What is the placenta for?
The placenta is the placenta (afterbirth) that connects the body of mother and child.
The placenta is attached to the body of the uterus by blood vessels; it is connected to the body of the child with the help of the umbilical cord. Inside the umbilical cord there are 2 arteries that carry blood from the fetus to the placenta. And 1 vein, which serves to transport oxygen and nutrients from the placenta to the fetus. The afterbirth performs certain functions throughout pregnancy:
- Gas exchange (delivery of oxygen to the fetus). Oxygen molecules pass through the mother's blood to the fetus, carbon dioxide is transported in the opposite direction.
- Delivery of nutrients to the child: water, vitamins, electrolytes. Removal of fetal metabolic products through the mother's blood.
- Production of hormones to support pregnancy and lactation.
- Fetal immune defense function. The placenta passes maternal antibodies through itself, which form the child’s immune defense.
The baby's place develops along with the child and leaves the uterus after the birth of the baby.
Treatment and childbirth
Complete restoration of homogeneity with the help of drugs is impossible. The absence of stress and anxiety has a beneficial effect throughout pregnancy.
A heterogeneous placenta during pregnancy is directly related to hypoplasia and hyperplasia. The doctor prescribes medications to improve uterine tone, blood circulation and proper oxygen delivery to the fetus. As an additional method - a healthy lifestyle and giving up bad habits. An ultrasound scan before the due date is also a necessary aspect of health monitoring.
Treatment of heterogeneity of the placenta:
- eliminating stress and depression;
- decreased tone, hypoxia;
- therapy of diseases: hypoplasia and hyperplasia;
- delivery.
A woman should strictly follow the doctor’s recommendations and take medications if they have been prescribed. Monitoring of fetal development should take place at all stages of gestation. If you follow the rules and lead a healthy lifestyle, then there is no need to fear for the unborn child and childbirth.
The tactics for managing childbirth with placental insufficiency are prescribed by the attending physician based on the condition of the woman’s body. Premature aging of the placental organ is an abnormal indicator that even causes concern to the doctor. With proper treatment, the problem can be corrected.
Birth of the placenta
5-40 minutes after the birth of the child, the placenta is born. Contractions of the uterus lead to a decrease in the placental area to which the baby's place was attached. After several contractions, the placenta separates from the wall of the uterus, and the obstetrician asks the woman in labor to push slightly. The placenta is born painlessly and fairly quickly.
After removing the placenta, the doctor carefully examines it. If a violation of the integrity of the placenta is detected, this may mean that pieces of membranes remain in the uterine cavity. They must be urgently removed from the uterine cavity to prevent the development of the inflammatory process. Manual examination of the uterus is performed under anesthesia.
The progress of pregnancy can be judged by how the afterbirth looks. Infectious or inflammatory processes will be visible in the condition of the child's place. This is important information for neonatologists and pediatricians who monitor the health of the newborn.
What to do if the placenta ripens prematurely?
It is imperative to take into account the fact that the “aging of the child’s seat” during pregnancy itself does not threaten either the mother or the unborn child. Only with a complex combination of several pathological signs can we talk about a threat to health, among them:
- disruption of uteroplacental-fetal blood flow;
- signs of intrauterine retardation in the development of the child;
- hypertension (persistent increase in blood pressure) in the mother;
- maternal diabetes;
- presence of Rh conflict.
All these conditions are dangerous in themselves and require careful monitoring. However, the “prematurely aged child’s place” is a reason for additional diagnostics - Doppler blood vessels of the placenta and cardiotocography (CTG). If these studies show normal blood flow and heart rate values, there is no need to worry about the fact that the placenta is “overripe”. If studies reveal severe fetal hypoxia, strict monitoring or, in some cases, emergency delivery is required.
Heterogeneous structure of the placenta
The condition of the placenta greatly influences how pregnancy and childbirth will proceed. She is also responsible for supplying the fetus with nutrients and oxygen. Therefore, doctors regularly examine this organ in order to identify possible abnormalities in time.
For this purpose, ultrasound diagnostics is used. With its help, doctors determine the location of the child's place, its thickness, and degree of maturity. As a result, many women expecting a baby learn that their placenta structure is heterogeneous.
Should I worry?
- Most often, the first reaction to such a conclusion is confusion and fear that this will have a negative impact on the child’s condition. After all, it is the child’s place that protects him from various infections and produces hormones necessary for his growth and development. Without it, oxygen access to the fetal blood will be impossible. However, there is no need to worry - in some cases, a heterogeneous placenta is considered completely normal.
- This organ is finally formed by the 16th week of pregnancy. Up to the 30th week, its structure does not change. If during this period the doctor discovers some inclusions or echo-negative areas in it, this may be a cause for serious concern. In this case, the heterogeneous structure of the placenta often indicates a disruption of its normal functioning.
- The reason for this may be infections present in the mother’s body, or previously suffered by her. Anemia, smoking and some other factors also have a negative impact on a child's place. If present, a heterogeneous placenta can lead to serious consequences for the fetus. Often, due to various formations in it, the blood flow between mother and child is disrupted. When the embryo begins to receive less oxygen, its development slows down. Hypoxia can even cause pregnancy to fail.
- But if a heterogeneous structure of the placenta is detected in a woman after 30 weeks of gestation, then everything is going as expected. For some expectant mothers, changes in the child's place are recorded as early as 27 weeks of pregnancy. If all other indicators are normal and the fetus feels well, there is no cause for concern.
