpose of which is to completely remove the placental tissue. Preoperative preparation in emergency cases (detection of pathology and bleeding in the third stage of labor) includes intravenous infusions, including donor blood, administration of hemostatic and contracting drugs, maintenance of vital functions (blood pressure, heartbeat).
What does central placenta previa mean during pregnancy and what does it affect?
With the onset of pregnancy, a woman must undergo an ultrasound examination. In conclusion, this study indicates how the future baby and placenta are located in the uterus. And if it talks about placenta previa, then the woman has something to think about.
Briefly about placenta previa
The placenta is an organ in a woman’s body that appears only during pregnancy. It serves as a connecting link between the body of the expectant mother and her baby. The placenta provides nutrition to the fetus and its respiration, and removes metabolic products. Placental tissue also produces hormones that are necessary for the healthy course and development of pregnancy.
Normally, the placenta is located at the bottom of the uterus - that part of it that remains almost unchanged. If this organ is located on the side of the pharynx, then doctors note presentation. Placenta previa is a pathology of its attachment and development in a place that does not ensure a healthy and optimal course of pregnancy. Presentation may be partial. In this case, the os of the uterus is covered by the placenta by a third or two thirds. Complete presentation is when the center of the placenta is completely aligned with the os of the uterus. It is also called central presentation. Medical statistics show that complete presentation is 5 times less common than incomplete presentation.
In the case of incomplete presentation, that is, lateral or marginal, there are chances of the placenta spontaneously shifting to the desired area closer to birth. In the case of complete (central) presentation, this option is completely excluded.
Prognosis and prevention
Preservation of a woman’s health is ensured by antenatal detection of pathology, planned delivery, adequate management and treatment in the postpartum period. When the placenta is intimately attached, the prognosis for childbirth and the woman’s health is favorable. Performing a hysterectomy deprives the patient of the ability to bear a child.
Primary prevention measures include: gestational planning, avoidance of abortions and unnecessary intrauterine manipulations, timely treatment of endometritis and latent sexually transmitted infections, and cesarean section according to strict indications.
Sozinova Anna Vladimirovna, obstetrician-gynecologist
just today
( 50 votes, average: 4.56 out of 5)
31 weeks of pregnancy: fetal development, height and weight, well-being of the expectant mother
Karyotyping of spouses: what is it, preparation for analysis
Related Posts
Depending on the degree of penetration of chorionic villi into the layers of the uterine wall, they are distinguished:
1) Excessively tight attachment of the child seat (placenta adhaerens);
2) True placenta accreta (placenta acreta, increta et percreta).
Intimate attachment (excessively tight attachment) of the placenta
is a pathology in which the chorionic villi do not extend beyond the compact layer of the falling membrane, but are excessively tightly connected to it.
True placenta accreta
is a severe pathology in which chorionic villi penetrate the muscular layer or, growing through it, reach the serous membrane of the uterus. The true increase in a child's place can be complete or partial. With complete accretion, the entire maternal surface of the placenta is firmly connected to the wall of the uterus, but with partial accretion, only the surface of individual lobules. This pathology is very severe and occurs relatively rarely: once per 0 births.
Etiology.
Pathology occurs when there are changes in the uterine wall, changes in the placenta itself, or when the enzymatic (proteolytic) ability of the chorion is impaired. Changes in the uterine wall are facilitated by: previous inflammatory processes (metroendometritis), scars on the uterus (after surgery, curettage of the uterine walls during abortion), tumors of the uterus (submucosal fibroids), and malformations of the uterus.
The occurrence of degenerative processes in the placenta is facilitated by: chronic infections, toxicosis, post-term pregnancy. The increased proteolytic ability of the chorion can lead to the ingrowth of villi into the compact layer of the falling membrane as a whole, and in some cases to growth into the muscular layer of the uterus up to the serous membrane.
Clinic.
With complete placenta accretion to the uterine wall, there is no bleeding, since the vessels over the entire area of placenta accreta are not injured. This clinical situation occurs without bleeding and is manifested by the absence of signs of separation of the placenta.
With intimate attachment or partial true placenta accreta, when one part of it is tightly attached to the wall of the uterus, and the other is exfoliated, the symptom of heavy bleeding is mandatory.
