What is breech presentation
In the early stages of pregnancy, the baby is still so small that it moves freely in the uterine cavity and can occupy any position there.
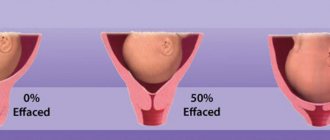
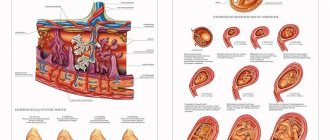
However, over time, the baby grows and his movements in the uterus become more limited. Thus, by approximately the 28th–30th week of pregnancy, it occupies a certain position - as a rule, longitudinally with the head down. This position of the baby is called cephalic presentation. Normally, a baby is born head first. But sometimes a situation arises when the child’s buttocks or legs are installed above the entrance to the pelvis towards the end of pregnancy. In this case, they speak of breech presentation of the fetus. The incidence of this complication varies between 2.7–5.4%. There are several types of breech presentation of the fetus:
- purely gluteal (the buttocks of the fetus are installed above the entrance to the small pelvis, with the legs bent at the hip joints, straightened at the knees and extended along the body);
- mixed gluteal (buttocks present with one or two legs bent at the hip and knee joints);
- leg (full - both legs are presented and incomplete - one leg is presented).
The most common is pure breech presentation (about 65% of cases).
Often during childbirth, a transition from one type of breech presentation to another may occur. Pure breech presentation is more often observed in primiparous women, mixed breech and leg presentation in multiparous women, which is associated with a decrease in the muscle tone of the uterus and anterior abdominal wall: the fetus has the ability to move more. It has been noted that breech presentation in multiparous women occurs approximately 2 times more often than in primiparous women.
Risk factors for breech presentation
There are a number of factors that can contribute to the occurrence of breech presentation:
- narrow pelvis;
- abnormal shape of the pelvis (for example, after suffering from rickets in childhood);
- malformations of the uterus (saddle-shaped, bicornuate uterus, presence of a septum in the uterus);
- uterine fibroids (benign tumors) and tumors of the uterine appendages;
- placenta previa (the placenta partially or completely blocks the exit from the uterine cavity). In this and other conditions listed above, the normal position of the fetus is disrupted, the head cannot take the correct position due to the presence of an obstacle and it is more convenient for the child to position his buttocks down;
- excessive mobility of the child with polyhydramnios or limited mobility with oligohydramnios, multiple births;
- pathological hypertonicity of the lower segment of the uterus and decreased tone of its upper sections. In this case, the fetal head, as the largest and densest part of the body, is pushed away from the entrance to the pelvis and takes a position in the upper part of the uterine cavity. Such disturbances in the contractile activity of the uterus in the third trimester of pregnancy can be caused by dystrophic changes in the myometrium due to inflammatory processes, repeated curettage, multiple pregnancies and complicated childbirth;
- malformations of the fetus (for example, hydrocephalus - an excessive increase in cerebrospinal fluid in the cranial cavity, when the enlarged head is too crowded in the lower segment of the uterus and the fetus turns down with the pelvic end). In addition, it was noted that those patients who were themselves born in a breech presentation often experience a similar situation during their own pregnancy. These facts may indicate a hereditary predisposition to breech presentation. However, this issue requires further study.
Possible complications of breech presentation
Birth in breech presentation is longer, which can result in various complications that cannot always be foreseen and prevented. In modern obstetrics, breech birth is considered pathological due to the high number of complications for the mother and fetus.
Untimely rupture of amniotic fluid (early or premature) before the complete opening of the cervix occurs due to the absence of a belt of contact between the bony pelvis and the presenting pelvic end of the fetus (this is especially common with foot presentation). In cephalic presentation, this function is performed by the head: pressing against the bones of the pelvis, it divides the waters into anterior and posterior. Overflow of the fetal bladder with communicating anterior and posterior waters leads to rupture of the membranes, and the waters pour out either before the onset of labor or until the cervix is fully dilated. In order to prevent early opening of the membranes, the woman in labor must observe bed rest. It is recommended to lie on the side towards which the back of the fetus is facing, this ensures a gradual, slow opening of the cervix, eliminating the pressure of the presenting part on the cervix.