- They appear if the degree of heterogeneity of the organ is too high and its thickness is small.
Then we can talk about its premature aging. To find out whether the blood flow of the vessels is impaired due to this, additional studies are carried out - for example, Doppler measurements are done. Based on their results, the mother of the unborn baby is often prescribed a course of treatment. In particularly difficult situations, it is carried out under the supervision of a doctor in a hospital. Moreover, it is impossible to completely change a heterogeneous placenta. But drugs that improve blood circulation, normalize the flow of oxygen to tissues and relieve the tone of the uterus are simply necessary. So listen to your doctor, worry less and rest more. And always monitor your health, avoiding infections whenever possible, both before and during pregnancy.
FPN
Fetoplacental insufficiency (FPI)
- one of the most common complications of pregnancy. In 50-77% of pregnant women it becomes the main cause of miscarriage, in 32% it occurs as a result of gestosis, in 25-45% of cases it develops in the presence of extragenital pathology, after a viral or bacterial infection it manifests itself in more than 60% of cases.
Fetoplacental insufficiency, or placental insufficiency (PI)
, is characterized by morphological (structure) as well as functional disorders in the placenta, the progression of which can lead to hypoxia, developmental delay and even antenatal fetal death.
The placenta is an extremely important organ; it becomes an “intermediary” in the creation of a unified functional system “mother-placenta-fetus”, and performs a number of vital functions for the fetus:
- Respiratory (oxygen delivery, carbon dioxide removal);
- Fetal nutrition and excretion of metabolic products;
- Protective (a kind of barrier and filter that protects the fetus’s body from the adverse effects of harmful factors that enter the mother’s body: some medications, toxic substances, microorganisms);
- Hormonal (produces hormones necessary for the normal course of pregnancy and fetal development).
dangerous When FPN appears, all these functions are disrupted, and a threat arises to the further normal course of pregnancy and fetal development.
Classification
According to the time and mechanism of occurrence, two types of PN are distinguished
:
- Primary
(up to 16 weeks), associated with disruption of the processes of placentation and implantation; - Secondary
(after 16 weeks), develops under the influence of external factors affecting the fetus and/or mother in an already formed placenta.
According to the clinical course, PN is divided into
:
- Acute
– most often occurs against the background of abruption of a low or normally located placenta. Acute PN occurs mainly during childbirth, but its occurrence at any stage of gestation cannot be ruled out; - Chronic
– occurs at various stages of pregnancy. In turn, it is divided into:
A compensated form of PN – in which metabolic processes in the placenta are disrupted, but blood circulation in the “mother-placenta-fetus” system is not impaired. Due to the compensatory capabilities of the mother’s body, the fetus adapts to these changes and does not experience discomfort;
Subcompensated form of PN - if the causes of PN have not been eliminated, the body’s compensatory mechanisms are under stress and gradually begin to deplete, reaching the next stage;
Decompensated form of PN - progression of the pathological process leads to the occurrence of hemodynamic disturbances in the “mother-placenta-fetus” system at the level of fetal-placental and/or utero-placental circulation.
When using the Doppler method, 3 degrees of decompensated form of FPN
:
- I degree FPN I degree – hemodynamic disturbance occurs only in the uteroplacental blood flow;
- FPN degree Ib - the disorder occurs only in the fetal-placental blood flow;
- II degree – there is a disturbance of blood flow at two levels, but they do not reach critical values;
- III degree – the level of disturbances in the fetal-placental blood flow is critical, the life of the fetus is at risk.
In 60% of cases, FPN leads to intrauterine growth retardation (IUGR), so it is also divided into:
- Placental insufficiency with FGR;
- Placental insufficiency without FGR.
Causes
The causes of fetoplacental insufficiency are multiple.
Primary PN occurs as a result
:
- Genetic disorders;
- After bacterial and viral infections suffered in the early stages of pregnancy;
- Endocrine pathologies (ovarian hormonal insufficiency, etc.).
Secondary FPN develops as a result
:
- Primary PN;
- Obstetric and gynecological diseases (menstrual irregularities, infertility, gestosis, miscarriage, uterine fibroids, multiple births, etc.);
- Extragenital diseases (diabetes mellitus, hypertension, blood, lung, kidney diseases);
- Congenital and hereditary pathology in the fetus or mother;
- Unfavorable social and everyday factors (mother's age is more than 30 or less than 18, psycho-emotional overload, heavy physical labor, harmful working conditions, smoking, drinking alcohol and drugs);
- Exposure to external environmental factors (ionizing radiation, use of medications).
The most significant risk factors for the development of FPN are the presence of extragenital pathology and gestosis, accompanied by vascular damage.
Symptoms
Information The compensated form of chronic FPN most often does not manifest itself at all. The woman’s condition is satisfactory; disturbances in the mother-placenta-fetus system can only be determined by additional studies (ultrasound, Doppler).
Symptoms of fetoplacental insufficiency begin to appear only in the decompensated form of PN.
However, at first, a pregnant woman may only present complaints characteristic of extragenital and obstetric diseases, against the background of which FPN develops, for example, headache with hypertension or swelling with gestosis.
But in parallel with this, she may note that the number of fetal movements has decreased. Remember that regular, but not too frequent movements of the fetus are an important sign of its condition!
If intrauterine growth retardation occurs during PN, then there is some discrepancy between the height of the uterine fundus and the gestational age (an indirect sign), which can be detected at the next visit to the antenatal clinic.
