Placenta
Information The placenta is a temporary organ consisting of cells from the body of the woman and the fetus. The maternal part consists of the basal part of the decidua, that is, the inner secretory layer of the uterus. And the fetal part of the placenta is formed from cells of the villous chorion (the outer membrane of the fetus). A feature of the structure of the human placenta is the direct contact of maternal blood with chorionic villi.
The placenta performs the following functions:
- Respiratory -
in the placenta, the fetal blood is saturated with oxygen, and carbon dioxide passes to the maternal red blood cells, which transfer it to the lungs and thus remove it from the body. When the blood vessels of the placenta are narrowed and blocked, the fetus receives insufficient oxygen and the baby’s growth and development slows down, and first of all, his brain suffers. - Nutritional –
transfer of nutrients to the fruit for its continuous growth. The diet of the expectant mother should be balanced not only in terms of the content of proteins, fats and carbohydrates, but also rich in vitamins and minerals, because without them the full development of the child is impossible. - Endocrine -
the placenta produces a number of hormones and biologically active substances necessary to maintain pregnancy and normal fetal development. The concentration of human chorionic gonadotropin (HCG), placental lactogen (PL), estriol and progesterone is used to judge the condition of the placenta and possible abnormalities in the development of the fetus. - The function of immune defense is
that the placenta is a barrier that separates two foreign organisms (since the fetus is half composed of the father’s genetic material), and prevents the penetration of fetal antigens into the mother’s bloodstream. If the immune defense fails, severe complications arise (hemolytic disease of the fetus due to incompatibility of the blood of the fetus and mother according to the Rh factor). - The barrier function -
restrictions on the permeability of the placenta for various substances - changes throughout pregnancy and depends on the needs of the fetus. However, alcohol, drugs and toxins (poisons) contained in tobacco smoke easily penetrate the child, damage his cells, cause intrauterine growth retardation and dependence on them.
The placenta begins to form almost immediately after fertilization from the outer membrane of the fetus - the chorion. Part of it becomes covered with villi and is embedded in the mucous membrane of the uterus, where the placenta is formed. The smooth chorion gradually increases and becomes the outer shell of the fertilized egg. Changes also occur in the uterus necessary for the formation of the maternal part of the placenta.
The final structural formation of the placenta is completed by 16 weeks of pregnancy, then it thickens, matures, and from 36 weeks the process of aging begins. Due to various reasons, the normal development of the placenta may be disrupted, and then the following problems arise:
- Placental hypoplasia -
a small placenta, can occur initially -
primary hypoplasia
- is combined with congenital malformations and mental retardation (for example, with Down syndrome).
Under the influence of unfavorable factors, premature aging of the placenta occurs, it shrinks and decreases in size - this is secondary hypoplasia.
In any case, a malnutrition of the fetus occurs and intrauterine growth retardation occurs, but with a initially normal placenta, the development of such complications can be prevented by prophylactic use of drugs that improve placental blood flow. - Placental hyperplasia is
a very large placenta and can occur with diabetes mellitus, severe anemia, hemolytic disease of the fetus, or infectious diseases. An increase in the volume of the placenta occurs due to swelling of the villi. - Thin placenta
– small thickness of the placenta with its normal diameter. There is also a high risk of developing feto-placental insufficiency and fetal growth retardation. Sometimes occurs with congenital anomalies of the fetus, but is not associated with a risk of developing dementia. - Thick placenta
- an increase in thickness up to 5 cm, with normal blood circulation is not a pathology and does not cause any disturbances in the fetus. - A change in the lobular structure of the placenta
- the presence of two, three or a separate additional lobule does not affect the course of pregnancy, but can cause bleeding in the afterbirth or early postpartum period. Retention of one of the placenta lobes prevents normal contractions of the uterus. - Anomalies of placental maturation
- occur more often with insufficient or overweight mother, as well as with
metabolic disorders:
- Uniform accelerated maturation of the placenta
can lead to premature birth. - Uneven accelerated maturation of the placenta
occurs when blood circulation in certain parts of the placenta is impaired and increases the risk of miscarriages, premature births and stillbirths. But with timely detection and treatment, pregnancy ends favorably. - Late maturation of the placenta
often develops in pregnant women who smoke and is combined with fetal malformations.
- Placental infarctions are
areas of dead tissue that occur in severe cases of gestosis and maternal hypertension. If more than 4 of them are detected or one very large one (more than 3 cm), then intrauterine growth retardation may occur. - Placentitis is
inflammation of the tissue of the placenta or fetal membranes (chorioamnionitis). In this case, the risk of intrauterine infection of the fetus and its developmental delay sharply increases. - Tumors of the placenta
can be benign - chorioangioma - proliferation of blood vessels. If its size is small and the fetus is not stolen, then the child develops normally. If the tumor size is significant, blood flow and blood clotting ability are impaired. When a malignant tumor—choriocarcinoma—occurs, excessive growth of the chorionic villi occurs and the death of the fetal egg occurs. Fortunately, this complication is extremely rare.