Obstetric tactics.
If the placenta is too tightly attached (there is a symptom of bleeding and there are no signs of separation of the placenta), it is necessary to perform manual separation and release of the placenta.
If there is no symptom of bleeding and conservative measures are ineffective, wait 10-15 minutes, after which the placenta should be manually separated. When trying to separate the placenta from the uterus when it is completely and truly enlarged, heavy bleeding immediately occurs. In such a situation, immediate surgery is necessary: transection and supravaginal amputation of the uterus.
With partial true accretion of the placenta, an attempt to separate the placenta by hand further intensifies the bleeding. It is necessary to perform an operation of transection and removal of the uterine body. At the same time, measures are taken to combat hypovolemia, anemia, and infection.
• Bleeding in the early postpartum period.
Bleeding from the genital tract that occurs in the first 4 hours after the birth of the placenta is called bleeding in the early postpartum period. It appears for three reasons: 1) when parts of the baby’s place are retained in the uterine cavity, 2) when there is atony or hypotension of the uterus, 3) when there is injury to the soft tissues of the birth canal.
• Hypotonic bleeding.
Uterine hypotension is a decrease in the tone and contractility of the uterus. Under the influence of measures and means that stimulate the contractile activity of the uterus, the muscles of the uterus contract, although often the strength of the contractile reaction does not correspond to the force of the impact. With uterine atony, drugs that stimulate the uterus do not have any effect on it, the neuromuscular apparatus of the uterus is in a state of paralysis, uterine atony is rarely observed, but causes massive bleeding.
Etiology.
1) depletion of the body’s strength, the central nervous system as a result of prolonged painful labor, persistent weakness of labor;
2) late toxicosis (nephropathy, eclampsia)
3) hypertension
4) anatomical inferiority of the uterus: underdevelopment and malformations of the uterus, uterine fibroids, scars on the uterus after operations, past inflammatory diseases or multiple abortions;
5) functional inferiority of the uterus: overdistension of the uterus due to polyhydramnios, large fetus, etc.;
6) presentation and low attachment of the placenta.
7) a combination of several reasons.
Clinic:
The main symptom is massive bleeding from the postpartum uterus, and hence hemodynamic disturbances, hemorrhagic shock, and disseminated intravascular coagulation syndrome. Blood flows out of the uterus continuously, with clots. The severity of the condition depends on the strength, duration of bleeding and the general condition of the woman at the onset of bleeding. Physiological blood loss should not exceed 100-150 ml, the maximum permissible is 0.5% of a woman’s body weight. If the postpartum woman’s body’s strength is depleted, the body’s reactivity is reduced, then even a slight excess of the physiological norm of blood loss can cause a severe clinical picture. The severity of the clinical picture also depends on the intensity of bleeding: for example, with large blood loss (1000 ml. hour more) for a long time, the symptoms of hypovolemia are less pronounced and the woman copes with this condition better than with rapid blood loss of the same or even less amount of blood, when Collapse and death may occur faster.
•Diagnosis
is established based on the symptom of bleeding from the uterus and objective data on the condition of the uterus:
On palpation, the uterus is large, relaxed, and sometimes poorly contoured through the anterior abdominal wall.
• Differential diagnosis.
In the early postpartum period, hypotonic bleeding should be differentiated:
1. With traumatic damage to the birth canal, with trauma to the birth canal, the uterus will be dense, well-contracted; when examining the cervix and vaginal walls using mirrors, the diagnosis of traumatic damage to soft tissues and bleeding from them is confirmed.
2. Defect of placenta.
3. Coagulopathy.
•Features of obstetric bleeding:
I. Suddenness.
2. Fast.
3. Massiveness.
4. The apparent volume of blood loss does not always correspond to the true one.
5Rapid increase in complications and decompensation.
6. Inadequacy of the severity of complications and the speed of their development to the volume of blood loss.
7. Occur against the background of changes in the hemostatic system characteristic of pregnancy.
* Principles of treatment.