The appearance of bloody vaginal discharge at different stages of pregnancy is a dangerous symptom. It indicates that premature placental abruption has occurred, which can lead to acute FPN and fetal hypoxia. In this case, it is better to seek medical help immediately!
Diagnostics
Particular attention should be paid to women at risk for developing FPN. Such pregnant women require regular clinical monitoring.
At each obstetric examination, the doctor should pay attention to weight gain, measure the height of the uterine fundus (UFH) and abdominal circumference.
The discrepancy between the difference in the numerical value of the gestational age and the gestational age, a decrease in the number of movements, a change in the frequency and dullness of the fetal heartbeat sounds is a signal for additional research.
FPN can be determined using 3 main methods
:
- Ultrasonography
. This method allows you to assess the condition of the placenta (thickness, location, degree of maturity, etc.) and the fetus (size, presence of malformations, compliance of growth rates with gestational age), as well as measure the amount of amniotic fluid; - Doppler
. Using this diagnostic method, the blood flow in various vessels of the mother and fetus is examined, which makes it possible to more accurately determine the degree and level of disturbances in the mother-placenta-fetus system, and also allows you to select rational therapy; - Cardiotocography
. A study that allows you to evaluate the cardiac activity of the fetus and indirectly judge its condition.
Timely diagnosis of FPN helps to recognize and respond with adequate treatment to abnormalities in the development of the fetus and the course of pregnancy.
Treatment
In the compensated form of FPN, outpatient treatment is allowed subject to constant monitoring (the number of visits to the antenatal clinic increases). In other cases, hospitalization is necessary.
Unfortunately, all existing treatment methods do not completely restore the normal functions and structure of the placenta.
They only help stabilize the process and prevent its further progression.
Additionally , since the main reason for the development of this pathology is impaired blood circulation in the vessels, all actions should be aimed at eliminating them.
Therefore, FPN should be treated using the following drugs: Trental, Curantil, Pentoxifylline, Eufillin. Actovegin and Troxevasin are used to improve and activate metabolic processes in fetal tissues. FPN is often accompanied by increased uterine tone; to reduce it, medications such as Ginipral, No-shpa, and Magnesium Sulfate are used.
All treatment measures are carried out exclusively in a hospital, under the strict supervision of doctors and constant monitoring of Doppler measurements, ultrasound and CTG, for at least 2 weeks.
Risks and consequences
Placental insufficiency during pregnancy often leads to the following complications:
- Termination of pregnancy;
- Fetal hypoxia;
- Delayed development and growth of the fetus;
- There is a risk of antenatal (intrauterine) fetal death.
important The presence of FPN during pregnancy does not mean that the child will be born with FGR or prematurely. With a small degree of hemodynamic disturbances in the mother-placenta-fetus system, early detection and adequate treatment, the prognosis for pregnancy and the fetus is favorable. Of course, with severe hemodynamic disturbances, the positive outcome of the disease is questioned.
Prevention
Prevention of FPN during pregnancy should be aimed at eliminating unfavorable risk factors and include:
- Maintaining a healthy lifestyle: complete rejection of bad habits;
- Full sleep;
- Rational and proper nutrition;
- Taking vitamins;
- Elimination of heavy physical labor and stress;
- Treatment of chronic diseases and sexually transmitted infections at the stage of pregnancy planning.
Source: https://baby-calendar.ru/mama/fpn/
Heterogeneous structure of the placenta
The placenta is invaluable in the development of the fetus; its condition determines how pregnancy and childbirth will proceed. Therefore, the placenta is regularly examined using ultrasound diagnostics for the timely detection of its abnormalities. As a result, a significant number of pregnant women find out that their placenta structure is heterogeneous. There are many worries about this, because the condition of the placenta determines the access of oxygen to the fetus, its protection from all kinds of infections, and the production of hormones that are necessary for its development and growth. Although in some cases, the heterogeneous structure of the placenta is considered normal.
Causes and symptoms
The main reasons for heterogeneity of the placenta may be infectious diseases, even those that existed before, or the negative consequences of drinking large quantities of alcohol and smoking. This leads to disruption of blood flow from mother to baby. Oxygen starvation of the fetus or the fading of the pregnancy process occurs. A striking symptom is a change in the movement of the child inside. Quitting smoking and alcohol reduces the risk of placental defects
If changes occurring in the structure are detected by a doctor at week 30, this fact is normal in development. The main condition is the absence of serious abnormalities in the fetus. The causes of heterogeneity are most often a combination of incorrect actions of the mother, including nervous experiences. The more comfortable and calm the mother is, the better the unborn baby will feel. The psycho-emotional state determines the state of the female body.
You should refrain from contact with sick people, as you can become infected with an infectious disease. And this is another negative factor leading to improper development of the structure.
20 - 27 weeks. A heterogeneous structure of the placenta at 20 weeks is a common phenomenon among mothers. In case of a negative change in the condition of the organ, the ultrasound procedure will immediately report the initial stage of the pathology. The placenta may remain heterogeneous until the 27th week; after this period it returns to normal. Do not panic, each individual organism has its own developmental characteristics.
30-32 weeks. Upon reaching 30 weeks, the structure of the organ should become homogeneous. If at 30-32 weeks the structure remains heterogeneous, then this indicates the presence of pathology in the female body. A heterogeneous placenta at 32 weeks indicates a serious pathology occurring in the body.
