How does FPN occur?
Fetoplacental insufficiency is a pregnancy pathology in which placental blood flow is disrupted.
The presence of FPN can be suspected by changes in the frequency and strength of the baby's movements. A sharp increase or decrease in fetal movements, and even more so their disappearance, often indicates an unfavorable condition of the baby, hypoxia and placental insufficiency. The consequences of this pathology are immediate and very dangerous for the fetus, because it is through the placental blood flow that nutrients and oxygen are delivered to the baby. When the speed and level of blood flow decreases in any part of the mother-placenta-fetus system, the baby begins to lack the substances necessary for normal growth and development. With long-term or rapidly developing FPN, not only the development, but also the life of the baby is threatened.
What reasons can lead to disruption of the functioning of an organ that is so important for mother and baby? Most often, FPN develops against the background of acute and chronic diseases of the mother, pregnancy pathologies, or diseases of the placenta itself. Here are the most common risk factors for developing FPN
- Extragenital (not related to gynecology) diseases of the mother. This includes cardiovascular failure, arterial hypertension (increased blood pressure), kidney pathologies (acute and chronic pyelonephritis, glomerulonephritis, urolithiasis, renal failure), endocrine diseases (diabetes mellitus, pathology of the adrenal glands, thyroid gland, pituitary gland), etc. All These diseases affect the speed and level of blood flow in the mother's body, which, in turn, causes a decrease in placental blood flow.
- Diseases of the genital area of a pregnant woman - endometritis (inflammation of the lining of the uterus), inflammation of the appendages, sexually transmitted diseases (ureaplasmosis, mycoplasmosis, chlamydia, herpes, cytomegalovirus, etc.). Infectious agents and their toxins that penetrate the placental barrier are retained by the placental tissue. In places where pathogens invade, pockets of inflammation form, in which blood circulation normal to the placenta is disrupted.
- Pathologies of pregnancy. The most common cause of placental insufficiency in this group is gestosis. One of the manifestations of this pathology is a persistent increase in blood pressure in the blood vessels, which, of course, very quickly affects the level of placental blood flow. Another reason is a violation of hemostasis (the ratio of factors of the coagulation and anticoagulation system of the blood, providing the necessary viscosity and speed of movement through the vessels), often detected in the second and third trimester. Less commonly, placental insufficiency develops against the background of prolonged severe anemia of pregnant women, a disease characterized by a decrease in the level of hemoglobin in the blood.
- Pathologies of the placenta. Like any other human organ, the placenta itself can also become diseased. This disease is called placentitis and is expressed in significant swelling of the placenta and disruption of placental blood flow. The cause of placentitis is mainly viruses that can penetrate the placental barrier. Sometimes foci of inflammation are limited to certain areas of the placenta; in this case, as a result of the disease, petrificates are formed at the site of inflammation - foci of calcification. A large amount of petrificates also impedes placental blood flow.
- Anomalies in the development of the placenta. This includes hypotrophy (“skinny” placenta), additional placental lobules, partial detachment and improper attachment of the placenta.
Causes
Placental insufficiency can occur as a result of the following reasons:
- genetic and chromosomal pathologies in fetal development;
- infectious and inflammatory processes in the mother’s body that occurred in the 1st trimester of the perinatal period;
- hormonal imbalance and ovarian dysfunction;
- pregnancy that occurs after the age of 35;
- maternal malnutrition;
- smoking;
- consumption of alcoholic beverages;
- excessive physical activity;
- chronic psycho-emotional stress;
- maternal diabetes;
- pathologies of the kidneys and excretory system;
- chronic diseases of the heart and vascular system;
- history of abortion;
- pregnancy after diagnosis of infertility;
- pathologies in previous pregnancies;
- miscarriages that preceded the current pregnancy;
- pathologies of the structure of the uterus;
- incorrect location of the placenta;
- severe forms of toxicosis or gestosis;
- excess amniotic fluid;
- bleeding;
- increased thrombus formation.
Why does my stomach hurt? Pain during pregnancy
Pregnancy is a wonderful period in the life of every woman, but the state of health during pregnancy cannot always be called ideal. A pregnant woman is often bothered by various ailments, in particular pain of various types and different localizations. Most often, women complain of pain in the lower abdomen and pelvic area. The pelvic area contains the storage of the growing fetus - the uterus, as well as many other organs (ovaries, intestines, ureters, bladder, as well as bones, muscles and ligaments of the pelvis). And each of these organs can make itself felt by pain in the pelvic area. It is not always possible to understand the source of pain and determine how dangerous this symptom is, even with a cursory examination by a doctor. However, let’s try to figure out what kind of pain you should be most afraid of during pregnancy and how to help yourself.
During pregnancy 12-24 weeks, pain in the pelvic area is often associated with tension in the ligaments that hold the non-pregnant uterus in the correct position
Source
Degrees. Classification
Types of placental insufficiency:
- acute - there is a sharp disruption of placental blood flow, which arose as a result of placental abruption;
- chronic – pathology develops gradually.
In addition, in obstetric practice, compensated and decompensated placental insufficiency are distinguished.
In the first case, the child adapts to negative changes and his health does not suffer. The decompensated form of the pathology provokes a delay in the child’s development.
The symptoms of the acute and decompensated forms are more pronounced. Consequently, a woman may be alerted by alarming signs and unpleasant sensations:
- excessive fetal activity with its abrupt cessation in the future;
- reducing abdominal girth;
- discrepancy between the height of the uterus and the gestational age;
- vaginal discharge with blood.
Chronic and compensated placental conditions are not often asymptomatic. They can only be diagnosed by undergoing an ultrasound examination.
What is placental aging?
