- Mom's health
There were times when heart disease was the cause of infertility—it was absolutely forbidden for such women to give birth. Now, thanks to modern methods of diagnosing and treating diseases of the cardiovascular system, “heart-women” can carry and give birth to a healthy baby without risking their lives. Of course, such a pregnancy requires special attention, both from the expectant mother herself and from doctors, but if certain rules are followed, a favorable outcome is guaranteed.
The increase in the number of women with heart defects and planning pregnancy has recently been associated with many factors: early diagnosis of such diseases has now begun, heart surgery has become possible, new methods of preserving difficult pregnancies have appeared, advances in medicine and medical practice have given women with cardiovascular diseases confidence in the ability to bear and give birth to a child.
Heart disease - what is it?
Heart disease is a congenital anomaly with defects in the structure of the heart muscle or large vessels.
CHD is characterized by impaired blood circulation in the heart cavity, large and small circles.
Cardiac anomalies, in turn, have a classification and are divided into types.
In addition to the congenital defect, there is an acquired type of the disease. It accounts for no more than 5% of cases, unlike congenital heart disease.
It is characterized by disruption of the heart valve as a result of infectious processes, injuries and visceral lesions.
Symptoms and signs
Sometimes a baby's cry for no reason may indicate the presence of a congenital heart defect.
When a baby develops a congenital myocardial defect, the symptoms of the disease appear not only as they grow older, but also in the first days and even hours after birth.
Signs of pathology formation include the following symptoms:
- Change in skin tone: bluishness or pallor. The nasolabial triangle stands out especially clearly during breastfeeding.
- Frequent regurgitation of milk by the baby during breastfeeding.
- Periodic episodes of shortness of breath or persistent breathing problems.
- Unreasonable occurrence of bradycardia or tachycardia.
- Excessive sweating.
- Restlessness or weakness throughout the body at the time of attachment to the breast for feeding.
- Swelling in the lower extremities.
- Slow weight gain by the baby.
- Screaming for no specific reason.
If such signs are detected, the parents of the baby should not hesitate. You should immediately consult a doctor. The sooner treatment begins, the greater the child’s chances of recovery.
Is it possible to give birth
During pregnancy, the load on the heart increases. For example, in the last trimester there is an increase in body weight (about 10 kg), and an increase in water level by an average of 4.8 liters.
An increase in sodium occurs from the 10th week of gestation. The blood circulation changes, a branch of the uteroplacental blood flow is added, which requires a certain amount of blood.
All these natural processes negatively affect the course of pregnancy of the “heart”.
Cardiac pathology is not an absolute contraindication to pregnancy. Such pregnant women are at risk of developing complications associated with the peculiarities of the course of pregnancy.
They are regular “clients” of the cardiologist and the ultrasound diagnostic room.
Thanks to modern medicine, congenital heart disease in women is operated on, the organ anomaly is corrected, and the patient leads a normal life.
An inoperable heart defect may prevent you from planning a child.
Three critical periods
- 10-12 weeks of gestation. The first manifestations of rheumatic complications. During this period, the issue of termination of pregnancy according to indications, or its prolongation, is decided.
- 26-32 weeks of gestation. Due to the increased load on the heart muscle, the patient is treated in a hospital setting;
- 37-40 weeks of gestation. A pronounced overload of the cardiovascular system develops. Quite often, labor with congenital heart disease occurs earlier than expected.
Heart defects that appeared during life
Effective treatment of infectious diseases has reduced the incidence of complications such as heart damage. During pregnancy, acquired heart defects occur only in 6% of cases. Most often they are a consequence of rheumatism, but sometimes they develop under the influence of the following pathologies:
- systemic lupus erythematosus;
- endocarditis;
- atherosclerosis;
- syphilis;
- scleroderma.
The mechanism of damage to valves or vascular openings is associated with an inflammatory reaction. It leads to sclerotic deformation and shortening of the valve. This is how its deficiency develops. Sometimes the consequence of inflammation is stenosis of the opening, which develops as a result of narrowing of the lumen.
Mitral stenosis
Most often it develops as a consequence of infective endocarditis; it takes 2-3 years after the illness to develop.
Clinically, the pathology is manifested by shortness of breath due to stagnation of blood in the pulmonary circulation. At first it only bothers you during exercise, but later it appears at rest.
Pregnancy can be complicated by gestosis, the threat of premature termination, hypochromic anemia and placental insufficiency. In the later stages, pulmonary hypertension and pulmonary edema may appear. At 14, 20-32 weeks, an exacerbation of rheumatic fever may occur.
Treatment is carried out with courses of benzylpenicillin, as well as glucocorticoids and non-steroidal anti-inflammatory drugs. If the gestation period is no later than 28 weeks, surgical intervention - commissurotomy - can be performed. It is recommended for hemoptysis, pulmonary edema and liver enlargement.