Afterbirth - description and structure of the organ
The placenta (baby place) is an embryonic organ that exists only during the period of bearing a child. This is a very important organ that ensures nutrition, respiration and normal development of the embryo. In addition, the afterbirth protects the child from various types of harmful effects. The question of what the afterbirth looks like interests many. Externally, the organ resembles a cake, and inside it there is a membrane that connects the circulatory system of the mother and the embryo.
Composition of the placenta: • Placenta • Umbilical cord • Membrane (aqueous, villous, decidual).
The chorionic villi attached to the uterus form the placenta. The placenta with all its membranes is the afterbirth. The placenta has 2 surfaces: external and internal. The outer (maternal) is adjacent to the wall of the uterus, it consists of lobules (from 15 to 20 pieces), which are covered on top with a gray membrane. Each lobule is pierced by villi through which blood vessels pass.
The inner (fruit) surface is adjacent to the fertilized egg, and a water membrane envelops it on top. The fetal surface is covered with blood vessels that rush to the root of the umbilical cord, attached to the center of the inner surface of the placenta.
From the inside, the uterus is covered with 3 membranes: maternal (decidual), fetal (chorion), internal (amnion). Inside the amnion is amniotic fluid in which the embryo floats. The aqueous membrane envelops the placenta and the umbilical cord. The fruit and water membranes are separated from each other.
The umbilical cord connects the embryo to the placenta. Two umbilical arteries pass through the umbilical cord, through which venous blood flows and a large vein that transports oxygen and nutrients to the fetus. Around the vessels there is germinal tissue (Wharton jelly), which protects them from compression by tissues.
Calcifications
Calcifications are salt formations that are deposited on areas of dead organ tissue. The placental organ contains multiple blood vessels. They transport vital substances to the unborn child. In case of vessel spasm or failure, it leads to the death of the area. Calcium salt deposits form on dead areas of tissue.
The deposition of calcifications in the placenta can result from:
- pathological process of the uterus;
- severe anemia;
- gestosis and its manifestations;
- infection and chronic diseases;
- sexually transmitted diseases;
- bad habits.
In order for the pregnancy to proceed positively, periodic examinations by a doctor are required. A modern way of observing the process is the ultrasonic method, that is, ultrasound. With its help, pathology is identified in the early stages and calcifications are detected in areas.
Symptoms. In the case of a single deposition of calcifications, the woman will not feel discomfort. This will not harm the unborn child. If multiple foci of salt deposits form on dead tissue, this seriously harms the fetus. With a strong phenomenon, the woman notices a change in the nature of the child’s behavior inside. He becomes too active or, on the contrary, calms down. Impaired performance results in failure to perform adequate life support functions. The child does not receive additional oxygen. In severe cases, the death of the fetus inside the female body occurs.
Treatment. It is impossible to completely remove salt deposits inside the body. To begin with, the doctor establishes the specific cause of the appearance of salts and tries to eliminate the possibility of relapse. If salts were noticed late in pregnancy, and their quantity is small, then periodic examinations of the woman in labor are prescribed. The doctor monitors the situation using ultrasound and monitors the heterogeneous placenta with calcifications. The examination reveals a large number of foci of salts, but the functioning of the placental organ can proceed without disturbance. If the fetus continues to receive the necessary vital substances, then taking therapeutic drugs is not required.
Complications. If dysfunction is detected, if the fetus suffers from lack of oxygen and nutrition, the doctor prescribes appropriate treatment. It includes taking medications that normalize blood circulation, as well as vitamins. Additional drugs in treatment are stimulants of the metabolic process.
Close monitoring of the structure of the placenta during pregnancy is required. Also, do not forget about the normal, comfortable development of the fetus inside the mother’s body. Based on his behavior and well-being, conclusions are drawn about the normal process of gestation.
The placenta performs many important functions during pregnancy. First of all, it carries out gas exchange, transporting oxygen to the fetus and removing carbon dioxide. Through the placenta, the fetus receives the nutrients it needs for development and gets rid of waste products. The placental barrier protects the baby from viruses and bacteria. Finally, the placenta serves as the endocrine system for the fetus.
What features of this organ will doctors pay attention to during an ultrasound examination? We have already talked about the degrees of maturity of the placenta and problems with its location. Let us recall that usually the baby's place is attached to the back wall of the uterus, and develops according to a certain pattern, providing at each stage all the needs of the fetus. By week 36, the placenta reaches its full maturity and aging begins. By the end of pregnancy, the placenta normally has a diameter of 15-18 cm and its thickness is 2-4 cm.
Another issue that will be of interest to doctors is the thickness and structure of the placenta. These indicators will be discussed in today’s article.
Functions of a child seat
The placenta of pregnant women is an important organ that performs the following functions:
• Gas exchange. The placenta transports oxygen from the mother's blood into the fetal bloodstream, and carbon dioxide is removed to the outside with the help of maternal red blood cells. With stenosis or blockage of blood vessels, the child suffers from oxygen starvation, which disrupts his development.
• Nutritious. The placenta provides nutrition to the embryo, metabolites are transported back, and this is how the excretory function manifests itself.
• Endocrine. The placenta produces hormones and biologically active substances that are necessary for the pregnant woman and the fetus (human chorionic gonadotropin, placental lactogen, estriol, progesterone). Based on the concentration of these substances, the condition of the placenta can be assessed and pathologies in the development of the embryo can be identified.