Aging of the placenta during pregnancy is a fairly common diagnosis that doctors make to expectant mothers.
This diagnosis is made on the basis of an ultrasound scan and is important for the normal development of the fetus
The placenta goes through 4 stages of maturation:
- zero, which is typical for pregnancy up to 30 weeks;
- the second, which corresponds to pregnancy from the 34th to the 37th week;
- the third, characteristic of the last weeks of pregnancy, that is, from the 37th week until the moment of birth.
Depending on the stage, the placenta changes and has characteristic features. Aging of the placenta during pregnancy is a decrease in the functionality of this organ. This does not mean at all that the placenta, which, for example, has a second degree of maturity, ceases to perform its functions. This body simply gradually reduces the scope of its capabilities.
In this regard, the detection of such pathology in late pregnancy should not cause serious concern. It is much worse when aging of the placenta during pregnancy is detected in the first or second trimester.
Placenta thickness
The normal thickness of the organ is 2–4 cm. If the placenta is excessively thick, this indicates an infectious disease of the fetus. The danger of this phenomenon lies in the appearance of calcifications, which lead to oxygen deficiency.
Hypoxia has a detrimental effect on the development of the embryo. Swelling of the placenta disrupts hormonal levels and can lead to termination of pregnancy. In some cases, premature placental abruption occurs and there is a risk of antenatal fetal death. When the doctor has concerns that the placenta is too thick, he immediately prescribes additional examination to the patient.
Another deviation in the development of the “baby place” is a thin placenta during pregnancy (discrepancy between the thickness and weight and the size of the disc). This pathology occurs as a result of a woman’s smoking and use of alcohol and drugs. A thinned placenta is not able to supply the fetus with the required amount of nutrients and oxygen, which leads to its slow development and subsequent complications during the newborn period. Read more about the thickness of the placenta →
Expectant mothers need to take their health seriously from an early age and also carefully monitor it during pregnancy. This will serve as a guarantee of good health for the unborn baby.
Author: Tatyana Strokan, especially for Mama66.ru
What is placenta
Translated from Latin, placenta literally means “cake”. This is exactly what this organ looks like. However, this cake is the most important element during pregnancy. The growth and development of the unborn baby literally depends on it. The placenta begins to form from the first minutes of fertilization. The egg divides and the resulting cells give rise to a new life. In this process, those cells are formed that will ensure contact between the fetus and the female body. On the 10th day after conception, a lacuna forms in the inner layer of the uterus, filled with the mother’s blood vessels, in which the embryo is located. It receives nutrients from the tissues of the mother's body. Around the embryo, in turn, a branched membrane is formed, into which the vessels of the fetus itself grow. This is how the exchange of blood between mother and fetus is established. This is the beginning of the formation of the placenta. The structure of this organ changes as the needs of the growing fetus change. Only by the end of the 35th week of pregnancy does the placenta reach full maturity. A normal placenta is 18 cm in diameter, its thickness ranges from 2 to 4 cm, and its weight is about 500 grams.
Functions of the placenta during pregnancy
- The most important task of the placenta is to transport oxygen to the fetus through the maternal blood. Carbon dioxide is transported in the opposite direction.
- It is through the placenta that the fetus receives the nutrients necessary for its growth and development, and also gets rid of its waste products.
- The placenta provides immunological protection to the fetus. It passes the mother's antibodies to the child and protects him in this way from many infections. However, many medications, drugs, toxins, pesticides, viruses, alcohol and nicotine easily penetrate into the baby’s bloodstream through the placenta. And they can significantly affect the development of the fetus and even completely affect it.
- The placenta also synthesizes hormones that are responsible for maintaining pregnancy, growth and development of the unborn baby.
Thus, we understand how important the proper development and functioning of the placenta is for a pregnant woman. Throughout pregnancy, the placenta performs important tasks, depending on its stage of development.
Taking into account the evolution of this organ (formation, growth, maturity and aging), doctors use ultrasound to observe changes in the placenta over the entire period of pregnancy. If there are serious deviations from developmental norms, treatment and reinforcement of the body are prescribed.
Functions of the placenta
The placenta really resembles a cake, one side of which is directed towards the wall of the uterus and is called the maternal side. The other side faces the fetus and the umbilical cord extends from it to the embryo. The placenta, up to the moment when its aging occurs, ensures the transfer of all substances necessary for development to the child from the mother’s body.
The role of this organ in medicine is called immune, since, along with nutrients, the fetus receives antibodies from the mother that provide immunological protection:
- The placenta prevents the penetration of certain bacteria and viruses contained in the mother's blood;
- The placenta blocks antibodies that can be produced in case of Rh conflict.
Another function of the placenta during pregnancy is gas exchange: oxygen enters the fetus with the mother’s blood, and carbon dioxide is transported in the opposite direction. With the help of the placenta, the child gets rid of all waste products.
More on the topic Placenta during pregnancy and after childbirth, what you need to know
low placenta
Placenta - during pregnancy and after childbirth: what you need to know. Therefore, in the first and second trimesters of pregnancy, the diagnosis of “low placenta” should not be frightening. Simultaneously with the enlargement of the uterus, the placenta rises.
low placenta recommendations
Placenta - during pregnancy and after childbirth: what you need to know. Therefore, in the first and second trimesters of pregnancy, the diagnosis of “low placenta” should not be frightening. Simultaneously with the enlargement of the uterus, the placenta rises.