Another complication is associated with untimely discharge of water - prolapse of umbilical cord loops, which can lead to hypoxia (oxygen starvation) of the fetus and even its death. The risk of umbilical cord prolapse depends on the type of breech presentation and occurs 5 times more often than with cephalic presentation. After the rupture of amniotic fluid, it is mandatory to conduct a vaginal examination to diagnose this complication. If the umbilical cord cannot be tucked in (this happens with breech presentation), a caesarean section is performed.
Another common complication is weakness of labor. Many factors of breech presentation predispose to this: insufficient pressing of the soft tissues of the birth canal and uterus by the pelvic end of the fetus to the woman’s bony pelvis, lack of proper reflex irritation, as well as untimely outpouring of water. Weakness of labor forces and premature rupture of amniotic fluid can lead to protracted labor, a long anhydrous interval, infection of the fetus and mother. In order to prevent these complications, childbirth is carried out against the background of regular replenishment of the energy resources of the mother's body with the use of vitamin complexes, antispasmodics, and timely prescription of drug intensification. If there is no effect from the use of birth-stimulating therapy, a cesarean section is performed. In order to prevent secondary weakness of labor, in order to achieve effective pushing in the second stage of labor, drugs that enhance uterine contractions are administered intravenously. The woman in labor is provided with a semi-sitting position and stability of the support points for the arms and legs. Great care is taken when using epidural anesthesia, since it causes relaxation of the pelvic floor muscles and thereby reduces the force of pushing.
The mechanism of birth itself during breech presentation presents a high probability of fetal hypoxia. Breech presentation is characterized by a physiological increase in fetal heart sounds during labor, caused by irritation of the visceral nerve due to the pressing of a limb to the fetal body. Violation of the fetal cardiac activity may be associated with compression of the umbilical cord and placenta by the fetal head located in the fundus of the uterus. The likelihood of fetal hypoxia occurs after its birth to the umbilical ring, because inevitably, the umbilical cord is pressed first by the shoulder girdle, and then by the fetal head to the bone ring of the entrance to the pelvis. The fetus can withstand the absence of utero-fetal blood flow for no more than 5 minutes.
When conducting a breech birth, careful monitoring of the condition of the fetus is carried out. A decrease in heart rate to 100-110 beats per minute is considered the initial signs of fetal hypoxia, as well as the passage of meconium (original feces) from the buttocks, which have not yet entered the pelvic cavity. If signs of intrauterine fetal hypoxia are detected at the beginning of labor, a cesarean section is performed. The passage of meconium when the buttocks descend into the pelvic cavity is explained by compression of the fetal intestines by the walls of the birth canal and is not a sign of hypoxia.
Premature expulsion of the fetus due to insufficient opening of the uterine pharynx or pinching of the subsequent head due to spastic contraction of the uterine pharynx is more common with foot presentation, as well as with a decrease in fetal weight (premature birth or intrauterine growth retardation). The reason for these complications is the discrepancy between the large size of the head compared to the small size of the pelvic end. Delayed birth of the head can lead to cranial and spinal injury of the fetus, asphyxia and even death. To avoid such complications, breech birth is carried out under careful monitoring of the woman in labor and the dynamics of cervical dilatation. The woman in labor should strictly follow the recommendations of the medical personnel, and at the end of the second stage of labor, in order to prevent cervical spasm, the woman is given intravenous antispasmodics (ATROPINE, NO-SPA). If necessary, inhalation anesthesia is used.
During the period of expulsion, complicated variants of the mechanism of labor may be observed, caused by a violation of the natural arrangement of parts of the fetus:
Throwing back the arms interferes with the passage of the fetal head through the pelvis.