• Protective. The placenta protects the fetus from the mother's antibodies and also prevents the penetration of embryonic antigens into the mother's blood. In this way, the organ prevents an immunological conflict between the two organisms. However, the placenta is not able to protect the fetus from drugs, alcohol, nicotine and viruses. If the development of the placenta is disrupted, complications that are dangerous for the mother and child arise.
What causes pathology
Early maturation of the placenta is caused by any factor that enhances the functioning of the mother-placenta-fetus complex. Disorders in the mother’s body, external unfavorable factors, and complications of gestation can trigger the aging process. Obstetricians include the most common triggers for the development of pathology:
- Extragenital diseases. Premature aging of the placenta is observed in expectant mothers suffering from chronic general and endocrine pathologies (kidney disease, hypertension, hypo- and hyperthyroidism, diabetes mellitus). Aging is caused by an increase in the load on initially incompetent organs and microcirculation transformations during gestation.
- Chronic pathology of the genital organs. Disruption of the implantation process and subsequent activity of the child's place is provoked by structural changes in the uterine walls caused by abortion, diagnostic curettage, adenomyosis, chronic endometritis, hyperplastic processes of the endometrium or submucous myoma. Also, premature aging of the placenta is observed with dishormonal disorders (inflammation of the ovaries or appendages, scleropolycystic ovaries, ovarian tumors).
- Preeclampsia. This complication of pregnancy causes characteristic changes in the circulatory system, increased permeability of the vascular walls, which affects increased blood flow in the uterine wall and the mother-placenta complex. In the initial stages of gestosis, compensatory mechanisms maintain normal blood flow in the maternal-placental-fetal complex. But when compensation processes fail, the growth of the organ accelerates, further development up to maturation with subsequent aging.
- Infectious diseases. The threat of damage to the embryo by pathogenic microorganisms increases the load on the placenta, which performs a protective function. Premature aging of the organ can be provoked by pathogens of sexually transmitted infections (herpes simplex, chlamydia, ureaplasmosis, mycoplasmosis) and other infectious diseases (toxoplasmosis, cytomegalovirus infection, influenza, ARVI, rubella, etc.).
- Incompatibility between the pregnant woman and the fetus based on blood type or Rh factor. With isoserological incompatibility, hemolytic disease of the fetus often develops; it needs an increased supply of oxygen and nutrients, which increases the load on the placenta. Increased work of the child's place and typical disruptions of microcirculation in it lead to accelerated growth, subsequent maturation and aging of the organ.
Also, predisposing factors for premature aging of the placenta include:
- disturbed ecology;
- exposure to industrial hazards (radiation, working with chemicals, high ambient temperature);
- bad habits (smoking, consumption of alcohol and psychotropic drugs);
- incorrect use of medications;
- being underweight or overweight;
- sedentary lifestyle;
- irrational and/or insufficient nutrition;
- hypovitaminosis;
- excessive interest in vitamin complexes.
note
Carrying a multiple pregnancy significantly increases the risk of pathology, since the load on the fetoplacental complex increases several times.
Possible problems associated with the placenta
One of the most common pathologies of the placenta is low placental attachment. If the problem is determined after the 28th week of pregnancy, then we are talking about placenta previa, which blocks the os of the uterus. However, only 5% of women retain this arrangement until 32 weeks.
Placenta previa is a dangerous complication of pregnancy in which the placenta moves to the lower segment of the uterus. This pathology occurs in repeat births, especially after abortion and postpartum complications. Complications can be caused by neoplasms, abnormal development of the uterus, and low implantation of the fertilized egg. With placenta previa, the risk of uterine bleeding and premature birth increases.
Placenta accreta is a condition characterized by tight attachment of the placenta to the uterus. Due to the low location of the placenta, chorionic villi grow into the myometrium or into the entire thickness of the uterus. As a result, the afterbirth does not come off on its own.
Tight attachment differs from the previous pathology only in that the chorionic villi grow to a shallower depth into the uterine wall and provoke retention of the placenta. In addition, this anomaly provokes bleeding during childbirth. In both the first and second cases, they resort to manual separation of the placenta.
Placental abruption is a pathology that is characterized by premature (before the birth of the child) separation of the placenta from the wall of the uterus. In this case, the uteroplacental vessels are damaged and bleeding occurs. The intensity of symptoms depends on the area of detachment. With a small detachment, natural childbirth is indicated, followed by examination of the uterine cavity. In case of severe detachment, a cesarean section is indicated.
Premature maturation of the placenta is characterized by early maturation or aging of the organ. In this case, the following types of placenta are observed: • Thin – less than 2 cm in the 3rd semester of pregnancy. This problem is typical for gestosis, intrauterine retention, and threatened miscarriage. • Thick – more than 5 cm in hemolytic disease and diabetes mellitus. It is necessary to carry out diagnosis and treatment.
Late maturation is more often diagnosed in women with diabetes mellitus, pregnant women who smoke, Rhesus conflict between mother and child, and congenital anomalies of fetal development. A small placenta is not able to perform its functions, and this threatens stillbirth and mental retardation of the child. The risk of placental infarctions, inflammation of the placenta or fetal membranes (for example, grade 3 ascending bacterial infection of the placenta), as well as placental neoplasms, increases.
Classification
In systematizing the degrees of maturity of a child's place, the features of its physiological growth, development and structural transformation of placental tissue characteristic of a certain gestational age are taken into account.