My daughter’s birthday, what happened before and what happened after... Part 3: Childbirth
And it flew away... 4:30 They shake me by the leg and spread my arms with the word “That’s it.” I still don’t understand anything, because I’m dying to sleep after a sleepless night of wallpapering. Somehow I wake up. Alenka explains to me that the mucus plug has finally come off and she is having contractions. In general, the fact that the plug has finally come off is a harbinger, but a few days may still pass before the birth. And the contractions may well be trial ones (by the way, we already sat with such trial ones at the dacha for an hour with...
placenta previa
placenta previa. Analyzes, studies, tests, ultrasound. Pregnancy and childbirth. Placenta - during pregnancy and after childbirth: what you need to know.
Low location of the placenta
Placenta - during pregnancy and after childbirth: what you need to know. Therefore, in the first and second trimesters of pregnancy, the diagnosis of “low placenta” should not be frightening. Simultaneously with the enlargement of the uterus, the placenta rises.
Cancellation of Dufston (Utrozhestan) - opinion of the audience
Placenta - during pregnancy and after childbirth: what you need to know. As pregnancy progresses, the outgrowths of the chorion increase in size and turn into the placenta; it is finally formed by the end of the first trimester of pregnancy.
about the formation of the placenta
Placenta - during pregnancy and after childbirth: what you need to know. As pregnancy progresses, the outgrowths of the chorion increase in size and turn into the placenta; it is finally formed by the end of the first trimester of pregnancy.
Once again about low placenta
Placenta - during pregnancy and after childbirth: what you need to know. It also happens that the placenta is located low, when its edge is lower than this. The placenta itself cannot contract, so it moves away from the place of attachment.
Placenta in the day
Placenta - during pregnancy and after childbirth: what you need to know. In a normal pregnancy, the placenta is usually located in the area of the fundus or body of the uterus, along the back wall, with a transition to the side walls - that is, in those places where the walls of the uterus are best...
Low placentation
Placenta - during pregnancy and after childbirth: what you need to know. In a normal pregnancy, the placenta is usually located in the area of the fundus or body of the uterus, along the back wall, with a transition to the side walls - that is, in those places where the walls of the uterus are best...
Low placenta
Low placenta. . Pregnancy and childbirth. Didn't find what you were looking for? See other discussions: Placenta - during pregnancy and after childbirth: what you need to know.
Structure and place of attachment of the placenta
The structure of the placenta is lobular - its lobules (cotyledons) are separated by partitions (septa). The organ develops along with the fetus and is finally formed by the 15th week of pregnancy. Then the mass increases and by 36 weeks it reaches its maximum maturity. Its weight by this time reaches 500–600 g, diameter – from 15 to 18 cm.
In most cases, the placenta is located along the back wall of the uterus. As the period increases, the “baby spot” is localized to the upper part of the cavity.
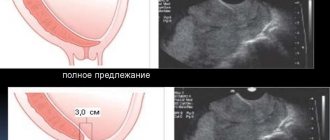
If the organ remains down by 32 weeks, it is called placenta previa. This condition is a complication of pregnancy and can lead to bleeding. More rarely, there are cases when the placenta is fixed along the anterior wall.
The condition of the placenta (how thick it is, what its weight is and whether the size corresponds to the fetus) is determined by ultrasound. In addition to the usual indicators using ultrasound, the blood supply to the placental vessels is studied.
Possible pathologies of the placenta:
- intraplacental thrombi;
- membranous placenta;
- presentation;
- edema;
- detachment;
- increment;
- tumors;
- infectious inflammation;
- early or late maturation;
- placental infarction;
- progressive growth or reduction of the placenta.
Appendicitis in a pregnant woman
Medical statistics show that among women diagnosed with appendicitis, about 3% of patients are pregnant. While waiting for the baby to be born, the expectant mother may experience abdominal pain. Most often they are associated with pregnancy, but you need to remember that this may be a sign of inflammation of the appendix, which is adjacent to the cecum. The appendix, which is what this organ is called in Latin, is located in the right lower abdomen. Sometimes the appendix has an atypical location and descends into the small pelvis or, conversely, rises to the liver. In such cases, it is difficult to make a correct diagnosis, especially during pregnancy.
What causes appendicitis during pregnancy?
The cause of the development of appendicitis or inflammation of the appendix is considered to be blockage of the opening between the appendix and the cecum by small fecal stones. As a result of blockage, the blood supply to the appendix is disrupted, swelling and inflammation occur
Source
What is hypoplasia of the nasal bones in the fetus?
Hypoplasia is a disorder of intrauterine development that can affect almost any organ. The reason for its development may be...
Hypoplasia is a disorder of intrauterine development that can affect almost any organ. The reason for its development may be the use of medications, severe illnesses suffered during pregnancy, or exposure to harmful factors. Hypoplasia of the nasal bones in the fetus is one of the common types of such disorders, which is a characteristic sign of Down syndrome.
Hypoplasia presupposes insufficient development of an organ; its highest form is aplasia, as a result of which the organ may not be formed at all. Hypoplasia may not always be detected immediately after birth. It often affects organs whose formation occurs during puberty, leading to combined hypoplasia of organs dependent on each other. For example, impaired development of the mammary gland leads to the development of hypoplasia of the genital organs, and hypoplasia of the brain leads to impaired formation of the spinal cord.
Hypoplasia of the nasal bones in the fetus can be detected already during an ultrasound examination during gestation. For up to 20 weeks, possible physiological disorders are not always detected, but pathology of the nasal bones can be diagnosed with accuracy. This fact, discovered during an examination, did not cause any particular concern for a long time until its relationship with Down syndrome was revealed.