Additionally, the location of the placenta also has a significant impact on the course of pregnancy.
Normally, it forms on the back or front wall of the uterus, but sometimes it is fixed in the corners, bottom or bottom of the uterus, completely or partially blocking the cervical canal. And then bleeding may occur in the midst of complete well-being, without pain and more often at night. It is urgent to seek help to prevent miscarriage and fetal death. There are many reasons for abnormal attachment, we list the main ones:
- Anomaly of the uterus (bicornuate uterus, presence of an internal septum);
- Large uterine fibroids;
- Dystrophic changes in the uterine wall due to frequent abortions;
- Inflammatory diseases of the uterus;
- Decreased ability of the fertilized egg to penetrate the uterine wall. May occur due to genetic disorders or exposure to adverse factors;
The following types of presentations are distinguished:
- Complete placenta previa -
the placenta completely covers the uterine os. Childbirth through the birth canal is not possible. - Partial -
the placenta obscures part of the exit from the uterus. Unattended childbirth is also not possible.
dangerous There is also a low and marginal location of the placenta, in this case natural childbirth is possible, but the risk of bleeding during pregnancy is high.
Also, the above reasons can cause dense attachment or placenta accreta
, it can be complete or partial. With this complication, the placenta does not separate independently in the third stage of labor, the uterus cannot fully contract and the mother’s condition worsens sharply due to large blood loss.
After the baby is born, the doctor and midwife carefully monitor the mother’s condition and watch for signs of placenta separation. If the placenta and membranes are not delivered within 30 minutes, the woman in labor is given general anesthesia and the placenta is manually separated and released. With true placenta accreta (occurs in 5–7 cases per 70,000 births), when the villi have penetrated into the muscular layer of the uterus, it becomes necessary to remove the uterus.
In accordance with the localization of the fertilized egg in the decidua, three parts can be distinguished:
- lining the uterine cavity (decidua parietalis);
- covering the fertilized egg from the side of the uterine cavity (decidua capsularis);
- located between the fertilized egg and the wall of the uterus (decidua basalis).
The decidua is a nutritional and protective layer for the fetus: its trophic function is mainly carried out in the early stages of intrauterine development, its protective role is most fully manifested by high phagocytic activity. Decidual tissue lyses microorganisms and inactivates their toxins, and also takes part in the synthesis of carbohydrates, lipids and proteins. The synthesis of prolactin and prostaglandins occurs in it. Thus, the decidua plays a very important role in the implantation and further development of the embryo and fetus.
The full-term umbilical cord of a human fetus is a cord, 40-50 cm long with a diameter of approximately 1.5 cm. It lies between the inner (fetal) side of the placenta and the ventral wall of the fetal body. The surface of the umbilical cord is covered with the ectodermal epithelium of the amnion, which in the placenta imperceptibly passes into the amniotic ectoderm covering the inner surface of the placenta, and towards the fetus passes directly into the skin (epidermis) of the surface of the fetus or, rather, the newborn. The place of attachment of the umbilical cord to the ventral wall of the fetal body has a ring-shaped shape (umbilicus, umbilicus). The basis of the umbilical cord stroma is formed by embryonic jelly-like tissue containing a relatively small number of cells, some fibrils and a significant amount of gelatinous ground substance (Wharton's jelly). Rudiments of the umbilical duct and urinary tract of the embryo in the full-term umbilical cord are usually absent. The umbilical cord vessels pass through the stroma of the umbilical cord, namely one umbilical vein, initially laid in pairs, and two umbilical arteries. The umbilical vein (vena umbilicalis) carries oxygenated fetal blood from the capillary network of the chorionic villi of the placenta into the fetal body, while the two umbilical arteries drain oxygen-deprived blood into the placenta. At the site of attachment of the umbilical cord to the placenta, the umbilical vessels first branch in the chorionic membrane into fairly large branches that are visible through the amniotic membrane of the placenta. Smaller branches of these branches then pass into the chorionic villi, forming a capillary network in them.
Fruit shells
Outside, the amniotic sac is covered by a smooth chorion
.
Its inner wall is made up of the amnion -
the water membrane of the fetus; its cells produce amniotic fluid, which is necessary for the mechanical protection of the baby, ensuring its free movement and metabolism. During the first stage of labor, the amniotic sac presses on the cervix, promoting its dilation. The rupture of the membranes usually occurs when the uterine pharynx opens by 5–6 cm. If for some reason attempts began with the fruit membranes intact, they rupture on the head of the born child, they say about this: “born in a shirt.”
Formation and arrangement
The placenta (baby place) is a unique embryonic formation that appears in the uterus during pregnancy. Correct localization of this amazing organ is the key to successful pregnancy and easy childbirth. That is why the location of the placenta during pregnancy is of paramount importance for doctors, and for the expectant mother herself.