Excessive extension of the head, which is very rare, is an indication for delivery by cesarean section, because During vaginal birth, there is a high risk of traumatic spinal injury in the fetus. Small extensions of the head, as a rule, are eliminated spontaneously due to contraction of the uterus.
The formation of a posterior view occurs when the back of the fetus turns posteriorly during birth, and the head with the chin can linger under the pubic arch and become pinched. The posterior view of the breech presentation often spontaneously turns into the anterior one during the process of expulsion.
In case of deviation from the typical mechanism of childbirth, the doctor uses special manual techniques for breech presentation.
Impaction of the buttocks into the pelvis is a complication in which the advancement of the fetus along the birth canal stops. It may be associated either with weak labor or with a discrepancy between the sizes of the fetus and the mother's pelvis. Careful monitoring of the nature of labor, the progress of labor, and a correct assessment of the expected weight of the fetus can prevent this complication. A fetus weighing 3600 g or more in a breech presentation is considered large; this estimated fetal weight is an indication for elective surgery.
Too rapid birth of the head without configuration and adaptation to the birth canal, due to the peculiarities of the mechanism of birth in breech presentation, can lead to ruptures of the soft birth canal in the mother, therefore, dissection of the perineum (perineotomy, episiotomy) when erupting the buttocks is mandatory.
Children born in a breech position are considered a high-risk group and require observation by a neurologist. The risk of traumatic injuries to the central and peripheral nervous system increases. Obstetric manipulations during childbirth with breech presentation can lead to fractures of the hip, shoulder, collarbone, and damage to the abdominal organs.
Children born in a breech presentation often experience a pathology that does not depend on the method of delivery. This is dysplasia (underdevelopment) of the hip joint and often torticollis, which is associated with the peculiarities of the position of the fetus in the uterus. Early diagnosis of these disorders and timely treatment give good results.
Also, such children often experience a decrease in muscle tone of the lower extremities, which, as a rule, is temporary.
With a fetal weight of 2500 to 3500 g, the outcome of birth for the fetuses is favorable and does not depend on the method of delivery.
Types of breech presentation
Pure gluteal - the legs of the fetus are bent at the hip joints, the knees are straightened and pressed to the stomach. It occurs in most cases of breech presentation in expectant mothers carrying their first baby.
Leg - one or both hips are extended, the leg is located at the exit of the uterus. It is observed in 25% of cases, more often in multiparous women.
Mixed (gluteal-leg) – the baby’s hips and knees are bent. It is observed in 5% of cases of breech presentation.
Diagnosis of breech presentation
The location of the fetus in the uterus can be determined during a routine external examination by a doctor at the antenatal clinic. With breech presentation, the following signs are determined:
When you feel the abdomen, the fetal head is located in the fundus of the uterus (its upper part) in the form of a dense formation, and the buttocks are located below the entrance to the pelvis (large, irregularly shaped, softer presenting part).
The fetal heartbeat is heard more clearly at the level of the navel and above, in contrast to cephalic presentation, when the heartbeat is heard below the navel.
The nature of fetal presentation is most accurately revealed by ultrasound, during which it is important to establish the type of breech presentation, trace the location of the legs in a breech presentation, determine whether the head is bent or straightened, and what are the features of the location of the umbilical cord. All these data are important in determining further tactics when choosing a method of delivery.
The seam. Aesthetic flaws
There are 2 types of sutures performed during caesarean section:
- Vertical - done during emergency surgery, in case of severe bleeding, fetal hypoxia and multiple pregnancy. Reaches down from the navel to the pubis. It is done in a nodular manner and is very noticeable after surgery.
- Horizontal – performed during planned caesarean section. It is located transversely above the pubis, is done carefully, causes less trauma to the tissue, and does not injure the peritoneum. The cosmetic seam is almost invisible on the body and is easily hidden under underwear.