The discovery of hypoplasia causes a lot of anxiety among the parents of the unborn baby, since this pathology, being one of the possible symptoms of Down syndrome, entails other signs of this disease - mental retardation, peculiar changes in the child’s appearance and other congenital malformations. According to statistics, deformation of the nasal bones is 80 times more common in children with Down syndrome. Factors contributing to the development of hypoplasia include:
- bruises during pregnancy; exposure to certain types of gamma radiation; prolonged overheating of a pregnant woman; abuse of alcoholic beverages and smoking during pregnancy; poisoning with toxic substances; past infectious diseases (influenza, rubella, toxoplasmosis and others).
The most common type of hypoplasia is considered to be infantilism (impaired proper development of the genital organs). Such hypoplasia, which develops during fetal development, is more typical for women; it is rare in men. A balanced diet, a healthy lifestyle, and walks in the fresh air will guarantee the health of the unborn baby, help boost his immunity and protect him from hypoplasia.
Placental hyperplasia causes and consequences
The placenta is a temporary organ and provides oxygen and nutrients to the fetus. There is an exchange between the blood of mother and child. The thickness of the placenta up to the 37th week of pregnancy corresponds to the period in weeks. So, at 20 weeks its thickness is 20 mm, and at 25 - 25 mm. At 37 weeks, its growth stops, and its thickness reaches its maximum value - 33.75 mm. By the time of birth, the placenta may become somewhat thinner, which is normal.
The main causes of placental hyperplasia
Infectious diseases of the genital organs, such as chlamydia, mycoplasmosis, gonorrhea, STDs, especially syphilis, and infectious diseases of other organs most often cause placental hyperplasia. In a state of ill health, the body cannot control the correct formation of the placenta - the capillaries in it are located chaotically, part of the tissue becomes sclerotic, and in response to this, new capillaries appear. As a result, blood circulation slows down. In patients with diabetes, the synthesis of hormones is impaired, in particular insulin, which is responsible not only for carbohydrate metabolism, but also performs many other important tasks: placental enzymes are inhibited, in response to this, the existing capillaries expand, which causes hyperplasia.
The diagnosis of placental hyperplasia is usually made during the second ultrasound at 18-23 weeks of pregnancy. The doctor sees thickening of the placenta and expansion of the intervillous space. The latter occurs compensatoryly to ensure normal nutrition of the fetus. If the fetus does not lag behind in development, the obstetrician will prescribe treatment that will improve blood circulation in the placenta and the child will be born completely healthy. A woman must be observed by an obstetrician and have diagnostic ultrasounds 2-3 times a month or weekly. This allows you to control the situation.
Why is placental hyperplasia dangerous?
Most often, with placental hyperplasia, the child experiences a lack of oxygen and nutrients. With moderate hyperplasia, natural childbirth is possible; with pronounced hyperplasia, the child is too weak to be born on his own. Such children are born with low weight, malnutrition, and manifestations of hypoxia. Modern medicine is able to provide them with adequate care, but the risks of some complications persist for about a year.
Almost all pregnant women with placental hyperplasia experience fetoplacental insufficiency (FPI). This condition cannot be cured, but can be compensated for by taking special medications that improve blood circulation in the placenta. Intrauterine growth retardation (IUGR) of the fetus is a consequence of placental insufficiency and occurs only with pronounced FPI. The degree of gold reserves is also different. With timely treatment, children are born underweight, but within a year they “catch up” with their peers in development.
Oligohydramnios or polyhydramnios of varying degrees are diagnosed in more than half of women with placental hyperplasia. Both conditions can be unsafe for the fetus. With pronounced oligohydramnios, curvature of the skeletal bones and fusion of body parts are observed. Polyhydramnios in this regard is less dangerous, but can provoke other complications of pregnancy, such as leakage of water or premature birth.
Intrauterine fetal death due to placental hyperplasia occurs extremely rarely, mainly in women who refuse treatment. It is not the hyperplasia itself that is dangerous, but the complications that thickening of the placenta entails. Timely treatment can fully or partially compensate for the lack of nutrients. Children are born healthy if there are no other reasons that could cause fetal pathology.
Placental abruption at different stages of pregnancy
One of the possible complications of pregnancy is placental abruption. In the first three months of pregnancy, it is easiest to maintain a pregnancy. On an ultrasound, the doctor sees that everything is fine with the child and the patient is prescribed hemostatic therapy.
Abruption in mid-pregnancy is characterized by pain and high tone of the uterus. Fetal movements become very noticeable. This happens because the child feels a lack of oxygen and physical activity increases blood flow, compensating for hypoxia.
In the last months of pregnancy, placental abruption occurs most often. In addition to pain and tension in the uterus, the woman feels increased fetal movements. This condition is accompanied by bleeding and is poorly tolerated by the fetus.
The placenta no longer grows, the baby’s connection with the mother is gradually lost, and in most cases an urgent birth is required. If the detachment is partial and does not grow, and the placenta is located on the posterior wall, then there is a greater chance of stopping the bleeding.
In case of multiple pregnancy or polyhydramnios, the walls of the uterus are stretched. During the birth of one fetus, intrauterine pressure drops sharply and placental abruption occurs. At this time, the connection between the mother and the fetus remaining inside is lost. This condition is easily identified by any obstetrician and complications can be avoided.
If the placenta is on the anterior wall of the uterus, then during movement the uterus contracts and detachment of the “baby place” may occur.
The consequences of this phenomenon can be fatal: in 15% of cases the child dies. A subsequent pregnancy may proceed with the same pathology, and if the uterus is amputated, there is no chance of getting pregnant at all.
Causes of placental edema during pregnancy
Placental edema is caused by a number of diseases. Pathological development of a child's place can lead to intrauterine fetal hypoxia and premature birth.