In obstetrics, there are 4 degrees of organ maturity:
- Zero – 0. This degree of maturity indicates the formation of the placenta, the youth and inexhaustibility of the functional resources of the organ. The structure of such a placenta is homogeneous, there are no calcifications. Zero degree is characteristic of the period from 2 to 30 weeks.
- The first is 1. Indicates the growth of the placenta. The proliferation of blood vessels in the organ is completed, the undulation of the chorionic membrane appears, and microscopic compactions and single calcifications are detected in the organ. The organ copes with its role, the fetus receives sufficient nutrients and oxygen. Corresponds to a 30 - 34 week period.
- The second is 2. It speaks of the maturity of the placenta; active regressive processes have begun in its tissues: the undulation of the membrane increases, the acoustic density increases, multiple echo-positive calcium inclusions are revealed, the organ becomes fragmentarily thinner. The placenta continues to function normally, the fetus does not suffer. The second degree is observed at 35–39 weeks of gestation.
- Third - 3. Indicates the aging of the organ: pronounced tortuosity of the chorionic plate appears, structurally the placenta is divided into lobules, cysts form in the placental tissue and many calcifications are visualized. The organ loses in size and volume. The third degree is typical for 37 and later weeks of gestation and can be determined just a few days before birth.
Pathology is indicated when manifestations of the 1st degree of maturity appear before the 27th week of pregnancy, the 2nd degree before the 32th week of gestation, and the third before the beginning of the 36th week of gestation . Accelerated maturation of an organ indicates a high risk of its functional failure and disruption of protective mechanisms in the mother-fetus complex.
note
The establishment of an intermediate degree on ultrasound, for example 0 - 1, indicates signs of a transition from one stage of maturation to another, but the transition itself is not yet complete.
The norm is considered to be 0 - 1 degree, detected at 27 - 28 weeks. Pathology includes grades 1–2 at 32 weeks and grade 3 detected before 38 weeks.
Birth of a child's place
The phrase: “The placenta passed away after childbirth” confuses many first-time women. After all, the 3rd stage of labor, when the placenta is born, is also very important, this is how the uterus is cleansed. Doctors monitor the woman, assess her condition, monitor her heartbeat and try to determine how much blood she has lost. To assess the degree of blood loss, a metal bowl is placed under the woman. It is important to empty your bladder regularly so that it does not retain the placenta.
After about 2 hours and blood loss of no more than 220 ml, the afterbirth comes out. In case of bleeding and retention of the placenta, external expulsion of the organ is performed. It is very important to completely remove the placenta after childbirth, because even a small piece of it can cause dangerous complications: severe uterine bleeding or purulent infections.
The mechanism of development of low placentation
7-8 days after conception, the fertilized egg enters the uterine cavity, where it attaches to one of its walls.
Normally, embryo implantation should occur in the upper part of the organ. The physiological position of the fertilized egg is in the fundus of the uterus, but it can be located on the front, back, right or left side. If the embryo is fixed in the area of the lower segment, obstetricians-gynecologists talk about. By approximately the 14th week of gestation, the placenta is formed from the chorion, the place of attachment of which depends on the primary implantation of the fertilized egg. However, the uterus grows throughout the entire period of gestation, so sometimes the incorrect position of the membranes can become physiological by the middle or end of pregnancy.
Low placentation along the anterior wall is the most favorable variant of the pathology, since due to the abdominal muscles, the outer uterine wall stretches well, and the baby’s place moves along with it.
If the placenta is located on the back side of the organ, the chances of its normal position at the end of pregnancy are slightly lower. This is due to the fact that there is a spine behind the uterus, which prevents it from stretching too much.
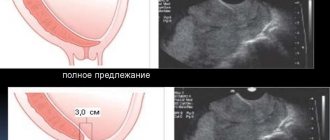
The low location of the placenta should be distinguished from its presentation. The second diagnosis has the same etiology and development mechanism, but is a more severe variant of the first. Placenta previa is a pathology in which the baby's place extends onto the uterine os. Experts distinguish between complete and partial presentation.
With complete presentation, the placenta completely covers the uterine os. The pathology is accompanied by multiple and frequent complications; if it is detected, natural childbirth is impossible. With complete placenta previa, upward migration almost never occurs.
In partial presentation, the baby's place extends onto the uterine os, but does not completely cover it. This diagnosis has a more favorable outcome: upward migration of the baby’s place is possible, complications are less common, and in some situations, natural delivery is possible.
Signs of placenta separation
The process of separation of the baby's place from the umbilical cord and fetal membranes is called the birth of the placenta. There are several characteristic signs of separation of the placenta:
• Schroeder's sign – the condition, shape and height of the uterus changes. When the placenta separates, the uterus becomes flatter and its bottom rises towards the navel. The uterus deviates to the right side.
• Alfred's sign – the free end of the umbilical cord becomes longer. After the baby is born, the umbilical cord is crossed, and its other end goes into the vagina. The doctor places a clamp on its end. When a woman's placenta descends into the lower part of the uterus, the umbilical cord also lengthens.
• Mikulicz's sign is the urge to push. This symptom does not appear in all women giving birth.
• Klein's sign - after pushing, the umbilical cord, which protrudes from the vagina, lengthens. If, after the end of pushing, the length of the umbilical cord does not decrease, then the placenta has separated from the uterus.
• Klyuster-Chukalov sign – when pressing on the suprapubic area, the umbilical cord lengthens. After the end of the physical impact, the umbilical cord remains motionless. If at the 3rd stage of labor the woman in labor feels normal, the placenta has not separated, and there is no bleeding, then the waiting period is extended to 2 hours. If after this time the mother’s condition has not changed or even worsened, then the placenta is removed manually.