Methods for correcting breech presentation of the fetus
The final pattern of presentation is formed by the 34th–36th week of pregnancy; before this period, the baby can still roll over. Breech presentation of the fetus up to 28 weeks of pregnancy is the norm and does not require any measures to correct the situation - simply dynamic observation is enough. Turning of the baby onto its head occurs spontaneously before birth in 70% of multigravidas and in 30% of primigravidas with breech presentation.
Naturally
If, during pregnancy over 28–30 weeks, the doctor reveals a breech presentation during examination and it is confirmed at the third screening ultrasound of the fetus (at 32–34 weeks of pregnancy), the pregnant woman is recommended to carry out a set of gymnastic exercises to help turn the fetus onto its head. The essence of all these exercises comes down to creating discomfort in the child in a certain position, after which he strives to take a convenient and comfortable position by turning over.
There are several methods of such exercises:
Methodology of Grishchenko I. I. and Shuleshova A. E.
Exercises are performed before meals 4-5 times a day. It is necessary to lie on the side opposite to the position of the fetus (that is, opposite to the position of the child’s back). Bend your legs at the knees and hip joints. You should spend about 5 minutes in this position, and then straighten your upper leg and, while inhaling, press it to your stomach; while exhaling, straighten your leg, bending slightly forward. These movements must be repeated slowly for 10 minutes. Then you should lie down for 10 minutes without moving on your back, and then take the knee-elbow position for 5-10 minutes. Thus, the child is subject to additional pressure that creates inconvenience, and he tends to turn around in order to get into more comfortable conditions.
Dikan's technique I. F.
Exercises are performed 3–4 times a day. It is necessary to alternately lie on your right and left sides for 10 minutes. You need to change position 4-5 times during the exercise. This technique is well suited for pregnant women with increased uterine tone, since in the lateral position, uteroplacental blood flow improves, the muscles of the uterus relax, and the baby has room to move and the ability to roll over.
"Bridge". You need to lie down on a flat sofa or bed, or on the floor, place a pillow under your lower back so that your pelvis is 20–30 cm higher than your head. You should remain in this position for 10–15 minutes. Performed 2 times a day before meals. During this exercise, the baby's head strongly presses against the fundus of the uterus, creating significant discomfort for the baby, and he tends to turn.
It should be remembered that for all these exercises there are certain contraindications, which include:
- a scar on the uterus (after a cesarean section in a previous birth or other operations on the uterus);
- placenta previa;
- threat of premature birth;
- oligohydramnios;
- polyhydramnios;
- multiple births;
- gestosis (toxicosis of the second half of pregnancy, manifested by edema, increased blood pressure, and the presence of protein in the urine);
- uterine tumors;
- severe maternal concomitant diseases (for example, heart defects, arterial hypertension, diabetes mellitus).
The effectiveness of these exercises is, according to various authors, about 75%.
Obstetrically
In case of ineffectiveness of corrective gymnastics, external rotation of the fetus onto its head has recently become more and more widely used. The use of modern drugs to relax the uterus, performing rotation under ultrasound and cardiac monitoring of the fetus in the absence of contraindications to rotation allows one to achieve very good results.
It is advisable to carry out the rotation after 36 weeks of pregnancy, because by this time, the fetus is considered mature, and if complications arise that require immediate delivery by cesarean section, the prognosis for the newborn is favorable.
If during pregnancy it was not possible to correct a breech presentation to a cephalic presentation, early hospitalization is necessary for a detailed examination and determination of tactics for the most rational management of labor.
Diet after cesarean section.