1. Timeliness of measures to combat bleeding.
2. Adequacy of therapeutic measures to the volume of blood loss.
3. Staged (carried out in a strictly defined order, according to indications).
4. Simultaneous implementation of measures to stop bleeding and combat complications,
5. Do not repeat ineffective measures.
6. Pathological blood loss is replenished with an adequate volume of transfusion media.
7. Compliance with all indications, principles, rules and technical features of all applied operations, including blood transfusions.
8. Almost all measures to combat bleeding relate to surgical methods, therefore, strict indications are required for the use of each of them.
• Measures to stop bleeding.
1. Emptying the bladder with a catheter.
2. External massage of the uterus: through the anterior abdominal wall, the fundus of the uterus is covered with the palm of the right hand and circular massaging movements are performed without using force.
3. Uterotonics (1 ml of oxytocin or methylergometrine intravenously). If during the massage the uterus does not contract or contracts and then relaxes again, then proceed to further measures.
4. Infusion therapy begins immediately after the maximum permissible blood loss is exceeded.
5. Cold on the hypogastric region.
6. Swab with ether into the posterior fornix.
7. For blood loss over 400 ml. - manual examination of the uterine cavity and external-internal massage of the uterus. After the corresponding misinformation. treatment of the external genitalia of the postpartum mother and the hands of the obstetrician under general anesthesia under aseptic conditions (Okinczyc sleeve) with a hand inserted into the uterine cavity, examine the walls of her day to exclude the presence of trauma and retained remnants of the placenta, remove blood clots, especially parietal ones, which prevent uterine contraction. They massage it on the fist, the fist comes into contact with the bottom of the inner surface of the uterus, and with the other hand they massage the uterus through the anterior abdominal wall. As the tone increases, the arm is tightly covered by the muscle of the uterus, and bleeding stops. The hand is removed from the uterine cavity. Rough, forceful massaging of the uterus is unacceptable, as it can cause multiple hemorrhages in the uterine muscle.
8. For blood loss over 500-600 ml, component blood transfusion.
9. Genter's method is to create a Trendelenburg position; then - squeeze the lower segment with the fingers of one hand and with the same hand press the lower segment to the spine, pressing the aorta.
10. Electrical stimulation of the uterus, cryogenic metrohemostats.
11. If blood loss exceeds 700-800 ml, clamping of the uterine vessels:
• according to Baksheev, a pair of bilateral T-shaped soft clamps are applied to the cervix, inserting one branch into the uterine cavity and placing the other in the lateral fornix of the vagina. When the instruments are closed, the uterine arteries in the area of the parametrium are clamped on both sides and the bleeding stops;
• according to Henkel-Tikanadze, clamps (intestinal clamps or Collen forceps) are applied to the parametriums on both sides through the lateral vaults of the vagina, lowering the cervix as much as possible;
• according to Quantiliani, several clamps (bullet forceps) are applied to the cervix, connecting the anterior and posterior lips, after which the cervix is lowered from the vagina and bent anteriorly.
12. For blood loss over 1000-1200 ml. if there is no effect from one of the listed methods, transection to radically stop bleeding. The lack of effect allows us to make a diagnosis of atonic bleeding, requiring surgical intervention on the uterus: hysterectomy, i.e. removal of the entire uterus (with the cervix).
Numerous described methods of stopping bleeding: applying a suture to the posterior lip of the cervix (according to Lositskaya), pressing the aorta in the abdominal region with fingers (according to Biryukov) or a fist, Momburg tourniquet, Piskachek’s method, Arendt’s method, etc. cannot be used to the extent listed above. in practice. Hypotonic bleeding differs primarily in intensity, and the use of all of these methods leads to loss of time, an increase in the volume of lost blood and the risk of developing hypofibrinogenemic complications.
Tamponade with a bandage of the uterine cavity according to Dursen is contraindicated. Ligation of the uterine vessels is also not used during laparotomy.
• Prevention of bleeding in the early postpartum period.
Prevention of bleeding in the early postpartum period should be carried out during pregnancy: identification and hospitalization in an obstetric hospital 2 weeks before. before birth of pregnant women with anatomical and functional inferiority of the uterus, with placenta previa, early detection and timely treatment of late toxicosis, proper management of labor and the early postpartum period, pain relief, administration of oxytotic agents, 40% glucose solution and 10% gluconate solution or calcium chloride.