Thickness and location of the placenta on ultrasound
Using ultrasound diagnostics during pregnancy, the thickness of the placenta and its presentation are determined, and cysts and calcifications (calcium deposits in the tissues of the organ) are excluded. The thickness of the “baby place” constantly increases until the 32nd week of pregnancy, and is normally about 30 mm.
Thickening or, on the contrary, decreasing the thickness of the “children's place” is a direct consequence and indicator of its premature aging. An increase in thickness (more than 4 cm) may occur due to Rh conflict, an infectious disease, or be a consequence of maternal diabetes.
Using ultrasound, the exact location of the organ’s attachment to the uterus is assessed to exclude its presentation. The localization of the “baby place” is determined during each screening ultrasound examination, starting from 10 weeks, but only at the third planned ultrasound procedure will it be possible to finally see the features of the location, and in the case of a pathological condition, determine the low attachment of the placenta - its previa:
- if there is a complete overlap of the internal os of the uterus, then they speak of a central presentation of the “baby place”;
- if the internal pharynx is blocked only by the edge of the organ - about marginal presentation;
- if close to the internal uterine os - low presentation.
There are often cases when placenta previa is diagnosed at the second ultrasound, but by the end of pregnancy, if placenta abruption does not occur, the localization of the “child’s place” again becomes normal - above the internal uterine os. That is why final conclusions about the level of localization of the organ should be made only by the end of the 3rd trimester.
The placenta blocking the entrance to the uterus is called presentation and is a pathology. If it is detected, the doctor must diagnose the form of presentation - marginal, low or central. Final results can be obtained only after the 3rd trimester, when the placenta has already acquired a stable position and has matured
Methods of expelling a child's place
The succession period takes little time, but this does not reduce its complexity. At this stage, the risk of uterine bleeding increases, which threatens the woman’s life. After all, if the baby’s place is not born, then the uterus can no longer contract, and the blood vessels do not close. Then doctors use emergency methods for separating the placenta:
• Abuladze method. The doctor performs a gentle massage of the uterus, then grabs the abdominal wall by the longitudinal fold and asks the woman in labor to push. External separation of the placenta using the Abuladze method does not cause pain; it is quite simple and effective.
• Genter's method. The fundus of the uterus is brought to the midline. The doctor turns sideways to the woman so that he can see her legs, clenches his hands into fists, and presses the back surface of the main phalanges to the fundus of the uterus. The physician applies gradual pressure, moving the placenta down and inward. The woman in labor should not push.
• Credet-Lazarevich method. This method is used if previous methods were ineffective. The fundus of the uterus is brought to the middle position, and its contractions are stimulated with the help of a light massage. Then the obstetrician should stand on the left side of the woman so as to see her legs, clasp the fundus of the uterus with his right hand so that 1 finger rests on the front wall, the palm on the bottom, and 4 fingers on the back surface. The physician then squeezes out the placenta by squeezing the uterus with one hand while pushing out the placenta with the other. These are effective methods for separating the placenta, which are used if the baby’s place has separated from the uterus on its own. In this case, the doctor simply facilitates his exit.
How and when it is carried out
Ultrasound scanning of the placental membrane is carried out already from 10-12 weeks of pregnancy during each routine ultrasound examination. However, it is possible to finally judge its functional state, localization, thickness and the presence or absence of pathology only after the third screening ultrasound. It is at these stages of pregnancy that the placenta reaches its maximum development and is best visualized.
As mentioned above, ultrasound of the placental membrane can be performed in two ways:
- Transvaginal, when a sensor-converter of high-frequency ultrasonic waves is inserted directly into the vaginal cavity, but before that a disposable diagnostic condom is put on it and a transparent gel is applied. Maximum proximity to the uterus allows you to obtain the clearest and most accurate echo picture of the condition of the placenta. The procedure is painless and harmless, despite some discomfort.
- The transabdominal method is more suitable for examining the placenta by ultrasound at 21 weeks of pregnancy and at a later date. The technique is that the procedure is performed through the outer abdominal wall, which is absolutely atraumatic and painless. The woman lies down on the couch in a position that is comfortable for her and the doctor, after which the latter installs the sensor in the suprapubic area and begins the diagnosis.
Thus, ultrasonographic scanning of the placenta is not a separate procedure, but is considered a mandatory step in every routine screening with special emphasis in late pregnancy.
Structural changes in the placenta during pregnancy. Placenta. beremennost9m.ru
Home Pregnancy and childbirth Placenta during pregnancy: placental formation and abnormalities
Placenta during pregnancy: placenta formation and deviations
Through the baby's place (another name for the placenta), the baby receives nutrition and oxygen from the mother's body.