Principles, products, sample menu for the week
After surgical delivery, a certain diet is prescribed:
- 1st day only still water, up to 1.5 liters;
- Day 2 – low-fat chicken broth, mashed potatoes, no milk or butter, no sweet tea;
- 3rd day – buckwheat or oatmeal unsweetened porridge with water, tea, kefir, steamed coles, boiled vegetables;
- Day 4 – you can stick to the usual diet of a nursing mother, namely:
- eat 5 times a day, half an hour before feeding the baby;
- eat boiled and steamed foods, completely exclude fried foods, onions, all products containing preservatives and food additives, lemonade, sweets;
- 50% of the diet should be dairy and fermented milk foods;
- eat lean pork, beef, rabbit, veal, cod, hake, perch;
- Buckwheat, oatmeal, millet, and pearl barley porridge, cooked in water, without adding oil, are allowed;
- Be sure to drink 1.5-1.6 liters. daily (still water, unsweetened tea, diluted compote, fruit juice, homemade).
The diet is designed taking into account the fact that the child’s gastrointestinal tract is not fully formed. It is not recommended to eat brightly colored foods that can cause diathesis. It is necessary to include as many vegetables and coarse fiber into the menu as possible to normalize intestinal function after surgery.
After 3-4 months, the menu is gradually expanded, strictly monitoring the baby’s body reaction.
Diet for the week:
1st day:
- Breakfast - buckwheat, toast, milk;
- 2nd breakfast – cottage cheese casserole, stewed apple;
- Lunch – fish soup, boiled chicken breast with carrots, compote;
- Afternoon snack – banana, cookies;
- Dinner – steamed hake with potatoes, tea;
- At night - yogurt.
Day 2:
- Breakfast - oatmeal, dried bread, tea;
- 2nd breakfast – walnuts, dried apricots, banana;
- Lunch – zucchini soup, chicken meatballs with stewed carrots, apple compote;
- Afternoon snack – baked apples with honey;
- Dinner – fish cutlets with vegetables, tea;
- At night - kefir.
3rd day:
- Breakfast – buckwheat, sandwich with cheese;
- 2nd breakfast – fruit puree, cottage cheese;
- Lunch – pearl barley soup, chicken meatballs, herbal tea with fennel;
- Afternoon snack – compote, cookies;
- Dinner – steamed veal with vegetable side dish, tea;
- At night - acidolact.
4th day:
- Breakfast – millet porridge, bread with butter, milk;
- 2nd breakfast – cottage cheese soufflé, compote;
- Lunch – vermicelli soup, boiled perch with potatoes, fruit juice;
- Afternoon snack – biscuits, tea;
- Dinner – beef with pasta, herbal tea with mint
- At night - organic yoghurt
Day 5:
- Breakfast - oatmeal, cheese sandwich, milk;
- 2nd breakfast – cottage cheese with sour cream, herbal infusion;
- Lunch – chicken soup, veal with buckwheat, compote;
- Afternoon snack – banana, milk jelly;
- Dinner – boiled perch with stewed zucchini, fruit juice;
- At night - fermented baked milk.
Day 6:
- Breakfast – pumpkin porridge, cheese, milk;
- 2nd breakfast – baked apples, compote;
- Lunch – pearl barley soup, steamed lean pork meatballs with boiled carrots, fruit juice;
- Afternoon snack – biscuits, herbal tea with fennel;
- At night - acidolact.
Day 7:
- Breakfast – noodles with milk, toast with cheese, tea;
- 2nd breakfast – cottage cheese dumplings, compote;
- Lunch – soup with dumplings, steamed rabbit meatballs with potatoes, fruit juice;
- Afternoon snack – cookies, acidolact;
- Dinner – steamed cod with vegetables, tea;
- At night - kefir.
To the hospital before giving birth
Upon reaching 38–39 weeks, all pregnant women with breech presentation are advised to undergo prenatal hospitalization in a hospital. An in-depth examination of the pregnant woman is carried out there:
- Ultrasound to determine the type of presentation (pure breech, mixed breech or leg), the degree of extension of the head (normally the fetal head is bent and the chin is pressed to the chest, extension of the head can complicate its birth), the size of the fetus;
- according to indications (for example, if a large fetus is expected) - X-ray pelviometry (accurate determination of the size of the pelvis using computed tomography or magnetic resonance imaging);
- assessing the condition of the fetus using cardiotocography - studying the fetal heartbeat and uterine tone, conducting a non-stress test (studying the reaction of the fetal cardiovascular system in response to its movements: with physical activity, the heart rate increases);
- assessment of a woman’s body’s readiness for childbirth.
Based on the results of the examination, the prognosis of labor and the choice of obstetric tactics for its management are determined. During the examination, pregnant women are divided into 3 groups according to the degree of risk of the upcoming birth for the fetus.
Group I includes high-risk pregnant women:
- estimated fetal weight more than 3600 g – large fetus;
- narrowing of the pelvis;
- chronic hypoxia (lack of oxygen) of the fetus;
- extragenital (not related to pregnancy) diseases affecting the condition of the fetus and labor, for example arterial hypertension, diabetes mellitus, renal failure;
- primigravidas over 30 years of age.
These pregnant women usually undergo a elective cesarean section.
Group II includes pregnant women who may develop complications during childbirth (for example, with a low placenta, entanglement in the umbilical cord, rapid labor in the past). Childbirth in this group must take place under mandatory intensive monitoring of the state of labor and the fetal heartbeat. If complications arise during childbirth, a caesarean section is performed.
Group III includes low-risk pregnant women. Their birth is carried out with usual supervision. This includes women under 30 years of age without serious chronic diseases, an estimated fetal weight of up to 3600 g, normal pelvic dimensions and satisfactory fetal condition according to CTG and Doppler measurements (a method for studying utero-fetal-placental blood flow).
Contraindications
Contraindications are associated with the danger of an inflammatory process in a woman’s body:
- sudden or aggravated chronic diseases such as pyelonephritis, cholecystitis, pneumonia;
- inflammatory process in the female genital organs;
- acute viral diseases, influenza, ARVI;
- labor lasts more than 24 hours (normally no more than 12 hours);
- frequent, more than 3 times examination of the vagina during childbirth.
- failed attempt using obstetric forceps;
- intrauterine infection, asphyxia and fetal deformity, severe hypoxia, in which there is no confidence in preserving the life of the child.
If there are concerns about the baby's viability, an operation is performed to remove the fetus along with the woman's uterus, or, if possible, an extraperiotanal cesarean section, which consists of temporary isolation of the abdominal cavity, and allows the removal of the dead fetus and preservation of the uterus.
Indications for surgery
The absolute indications for performing a planned caesarean section are:
- extragenital diseases that require the exclusion of attempts (for example, heart defects, including operated ones, threatening retinal detachment, etc.);
- severe disturbance of fat metabolism (obesity of the 2nd degree and higher);
- pregnancy after IVF;
- post-term pregnancy (pregnancy 42 weeks or more);
- malformations of the internal genital organs;
- narrowing of the pelvis;
- scar on the uterus;
- estimated fetal weight less than 2000 g or more than 3600 g;
- placenta previa (situations when the placenta partially or completely covers the internal os of the cervix);
- cicatricial changes in the cervix;
- multiple pregnancy (breech presentation of the first fetus located closer to the entrance to the pelvis). In other cases, cesarean section is performed according to a combination of indications (for example, the age of the expectant mother is over 30 years, complications during pregnancy, chronic fetal hypoxia). The caesarean section rate for breech presentation is 80% or more.
How is the date of a cesarean section determined?
When determining the date of the operation, they take into account the reasons for which a cesarean section is prescribed, the pros and cons for the health of the pregnant woman and the child. The fetus is fully formed at 37 weeks.
For the first, normally ongoing, singleton pregnancy, the doctor prescribes surgery at 39-40 weeks, at the onset of contractions, paying attention to:
- child's weight;
- maturity of the placenta;
- the baby’s readiness for birth—the maturity of the lungs and vital systems;
- general condition of the pregnant woman;
- umbilical cord entanglement and degree of fetal hypoxia.
If two or more children are expected to be born, then the scheduled caesarean section is scheduled for the 38th week, and if the babies share one amniotic sac - at the 32nd week of pregnancy. Having discovered HIV infection, surgery is performed at 38 weeks.
During the second pregnancy, provided that the first birth ended in a cesarean section, the date is chosen at 37-38 weeks.
Doctors do not recommend a third pregnancy, if the previous two ended in surgical delivery, due to the danger of uterine rupture during fetal growth, but if a woman decides to take this risky step, and no complications arise, the baby is removed at 37-38 weeks.
The above calculation is done only for a planned cesarean section; if complications arise during childbirth, an emergency operation is performed urgently.
How will childbirth proceed in a breech position?
The main difference between birth in a breech presentation through the natural birth canal and birth in a cephalic presentation is as follows. The largest part of the fetus - the head - during childbirth in the cephalic presentation, is the first to overcome all the narrow parts of the bony pelvis, being configured by soft sutures and fontanelles. If there is a discrepancy between the sizes of the head and the bony pelvis, then the child simply cannot be born on its own and an emergency caesarean section is performed. If the head has successfully passed all the narrow parts of the pelvis and was born, then the remaining parts of the baby are born without much effort. With a breech presentation, the narrow sections of the pelvis are the first to overcome the baby’s buttocks, which happens quite easily, but when it comes to the head, a discrepancy may arise, which will be critical, and surgical intervention will be required.
During childbirth with breech presentation, the following complications may develop:
- Premature rupture of amniotic fluid (rupture of the membranes before the opening of the cervix by 5–6 cm is considered premature, since until this moment the fetal bladder is involved in the process of opening). This occurs due to the strong pressure of small parts of the fetus on the lower pole of the amniotic sac.
- The loss of small parts of the fetus and the umbilical cord occurs with premature rupture of the membranes and rupture of amniotic fluid due to the lack of tight contact between the pelvic end of the fetus and the lower segment of the uterus.
- Primary weakness of labor occurs at the beginning of labor due to premature rupture of amniotic fluid and insufficient pressure of the pelvic end of the fetus, which is softer than the head, on the cervix.
- Secondary weakness of labor develops during labor due to the fact that the woman in labor becomes fatigued with prolonged labor. It manifests itself as weak contractions, during which the opening of the cervix slows down or stops.
- As the fetal head passes through the birth canal, the umbilical cord may become tightly pressed against the walls of the pelvis. If it lasts more than 5–7 minutes, then fetal death may occur (as oxygen-carrying blood stops flowing to the fetus and severe hypoxia occurs).
- The throwing back of the arms and the extension of the head in the second stage of labor occurs reflexively at the birth of the body.
- Aspiration of amniotic fluid is the entry of water into the baby’s respiratory tract when trying to take a breath when his head is still in the birth canal and has not been born.
- Birth canal injuries and fetal injuries (traumatic brain injury with cerebral hemorrhages) occur when the birth of the fetal head and shoulders is difficult.
Breastfeeding after caesarean section
After surgery, problems often arise with breastfeeding.
Previously, they were considered insurmountable, but now it is quite possible to establish lactation:
- It is necessary to give the baby breastfeeding as early as possible. With epidural anesthesia 30 minutes after birth, if general anesthesia was performed - no later than 6 hours;
- for inflammation, prescribe antibiotics used during breastfeeding;
- refuse bottles and nipples, give the baby only the breast. Supplement with the mixture from a spoon or syringe;
- express milk if it is impossible to feed the baby. This should be done once every 3 hours;
- apply to the breast as often as possible, the baby stimulates the process of milk arrival, in addition, drink tea with fennel or drugs to stimulate lactation;
- feed in a comfortable position. It is best to do this lying down or from under the arm, to avoid injury to the postoperative suture;
- Make sure that when eating, the baby grasps the entire nipple completely, and not just the areola.