The placenta is formed during pregnancy. It develops mainly from the chorion and lining of the uterus. Its development continues up to 4 months. Through the tissues of the placenta there is an exchange of necessary substances and the flow of oxygen from the mother to the fetus. Swelling of the placenta during pregnancy occurs due to inflammatory processes.
Basic functions of a child's place.
- The exchange of oxygen, which comes from the blood of the pregnant woman and enters the body of the fetus, is returned by carbon dioxide.
- Enrichment of fetal nutrition, removal of metabolic substances.
- Protective functions.
- Endocrine secretion.
The development and growth of the placenta occurs along with the fetus. Pathological changes can indicate violations of its functions, which can lead to serious consequences. Swelling of the placenta occurs against the background of infectious, viral diseases, diabetes mellitus, Rh conflict, gestosis and other problems. Pregnant women with the following pathologies are at risk.
Edema due to Rh conflict
A Rh factor conflict is possible only if the mother has a negative Rh factor and the fetus has a positive blood factor. In this case, swelling of the placenta occurs, and in severe cases, edema syndrome of the newborn develops.
Edema in diabetes mellitus
Swelling of the placenta in diabetes mellitus is observed from 20-25 weeks of pregnancy. Blood flow in the placenta and fetus is examined. Changes in the child's place are characterized by an increase in mass and thickening of the organ.
Edema with syphilis and toxoplasmosis
Damage to the placenta is characterized by swelling and proliferation of tissue cells. It increases in size, hyperplastic processes develop, that is, the epithelium grows in the placental cells.
Toxoplasmosis is a parasitic disease. When chronic, it is practically not dangerous to the fetus. In case of infection with toxoplasmosis during pregnancy, the placenta increases in size and resembles the swelling of a hemolytic disease. Microscopic examination reveals inflammation of the vessel walls.
External and hidden swelling
Physiological edema appears in late gestation. They may be normal or pathological. Normal swelling does not pose a health risk. Hidden edema is the first sign of the development of gestosis, which can lead to a threat to the life of the mother and fetus. Preeclampsia causes swelling of the placenta, blood pressure rises, protein is found in the urine, and calcifications form. Hidden edema provokes an increase in weekly weight by 300 g.
Diseases of the mother and fetus - pathology of the placenta: complications
Pathology of the placenta
The following are possible complications of pathology of the placenta, diseases of the mother and fetus:
Bleeding
- Sometimes labor can be so difficult that heavy vaginal bleeding may occur during or after the process.
- Bleeding is usually not accompanied by pain, although some women may experience uterine cramps during bleeding.
- Bleeding from the placenta can increase the risk of premature rupture of membranes, which leads to preterm labor.
Placenta accreta
- Occurs when placental tissue grows too deeply into the uterus, attaching to the muscle layer.
- This leads to difficulty in separating the placenta from the uterine wall during childbirth.
- This complication can cause life-threatening bleeding.
Fetal dystocia
- This complication indicates an atypical size or position of the fetus, which leads to a difficult birth.
- Treatment is by physical activity to reposition the fetus or by caesarean section.
Vasa praevia
- Occurs when the membranes connecting the umbilical cord and placenta overlap or are within 2 cm of the inner cervix.
- Bleeding accompanying Vasa praevia jeopardizes, first of all, the life of the child, not the mother.
Fetal anemia
- Fetal anemia occurs when the number of circulating red blood cells and hemoglobin in the fetus falls below normal levels.
- Placental abruption. This is a condition in which the placenta separates from the uterus, disrupting the baby's blood and nutritional supply and can endanger the life of the unborn baby.
Infarctions in the placenta
- These are areas of non-living tissue in the placenta that cause decreased blood flow.
- They may appear with hypertension, which is caused by pregnancy.
In addition, pathology of the placenta can have a significant emotional impact on a pregnant woman and even cause depression.
Swelling of the legs during pregnancy
If swelling of the legs occurs during pregnancy, the treatment may be as follows:
If your legs are swollen, painful, or red, you should consult a doctor. Perhaps in this situation the development of thrombosis began.
To avoid leg swelling during pregnancy, you should try to monitor your body weight and adhere to a balanced diet. To prevent leg swelling during pregnancy, you should eat less fatty foods and drink more water, which will help improve kidney function and remove excess fluid from the body.
To get rid of swelling of the legs during pregnancy, you need to include in your diet foods that help maintain the functioning of the genitourinary system and have good diuretics. These include citrus fruits, apples, celery, parsley (but not very much), watercress. Eat more garlic and onions. They help improve blood circulation.
What to do about edema during pregnancy? Limit your intake of salt, food additives, and processed foods that contribute to fluid retention. Include in your diet foods containing vitamins E and C. They are found in tomatoes, potatoes, broccoli and potatoes, red and green peppers, melon, citrus fruits, and strawberries. And also in soybean and corn oil, in wheat germ oil. Sunflower seeds, sprouted wheat and corn, cashews and nuts, almonds are rich in vitamin E.
Swelling during pregnancy, treatment means rest. When resting, try to place your feet above the level of your body. If for some reason you have to stand for a long time, it is recommended to step from foot to foot. This improves blood flow.
Using a bucket of water where your feet are placed, with a few drops of any aromatic oil. Cypress oil has a positive effect on blood circulation. Lavender and chamomile oil relieve tension and fatigue.
Cabbage leaves, which are first cooled in the refrigerator and then applied to the feet and swollen areas of the legs, can help relieve swelling and remove excess fluid. Keep it for as long as possible. And then change to new ones.
What to do about edema during pregnancy? Taking homeopathic remedies such as sodium chloride will help get rid of them. It is taken one tablet or two tablets under the tongue at a dosage of 30c up to four times a day. The course is five days. Admission only as prescribed by a doctor.