Have you ever thought about how a woman’s body itself finds out about pregnancy? Who gives him the signal for his period to stop and for his breasts to harden and enlarge in preparation for milk production? How does this microscopic embryo adapt the entire organism to itself? The answer is simple: in the early stages of pregnancy, the main ruler is the hormone chorionic gonadotropin. It is produced in the villi that appear on the surface of the fertilized egg when it is implanted into the uterus. These villi are called chorion, hence the name of the hormone they produce. It signals the body that pregnancy has occurred and also helps maintain it. It is this hormone that is found in the urine during a pregnancy test. When the fertilized egg attaches to the wall of the uterus, the villi destroy the vessels and float in the resulting blood lakes, receiving oxygen and nutrients from the mother's blood. In the early stages, the fertilized egg can release such villi from either side. Therefore, if there is a threat of termination of pregnancy. even if part of the fertilized egg has peeled off and spotting appears. If conservation therapy is started in a timely manner, the fetal egg will release new villi, and in the future this will not affect the condition of the fetus in any way. By the 15-16th week, the chorion turns into the placenta, which continues to participate in the transport of oxygen and nutrients. In this case, the blood of mother and child never mixes. During pregnancy, the placenta itself and the umbilical cord that extends from it contain fetal blood. Therefore, after the birth of the baby and the intersection of the umbilical cord, you can take blood from it for analysis and determine from it the blood type and Rh factor of the child. The thickness of the placenta in millimeters is approximately equal to the gestational age in weeks. So, if at 24 weeks the placenta has a thickness of 23-24 mm according to ultrasound, then everything is in order, but if it is 40 mm, it’s time to sound the alarm. The diameter of the placenta at the time of birth is 16-20 mm, and the weight is about 500 g. In large children it is larger, in small children it is smaller. The placenta also performs a hormonal function. It secretes hormones such as progesterone, estriol, placental lactogen and others. All of them are necessary to maintain pregnancy (relax the uterine muscle), as well as for fetal growth and preparation of the mammary glands for breastfeeding. Before birth, the balance of hormones produced by the placenta changes, which helps prepare the uterus for childbirth and ripen the cervix. During pregnancy, the placenta, like a guard, protects the unborn child from toxic substances that enter the mother’s body. True, if there are a lot of these substances, she is not able to cope with them. This is why the expectant mother should not drink alcohol or smoke.
Clinical manifestations
The pathology has no clinical manifestations and is established only instrumentally (ultrasound). The expectant mother, in the absence of an acute process, exacerbation of chronic pathology or a complicated course of gestation, does not complain. If the above is present, the symptoms of the underlying disease come to the fore (for example, with gestosis, high blood pressure and edema). If premature maturation of the placenta provokes significant fetoplacental insufficiency, the motor activity of the fetus changes (the frequency and intensity of movements increases). With a critical disorder in the placental-fetal complex, the child begins to move rarely until the movements completely stop.
Diagnostics
Currently, the diagnosis of “low placentation” is made using ultrasound
when identifying the localization of the child’s place near the uterine pharynx at a distance of 7 centimeters and below. Ultrasound at 19-21 weeks of pregnancy reveals this pathology in 2-3% of pregnant women. However, over time, the placenta can rise and take its normal position in the uterine cavity at the time of birth.
With an ultrasound examination, doctors can note indirect signs of low placentation. These include incorrect position of the fetus - oblique and transverse, as well as breech presentation. With a low position of the placenta, the unborn child in the last weeks of pregnancy cannot descend to the uterine os; it is higher than normal, as can be seen on ultrasound.
A woman with detected low placentation should visit a doctor at certain intervals to monitor the dynamics of the pathology. If there is a history of bleeding, the obstetrician-gynecologist should refer the expectant mother for a blood test for iron and coagulation parameters.
The danger of low placentation
Low placentation itself does not affect the mother’s well-being; the danger of this pathology lies in possible complications.
The most common consequence of an abnormal position of the baby's place is bleeding from the vagina. With low placentation, red discharge usually occurs after the 30th week of pregnancy, but sometimes it does not bother the woman at all. In more severe cases, uterine bleeding may appear at 23-24 weeks of gestation. The reason for bleeding due to abnormal placentation is that the lower segment of the uterus is greatly stretched due to an increase in the weight of the fetus. The child's place does not have time to adapt to the stretching of the muscle wall, resulting in microdetachment. Its development is accompanied by exposure of the vessel, which leads to the release of blood from it.
Bleeding with low placentation has distinctive features. They almost always occur suddenly and are not accompanied by physical or emotional stress. Such bleeding is often observed at night. With low placentation, the discharge is scarlet in color and is not accompanied by pain. Bleeding tends to recur constantly.
Against the background of bleeding, accompanying complications sometimes occur - a drop in blood pressure and anemia. They impair the blood supply to the fetus, which can provoke hypoxia - oxygen starvation. Hypotension and anemia also worsen the well-being and performance of the expectant mother.
Attention! Low placentation may not manifest itself in any way in the first half of pregnancy, sometimes until the very end of the gestation period, so expectant mothers should not skip routine ultrasound examinations.
With chronic severe hypoxia, intrauterine growth retardation and development of the fetus develops. With this pathology, the unborn child lags behind its “peers” in weight and length by two or more weeks of gestational age. Intrauterine growth retardation and development of the fetus can provoke congenital pathologies of the nervous system and other organs, as well as death in the postpartum period.
The abnormal position of the placenta sometimes causes abnormal position of the fetus - transverse (when the fetus is located transverse to the vertical axis of the uterus) and oblique (when the fetus is located at an acute angle to the vertical axis of the uterus). With these pathologies, it is impossible to give birth to a child without surgical intervention. Also, low placentation can provoke breech presentation - a position in which the fetus is born with the buttocks or legs, which complicates natural childbirth and often requires a caesarean section.
The most dangerous complication of low placentation is premature birth. They are observed as a result of detachment of a large area of the child's place. The complication is accompanied by a shortening of the length of the cervix, opening of the internal and external pharynx and the onset of labor.
Marina Aist - low placentation and normal location of the placenta: