Benefits of the procedure
If we talk about diagnostic laparoscopy, its main advantages are the ability to make a final diagnosis and accurately determine the location of the fetal egg.
Distinctive features of operative laparoscopy will be:
- Minor blood loss during the intervention.
- Less trauma to surrounding tissues, which accordingly reduces the risk of adhesions in the pelvis. Therefore, after laparoscopic surgery, there is a more favorable prognosis for future pregnancy.
- The postoperative period is easier and discharge from the hospital is carried out much earlier.
- Do not forget about the aesthetic side of the issue: with an open operation, a large scar remains, and with laparoscopy - 3 very small scars.
Contraindications for carrying out
It is customary to identify absolute and relative contraindications for laparoscopic treatment of ectopic pregnancy.
dangerous There is only one absolute contraindication - extensive hemorrhage into the abdominal cavity (more than 1.5 liters), accompanied by severe hemorrhagic shock.
The rest will be relative , that is, under certain conditions the doctor can neglect them. These include:
- unstable hemodynamics (blood circulation) with blood loss of more than 500 ml;
- the presence in the past of two or more surgical interventions for pathological processes in the internal genital organs;
- large size of the embryo in the rudimentary uterine horn (an underdeveloped section of the bicornuate uterus);
- the presence of an extensive uterine hematoma with pronounced inflammatory changes in the adjacent tissues;
- combined pathology of the genitals (uterine fibroids, endometriosis);
- rupture of the wall of the fallopian tube;
- localization of the fertilized egg in the interstitial region (the place where the body of the uterus enters the tube);
- obesity (technical difficulties arise).
Process
In general terms, laparoscopic surgery looks like this : most often, under endotracheal anesthesia, 3 punctures are made in the abdominal wall. Gas (usually CO2) is injected into the abdominal cavity to expand the internal organs and improve visibility. Next, a camera is inserted into one of the punctures, which transmits the image to the monitor screen. Various laparoscopic instruments necessary during the operation are inserted into the remaining two holes.
Regarding the treatment of tubal pregnancy, there are the following surgical options :
- Removal (tubectomy).
- Organ-preserving operations.
A tubectomy is performed when there are significant changes in the fallopian tubes (for example, rupture).
Organ-preserving operations:
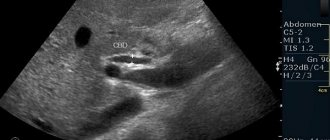
- The most popular is tubotomy - dissection of the fallopian tube. It is performed in case of an undisturbed ectopic pregnancy, if the woman wishes to keep the tube, and also when there is a threat of disruption of the blood supply to the ovary after a tubectomy. Contraindications to the procedure are rupture of the fallopian tube, its gross deformation, the size of the ovum is 3 cm or more, severe anemia due to massive blood loss.
- Removal of a section of the pipe followed by microsurgical restoration of its patency. In recent years, this intervention is performed extremely rarely, since highly effective assisted reproductive technologies have appeared, and microsurgical operations are very expensive and their effectiveness in this case remains questionable.
- Squeezing the fertilized egg out of the tube. This method is not widely used, as it is highly traumatic and has the possibility of bleeding due to incomplete removal of the fertilized egg elements.
Before surgery
In addition to diagnosing and treating gynecological pathologies, laparoscopy of the gallbladder, intestines, stomach and other organs can be performed. Quite often, this method is used to remove one or another organ or part of it.
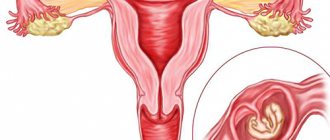
Diagnosing an ectopic pregnancy in the early stages is quite difficult. Signs of an ectopic pregnancy may appear at 4-10 weeks of pregnancy, but do not receive proper attention. It is especially difficult for a pregnant woman to independently determine the presence of abnormalities. Symptoms of an ectopic pregnancy in the early stages cannot be distinguished from the usual common symptoms of a normal pregnancy.
Consequences
important The consequences of surgical laparoscopy appear in the long-term period after the procedure.
Therefore, patients who have undergone this intervention due to an ectopic pregnancy are in dire need of further therapy aimed at restoring menstrual and reproductive function.
More than half of these women experience hormonal and vegetative-vascular disorders, and infertility occurs in a more distant period. I would also like to note that in these patients the risk of recurrent ectopic pregnancy increases, especially if organ-conserving surgery was performed.
How long before you can get pregnant
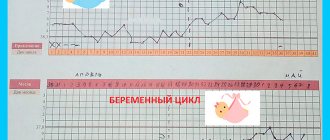
Doctors recommend planning conception after laparoscopy for ectopic pregnancy no earlier than the hormonal levels and functions of the reproductive system are restored. With an uncomplicated operation that preserves the tubes and ovaries, you can begin sexual activity after a month; it is during this period that the menstrual cycle begins. But the time when you can plan a pregnancy is postponed by another month so that the doctor can make sure there are no long-term complications.
If the operation occurred due to a rupture of the oviduct, pregnancy after laparoscopy of the fallopian tubes is postponed by 2-3 months. Even later, doctors recommend planning to conceive a child after removal of the ovary. In this case, it is necessary to take contraceptives (Yarina, Novinet and other hormonal drugs with a therapeutic effect) for 9-12 months. If after repeated examination there are no obstacles to conception, the onset and development of pregnancy will proceed without disturbances.
SOURCES: https://azbukarodov.ru/bolezni-i-oslozhneniya/operaciya-pri-vnematochnoj-beremennosti https://diagnozpro.ru/skopiya/laparoscopy/laparoskopija-pri-vnematochnoj-beremennosti https://borninvitro.ru/ laparoskopiya/laparoskopiya-pri-vnematochnoj/
Alternatives to laparoscopy for ectopic pregnancy
There are two alternatives:
- Carrying out routine surgery.
- Conservative treatment.
As for the first option, everything is quite clear: an incision is made through the anterior abdominal wall, a pathologically altered fallopian tube is found and it is removed.
But if we talk about conservative treatment, then everything is much more complicated, since until now doctors have not reached a common point of view, both regarding the choice of medications and their dosages, duration of treatment and place of administration.
Of the medications, the most studied is methotrexate . This drug is a cytostatic (stops cell division) and, when used during ectopic pregnancy, causes tubal abortion or destruction of the fertilized egg.
Options for its introduction:
- Systemic use (in the form of tablets or intravenous injections).
- Local introduction:
- under the control of a transvaginal ultrasound sensor;
- During laparoscopy, local injections of the drug are made into the wall of the fallopian tube.
- Combined administration (combination of systemic and local).
In many countries around the world, other drugs are also being actively studied: prostaglandins (terminate pregnancy by increasing the contractile activity of the tube), Mifepristone (used before surgery, causes detachment of the fertilized egg, facilitating its removal from the cavity of the tube), other cytostatics (in addition to methotrexate).
Progress of the operation
Another complication that may arise during the operation is injury to neighboring organs by the inserted manipulators. As a result, internal bleeding may begin. That is why at the end of the procedure the doctor examines the abdominal cavity and organs for damage.