Dandelion roots, from which tea is made. Although it should not be taken with increased cholecystitis.
Alternative medicine, such as acupuncture, helps restore the balance of internal energy and improves kidney function and blood circulation.
Hypoplasia of the placenta.
Girls, I had a scheduled ultrasound today, thank God our son is fine, weight 1800 kg, gestational age 32-33 weeks.
There is one BUT. I was diagnosed with “placental hypoplasia.”
Please tell me - who has encountered this, and how did you complete your pregnancy (did you go beyond the full term or not)? If anyone can tell me anything about this, I will be very grateful to you all.
Doppler: - umbilical cord artery RI: 0.75 normal limit
— uterine artery on the left RI: 0.65 reduced
— uterine artery on the right RI: 0.62 reduced
On the pages of the Children Mail project. Ru comments that violate the legislation of the Russian Federation, as well as propaganda and anti-scientific statements, advertising, insults to the authors of publications, other discussion participants and moderators are not allowed. All messages with hyperlinks are also deleted.
The accounts of users who systematically violate the rules will be blocked, and all messages left will be deleted.
You can contact the project editors using the feedback form.
Possible abnormalities in organ development
Pathologies of the placenta are not uncommon. But there is no need to worry in advance. Of course, some disturbances in the structure and location of an organ can harm the child, but this does not apply to all pathologies of this organ.
In addition, even serious problems can be solved thanks to timely medical care. Therefore, if any symptoms of trouble appear (bleeding from the vagina, abdominal pain, high blood pressure), you need to inform your doctor about them in order to exclude the development of pathology.
The main pathologies of the placenta are:
- lag or, on the contrary, rapid maturation of the organ;
- detachment before the onset of labor; Read more about placental abruption→
- pathological growth or, on the contrary, extremely slow growth of the organ;
- formation of intraplacental blood clots;
- violation of the lobular structure of the organ;
- inflammatory process;
- accretion or too tight attachment to the wall of the uterus;
- thickening of the placenta;
- low localization of the organ (at the pharynx of the cervix);
- placental tumors;
- placental infarction.
All of the above pathologies can develop due to the following reasons:
- toxicosis;
- diabetes;
- atherosclerosis;
- gestosis;
- infections, including influenza and toxoplasmosis;
- Rh incompatibility between mother and fetus;
- severe anemia;
- pregnancy after 35 years;
- past abortions;
- stress;
- bad habits;
- acute and chronic somatic diseases of women;
- excess or, on the contrary, insufficient body weight of the expectant mother;
- congenital fetal defects.
To successfully treat placental pathologies or prevent their development, it is necessary to eliminate the factors contributing to these disorders.
So, the outcome of pregnancy and the health of the unborn child largely depend on the normal state of the placenta. In turn, organ pathologies negatively affect the development of the fetus, in particular provoking its mental retardation and the formation of defects of internal organs.
Therefore, every woman carrying a pregnancy should be observed by a doctor and undergo routine ultrasound examinations.
In addition, she needs to take care of her own health and report to a specialist about all ailments and negative changes in well-being.
Often, it is an attentive attitude towards yourself that allows you to prevent the development of complications that an experienced doctor might have missed at the initial stage.
especially for Mama66.ru
Pathology of the placenta: prevention
Pathology of the placenta: prevention
Prevention has a huge role in any condition, and even more so during pregnancy. The main preventive measures to combat placental pathologies should be listed:
- Reducing the number of abortions - curettage, curettage, by preventing unwanted pregnancies: the use of contraceptives.
- Treatment of inflammatory, hormonal and infectious diseases of the female reproductive system.
- Limiting the use of drugs to maintain pregnancy, as well as surgical delivery without justified reasons.
- The failure of the uterine scar after previous births must be corrected outside of pregnancy using reconstructive transvaginal plastic surgery.
- Reducing the frequency of use of assisted reproductive technologies ( IVF ).
- Conducting conversations and consultations with women on the risk of pregnancy after 35 years .
- Treatment of extragenital pathology in women.
You should also know that when uterine fibroids are diagnosed in a woman who wants to become pregnant, it must be removed.
Possible problems related to the placenta
During pregnancy, the placenta and its condition are influenced by various factors. Possible causes of violations:
- maternal age (after 40 years, the risk of pathological changes and disorders of the basic functions of the placenta increases);
- premature rupture of the amniotic membrane of the fetus (leading to the development of placental pathology);
- multiple pregnancy increases the risk of placental structural disorders;
- high blood pressure;
- bleeding disorder (increased or inadequate hemostasis causes problems with the placenta);
- previous surgical interventions on the uterus (caesarean section, corrective and other operations increase the risk of pathology);
- problems with the baby's place during previous pregnancies;
- smoking or consuming other substances harmful to the health of the placenta;
- trauma (a fall or blow to the abdomen plays a significant role in problems with the placenta).
The most common problems of human afterbirth are:
- Placenta previa. Normally, the placenta is located near the cervix on its lateral or posterior wall. As the uterus grows and its layers stretch, the attachment site moves upward, which corresponds to the fundus of the uterus. If the point of attachment of the placenta is in an incorrect position in the cervix and extends onto it, then the woman experiences intense uterine bleeding from the open spiral vessels of the uterus. This is very dangerous, so the doctor refers pregnant women with this pathology to a caesarean section.
- Detachment. In this case, both a small and a significant part of the placenta can detach. In this case, the process of oxygen delivery to the fetus is disrupted, which leads to the development of intrauterine hypoxia.
- Placental accretion. In some cases, excessive penetration of placental elements into the uterine wall occurs. This leads to disruption of the process of separation of the placenta during childbirth and uterine bleeding. For this pathology, doctors often recommend cesarean section.
- Retention of the placenta in the uterine cavity. The etiology of this disorder is rapid compression of the cervix after childbirth, creating a mechanical obstacle to the release of the placenta. In some cases, it can be combined with accretion and requires emergency intervention due to the risk of blood loss.
Typical symptoms accompanying these disorders:
- intense vaginal bleeding;
- stomach ache;
- back pain;
- uterine contractions.
The listed signs require urgent consultation with a doctor, because... can lead to serious complications during pregnancy, dangerous to the fetus and the female body. Is it possible to reduce the risk of placental disorders? Most of these pathologies are unpredictable, but following certain recommendations will help to significantly reduce risk factors.
Prevention Tips:
- quitting smoking and alcohol;
- taking any medications only after consulting a doctor;
- regular visits to the obstetrician for examination and ultrasound;
- proper nutrition and daily routine during pregnancy.
Pathology of placenta and umbilical cord attachment during pregnancy: pathogenesis
Pathology of the attachment of the placenta and umbilical cord during pregnancy
The placenta forms inside the endometrium. This functional layer during pregnancy is called the decidua. At the 40th week of gestation, such a membrane During childbirth, it separates, the endometrial vessels contract, and this process helps to avoid uterine bleeding.
- If the expectant mother develops inflammation in the uterus, dystrophy, or cicatricial changes in the mucous membrane occur, then the spongy layer of the placenta is replaced by connective tissue.
- It becomes overgrown with villi and during childbirth will not be able to spontaneously separate from the uterus.
In obstetrics, there are several pathologies of the placenta and umbilical cord attachment during pregnancy. Such anomalies vary in the depth of placental ingrowth into the deep layers of the uterus, as well as in the prevalence of placental tissue accretion:
Tight placement of the placenta:
- This is the most popular type of pathological attachment of placental tissue to the uterus.
- It was described above that chorionic villi can reach the basal layer and are well attached to the walls of the uterus along with the placenta.
Low placental attachment:
- A common pathology, occurs in 15-20% of cases .
- If it appears after 28 weeks of pregnancy, the doctor will already diagnose “placenta previa ,” since in this case the baby’s place partially covers the uterine os.
- But it is very good that in only 5% of pregnant women, the low location of the placenta persists up to 32 weeks . And only in 1/3 of them—that’s 5%—the placenta will remain in this position by 37 weeks .
Placenta previa:
- Reaches the internal pharynx or overlaps it.
- Occurs in pregnant women a second or more times.
- More often occurs if there have been abortions or gynecological operations after childbirth.
- In addition, various tumors and developmental anomalies of the uterus contribute to the development of such pathology.
- This disease can lead to severe bleeding and difficulties with childbirth.
Placenta accreta (true accreta):
- The chorionic villi pass through the decidua into the myometrium.
- The prevalence of increment in depth can be either insignificant or quite pronounced.
- Penetration of villi occurs through all layers of the uterus, right up to the serous membrane.
- The most severe consequences in the form of pathological attachment of the placenta most often occur with pathological changes in the uterus.
Abnormal and pathological attachment of the umbilical cord is primarily associated with defective implantation of the umbilical cord. As a result, the umbilical cord is located outside the trophoblast region. So the result of this pathology are:
- Membranous umbilical attachment - the umbilical cord is attached to the membranes of the fetus.
- Marginal attachment - the umbilical cord is attached to the edge of the placenta, and not to its center.
- A single umbilical cord artery in half of the cases can be combined with fetal malformations: heart, kidney, urinary tract, genitals, musculoskeletal system. This pathology occurs 3-4 times more often with such abnormalities as multiple pregnancies and diabetes mellitus in the mother.
It is worth noting that if the placenta is tightly attached, active uterine postpartum bleeding does not occur, since the “baby place” is not separated from the walls of the uterus. If attachment is incomplete, then blood loss can be intense.
Gestosis during pregnancy
Preeclampsia is one of the most dangerous complications that occurs during pregnancy and goes away after childbirth. This serious disease is one of the top three leading causes of death for expectant mothers and is diagnosed in almost 30% of pregnant women.
Preeclampsia during pregnancy is often called late toxicosis and is usually detected in the 3rd trimester. It can be accompanied by dysfunction of any vital organs, however, most often the vascular system suffers.
The placenta of pregnant women with gestosis begins to produce special substances that provoke the formation of micropores on the walls of blood vessels. Thanks to them, plasma fluid and protein penetrate into the body tissues. This causes severe swelling. Since the kidney vessels also allow protein to pass through, it is easily detected during a general urine test. Timely testing allows you to identify gestosis in the early stages of development, which greatly facilitates its treatment
Source
Diagnostics
To make an accurate diagnosis, various laboratory tests are performed on the fetus and placenta. Hypoplasia is diagnosed as a result of:
- ultrasound examination (detects intrauterine growth retardation); cardiotocography (determines the child’s heart rate); Dopplerometry (determines deviations in placental circulation); genetic screening to identify chromosomal abnormalities that provoke the development of primary hypoplasia.
Only in combination do all these diagnostic methods give a complete picture of the state of the placenta at a given stage of pregnancy. If hypoplasia is suspected, immediate treatment is started. The sooner the pathology is detected, the greater the chances of a successful outcome of events.
Keep in mind. If the expectant mother is a petite woman, then her placenta will be one. In this case, hypoplasia is not diagnosed.
Placenta size: normal
When do we talk about placental hypoplasia? There are indicators that are the norm. If screening studies show deviations from these figures, additional diagnostics are performed to confirm or refute the diagnosis.