The afterbirth, like the fetus, goes through several stages of formation. Doctors monitor its location, growth and movement throughout the entire gestation period. This allows you to timely prevent and eliminate possible complications.
Normally, the attachment site is the area of the fundus or walls of the uterus. As a rule, the afterbirth is located along the back wall.
The location of the placenta is important when it is located in the lower segments of the uterus. This position is called presentation. It can be complete or partial.
The danger of this pathology is that the placenta closes the internal os and prevents the passage of the fetus during delivery. Also, the danger lies in the occurrence of detachment and bleeding with a fatal outcome for the fetus or severe brain hypoxia.
With complete presentation, independent delivery is impossible. Doctors perform surgery without fail.
But at the same time there is one significant advantage. The placenta has one amazing property - it is able to move (migrate) towards better blood supply and nutrition, that is, to the fundus of the uterus. The placenta rises with the growing uterus.
Umbilical cord
Umbilical cord
- an important component of the afterbirth.
Connects the body of mother and baby, providing a constant flow of blood through the vessels. Through the two umbilical arteries,
venous blood flows from the fetus, saturated with carbon dioxide and waste products of the fetus.
Oxygen and nutrients are supplied through the umbilical vein
.
On all sides, the vessels are protected from compression by a special substance - Wharton's jelly
. But it happens that during contractions or pushing the umbilical cord is compressed and blood stops flowing to the fetus. This situation requires increased attention from the doctor and, if necessary, the birth is completed by caesarean section.
When the baby is already born, it is lowered below the level of the uterus to prevent its blood from flowing to the mother. Clamps are then placed on the umbilical cord and cut.
Placenta: structure, functions, maturity, hyperplasia, presentation, detachment
The placenta is not just an organ that connects two organisms. She faces several challenges:
- Respiratory function. Responsible for gas exchange between mother and fetus.
- Trophic, or nutritional. Delivers all the necessary substances for nutrition (protein, water, vitamins, microelements).
- Protective. Protects from the negative effects of the environment and microorganisms, but has a throughput capacity for viruses, toxic substances, poisons and drug molecules.
- Immune function. The organ suppresses the immune conflict of two genetically foreign organisms - mother and fetus.
- Endocrine. The afterbirth produces hormones (estrogen, human chorionic gonadotropin, placental lactogen, progesterone, prolactin and cortisol). It also promotes the transport of hormones from mother to fetus (adrenal, sex and thyroid hormones).
The placenta produces progesterone, human chorionic gonadotropin, and human placental lactogen; only the latter hormone can provide information about the well-being of the placenta. If at a gestational age of more than 30 weeks, upon repeated determination, its concentration is below 4 μg/ml, this suggests a violation of placental function.
The well-being of the fetal/placental axis is monitored by measuring the daily excretion of total estrogens or urinary estriol or by measuring estriol in the blood plasma, since pregnenolone synthesized by the placenta is subsequently metabolized by the fetal adrenal glands and liver, and then again by the placenta to synthesize estriol.
Today, many mothers know far more about pregnancy than our parents knew. Therefore, many women during pregnancy worry about the state of their health, and are very worried if the doctor talks about the condition of such an important organ during pregnancy as the placenta. This organ performs the most important functions, and without it it is impossible to carry a pregnancy to term.
Where is the placenta located and what does it look like?
During a normal pregnancy, the placenta is located in the body of the uterus along its posterior (usually) or anterior wall. It is fully formed by the 15th-16th week of pregnancy; after the 20th week, active metabolism begins through the placental vessels. From 22 to 36 weeks of pregnancy, the weight of the placenta increases, and by 36 weeks it reaches full functional maturity.
In appearance, the placenta looks like a round, flat disc. By the time of birth, the weight of the placenta is 500-600 g, the diameter is 15-18 cm and the thickness is 2-3 cm. There are two surfaces in the placenta: the maternal one, adjacent to the wall of the uterus, and the opposite - the fetal one.
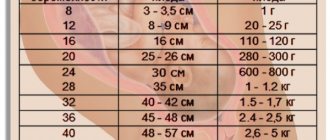
Norms for placental thickness at different stages of pregnancy
Thickness is an important criterion for a woman’s pregnancy. During routine ultrasound examinations, this indicator must be monitored.
Deviations in values, both upward and downward, signal possible pathologies and complications.
Thickness is taken into account to determine the degree of maturity of the “children’s seat”.
The first measurement of this value occurs during a routine ultrasound examination at 20 weeks. The thickness norm at this time falls within the range of 16.7 to 28.6 mm.
Until the 36th week of pregnancy, an increase in thickness occurs. This figure increases by about 1 mm per month.
At 25 weeks, normal is considered to be from 20.3 to 34.0 mm, at 30 weeks from 23.9 to 39.5 mm.
Starting from week 36, it gradually becomes thinner. At 40 weeks of pregnancy, normal thickness ranges from 26.7 to 45.0 mm.