- 14 weeks: thickness on average should be 12-22 mm (average - 16 mm);
- 20 weeks: 16-28 mm (average - about 21 mm);
- 31 weeks: 24-40 mm (average norm - 31 mm);
- Week 38: 27-45 mm (average - 34 mm).
And if placental hypoplasia is successfully treated for 32 weeks, since the mother will have time to stay in the hospital and go into labor completely healthy and without pathologies, then at week 38 the course of therapy will hardly be able to be carried out. However, this is the very period when the baby can be born completely healthy and full-fledged.
. With this diagnosis at this stage of pregnancy, in most cases a cesarean section is performed.
Villous mole
Villous mole (Mola villosa) is a pathological condition of the placenta often found in cows. Villous mole manifests itself in villous hypertrophy and hyperplasia, which gives the placenta a cauliflower shape. The villi become soft and long (up to 2 cm) or dense, fibrous. The villi either do not come into close contact with the maternal part of the placenta or, on the contrary, grow together with it, causing retention of the placenta. In a foal on the miscarriage placenta, hypertrophy of individual chorionic villi can be observed; which, among normal villi, stand out for their size and have the appearance of either individual or collected in groups of thread-like protrusions up to 1 cm high, which have a pasty consistency, or fibrously compacted mushroom-shaped, sometimes calcified growths.
Symptoms and diagnosis
In the presence of a thin placenta, the supply of components necessary for intrauterine life to the child is reduced, which results in a clear slowdown in fetal development. In many cases, the disease is asymptomatic and is detected only during a routine ultrasound scan.
. If the ultrasound results show some abnormalities in fetal development, then doctors prescribe additional studies.
Main symptoms of the disease:
- Slow fetal development. The basis for this conclusion is the results of an ultrasound examination, during which it will be detected that the weight of the fetus and its growth are inappropriate for the timing.
- Decreased baby's heart rate. Detected by cardiotocography - CTG.
- The level of blood flow in the placenta is significantly reduced, which is determined using the Doppler method.
If a decrease in the size of the embryonic organ is not accompanied by the above symptoms, then placental hypoplasia is unlikely. During the formation of the placenta, some minor deviations may occur, which in no way affect the intrauterine development of the baby
. It should also be taken into account that in women giving birth with a miniature body structure, the size of the placenta will be much smaller than in expectant mothers with a large build, so its development must be monitored over time.
White placenta infarction
In cows and goats, changes in the fetal placenta occur during abortion, followed by maceration or mummification of the fetus. Individual or all placentas located in one of the horns lose their villous structure; in their place, homogeneous, light yellow or dark yellow, cake-shaped plaques with a brown tint are formed. Upon examination, their placental surface is smooth and shiny, with a doughy consistency. Plaques on the cut are homogeneous or consist of two layers. The vessels approaching them are obliterated, in fresh cases we note their thrombosis, sometimes they are dilated, and there are diffuse hemorrhages along the vessels. Histological examination reveals necrosis of placental tissue, and only in places there are foci of cell accumulations in various stages of decomposition. The blood vessels are dilated and filled with decaying formed elements. In necrotic areas, accumulations of hemosiderin and lime salts are released (L.G. Subbotina). White placental infarction is often found in fetuses of stunted piglets. Due to heart attacks, animals develop mummification of fetuses.
Treatment of thin placenta
The basis for successful treatment of placental hypoplasia is timely diagnosis and detection of the cause of the disease.
After all components of the disease have been clarified, the woman in labor is prescribed treatment, which should take place exclusively in a hospital.
First of all, doctors prescribe medications that stabilize blood flow in the placenta, after which they concentrate on treating the disease that causes hypoplasia.
A number of measures are also carried out to normalize the child’s heart rate and monitor his activity and movements.
If the placenta is significantly thin and the baby’s condition worsens, doctors may decide to give the pregnant woman an emergency birth by cesarean section. However, it is worth noting that it comes to this extremely rarely, and with modern medications and careful monitoring of the fetus, treatment of placental hypoplasia is very successful, pregnancy proceeds according to the terms, childbirth is carried out without complications, and the child is born absolutely healthy.
One of the most dangerous pathologies of pregnancy is placental hypoplasia - its reduction, underdevelopment, and immaturity. This is fraught with the most undesirable consequences for the child.
. After all, it is the placenta that is the very organ that helps him survive in the womb: it nourishes him, supplies him with breathing, and provides him with favorable conditions for full development.
If she cannot function normally, the baby may die. To prevent this from happening, appropriate and timely measures are needed, both from doctors and from the expectant mother.
Diffuse placenta
Diffuse placenta (Placenta diffusa) is found in cows and is not separate placentas, but continuous villous tissue that more or less evenly covers the entire surface or only a limited area of the chorion. The villi of this placenta often acquire changes characteristic of a villous mole. The presence of a diffuse placenta must be taken into account by the veterinarian when determining the timing of pregnancy by palpating the placentas. Abortions due to diffuse placenta have not been registered (L.G. Subbotina).
What it is?
Insufficient development of an organ is called hypoplasia. This condition is characterized by a decrease in mass, diameter and thickness
. Doctors also often call such a placenta “thin,” emphasizing that with hypoplasia, the thickness of the placental tissue also changes significantly.
Doctors identify several clinical variants of this condition.
- Primary hypoplasia. Associated with an initially disrupted process of implantation of a fertilized egg to the uterine wall due to certain reasons. In this situation, from the very first days of pregnancy, the placental tissue is small
. The functioning of the organ is usually impaired. - Secondary hypoplasia. In this case, the initial formation of placental tissue was correct, and all changes appeared later. Adverse symptoms with secondary hypoplasia appear, as a rule, not at the earliest stages, but already in the second half of pregnancy.