Mitral valve insufficiency
Incomplete closure of the valve leaflets occurs, and part of the blood flows back into the atrium during cardiac contraction. The cause of the development of the defect is considered to be rheumatism and atherosclerosis.
Manifestations of pathology during pregnancy are nonspecific. This may be increased fatigue, shortness of breath, pulmonary asthma. In severe cases, pulmonary edema may develop. Pregnant women are characterized by swelling in the legs and hepatomegaly.
Pregnancy may be complicated by the following conditions:
- gestosis;
- bleeding;
- toxicosis;
- threat of interruption;
- anomalies of labor.
Mitral valve insufficiency is often corrected by valve replacement. This requires the use of anticoagulants throughout the entire gestation period to reduce the risk of thrombotic complications.
Aortic stenosis
The most common cause is rheumatism. But damage to the aortic opening rarely occurs in isolation. Most often it is combined with mitral stenosis. Sometimes the pathology is a consequence of infective endocarditis.
Aortic stenosis is asymptomatic for a long time. Only a 50% decrease in blood flow leads to the appearance of clinical signs of cerebrovascular accident:
- dizziness;
- nausea;
- fainting.
Later, shortness of breath bothers me. Pregnancy against the background of a defect is complicated by gestosis, toxicosis and placental insufficiency.
The main goal of the therapy is to alleviate the patient’s condition, but it is difficult to significantly influence the condition with medications. It is necessary to replace the valve before pregnancy or after delivery.
Aortic valve insufficiency
Incomplete closure of the valve leaflets leads to reverse flow of blood from the aorta into the ventricle. The cause of damage to the valvular apparatus is rheumatism, less often - chest injuries, systemic lupus erythematosus, rheumatoid arthritis.
Clinical manifestations of deficiency may not appear for 10-15 years. The exception is acute inflammatory processes leading to the formation of a defect.
The prognosis for pregnancy is favorable in the absence of signs of heart failure and rhythm disturbances.
Tricuspid stenosis and insufficiency
Tricuspid valve stenosis rarely occurs as an independent defect. It is usually combined with damage to other parts of the heart, and sometimes with tricuspid insufficiency.
Tricuspid valve defects lead to serious pregnancy complications. If before conception there was hypertrophy of the right parts of the heart, then with an increase in the volume of circulating blood, these processes intensify, the ventricle and atrium dilate. This shows up:
- bulging neck veins;
- stagnation of blood in the liver;
- ascites;
- generalized edema.
Later atrial fibrillation joins. This condition is very difficult to treat and often becomes an indication for termination of pregnancy or early delivery by cesarean section.
Congenital heart defects during pregnancy, as well as acquired ones, require close attention from a doctor. Therefore, women need hospitalization three times during their entire period: at 12 weeks, at 22-24 and before giving birth at 36 weeks, in order to assess the condition and choose delivery tactics. In case of severe heart failure, a cesarean section is indicated, and in some cases, childbirth is carried out through natural means, but with the period of pushing turned off. This is done by applying obstetric forceps.
Forms of the disease
- Valve insufficiency. Congenital anomaly of the heart valve (1 or more). When several valves are involved, a combined defect occurs. The edges of the valve do not fit closely together, and blood enters through the resulting gap.
- Heart valve stenosis. Thickening of the walls prevents full opening, and the heart muscle does not receive the required volume of blood;
- Combined defect. Stenosis and insufficiency were detected on one valve.
There are about 50 types of heart defects, but none is an absolute contraindication to pregnancy and childbirth.
During the period of pregnancy planning, a woman undergoes a large number of studies, where the result says that pregnancy is allowed or prohibited.
How to plan a pregnancy with heart defects
Modern medicine has quite effective methods that allow us to calculate the degree of risk associated with pregnancy and childbirth in women with heart defects. With their help, doctors help a woman determine the optimal time for conception or decide the fate of an unplanned pregnancy.
The most important method for assessing the state of the cardiovascular system in case of heart disease is ultrasound of the heart - echocardiography. It is harmless and helps to objectively assess the condition of the cavities, valves and openings of the heart. An auxiliary role in the diagnosis of heart defects is played by electrocardiography (ECG - graphic recording of the electrical activity of the heart), phonocardiography (PCG - graphic recording of cardiac sound phenomena) and Dopplerography (ultrasound, which allows assessing blood flow).
In pregnant women, heart defects account for 0.5 to 10% of all heart diseases. Most often, they have an atrial or ventricular septal defect or patent ductus arteriosus. Women with the above defects usually (with appropriate treatment that compensates for the defect) tolerate pregnancy and childbirth well.
Currently, many women who have undergone heart surgery have the opportunity to give birth. The recovery period after such an operation usually takes 1 year. Therefore, it is in a year that you can plan a pregnancy - of course, in the absence of contraindications (unfavorable results of the operation, the development of diseases that complicate postoperative rehabilitation and reduce the effect of the operation).
It is unnecessary to remind that the question of the possibility of pregnancy and the admissibility of childbirth should be decided individually before pregnancy, depending on the general condition of the woman, the nature of the disease, the severity of the operation, etc. After a comprehensive examination of the patient, the doctor can give a very definite conclusion.
However, even when a woman’s condition is stabilized after surgical (or therapeutic) treatment, pregnancy against the background of an increasing load on the heart increases the risk of recurrence of the underlying disease (a previously compensated defect may become decompensated) - this is another argument in favor of the need for consultation with a doctor and medical supervision before and during during pregnancy, even if the woman herself seems to be healthy and full of strength.
There are severe heart defects with significant circulatory disorders (stenosis of the pulmonary artery, tetralogy of Fallot, coarctation of the aorta, etc.), in the presence of which such dramatic disturbances in the functioning of the cardiovascular system can develop that in 40-70% of cases they lead to the death of the pregnant woman Therefore, with these defects, pregnancy is contraindicated .
Such defects can be inherited, and the likelihood of transmitting the disease to a child is determined in each specific case. (For example, if two or more family members have a heart defect, the likelihood of inheriting it increases.)
In general, the worse the prognosis for the expectant mother and child, the more pronounced the circulatory disorder and the activity of the rheumatic process. In severe heart failure and a high degree of activity of the rheumatic process, pregnancy is contraindicated. However, the issue of continuing pregnancy is decided by the patient and the doctor in each specific case.
Complications of childbirth caused by disease
Possible complications during the gestational period caused by congenital heart pathology:
- late gestosis;
- premature birth;
- high risk of bleeding;
- frequent delivery using ACS;
- high mortality.
If you have a heart defect, you are allowed to give birth on your own if there are no significant hemodynamic pathologies of the circulatory system. This condition is characteristic of minor cardiac anomalies.
In some cases, a pregnant woman is allowed to give birth naturally by blocking the attempts. It is important to note that the child is removed with special tools, careless handling of which can cost the life and health of the baby.
Childbirth takes place in a specialized center. The team consists of the following professionals: anesthesiologist, resuscitator, neonatologist, therapist, cardiologist and obstetrician-gynecologist.
Complications of childbirth with congenital heart disease
- maternal mortality;
- weakness of labor;
- large blood loss;
- coagulopathy;
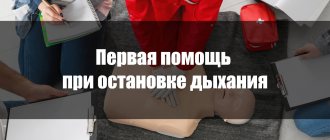
- cardiac arrest;
- ischemic lesions of the heart and brain;
- coma;
- purulent-inflammatory processes.
Consequences for the baby
- 90% confidence that the child will inherit a heart defect (one of the reasons for the development of congenital heart disease in the fetus is heredity);
- fetal hypoxia due to placental insufficiency;
- delayed fetal development;
- perinatal death of a child due to defects incompatible with extrauterine life.
Recommendations for women suffering from heart defects
Remember that the main reason for the unfavorable outcome of pregnancy and childbirth in those women with heart defects, for whom pregnancy is not contraindicated in principle, is insufficient or irregular examination in the antenatal clinic, the lack of comprehensive pregnancy management by an obstetrician and cardiologist and, as a consequence, the insufficient effectiveness of treatment measures and errors in the management of childbirth and the postpartum period.
Recommended:
- try to prevent unplanned pregnancy;
- consult your cardiologist before pregnancy; find out whether you are able to bear a child and what method of delivery you should prepare for;
- if you suffer from congenital heart disease, be sure (preferably before pregnancy) to consult a geneticist;
- find out what regime you should follow so as not to put yourself and your unborn child at risk, how to eat properly, what physical therapy exercises could help you bear and give birth to a child;
- do not miss your appointments with antenatal clinics and appointments with a cardiologist, complete all prescribed examinations on time;
- do not refuse hospitalization and taking medications - because not only your well-being, but also the health and life of your baby depends on how effectively your heart functions.
Features of pain relief for women in labor with heart defects
Vanin L.V. A scheme for managing labor in pregnant women with cardiac anomalies has been proposed:
- From the onset of labor and up to 4 cm of dilation, administer tranquilizers (for example, Seduxen), antihistamines, antispasmodics and analgesics to the pregnant woman.
- At the second stage, the pregnant woman is given medicated sleep for at least one and a half hours.
- Before pushing occurs, autoanalgesia with nitrous oxide and oxygen is performed. The appearance of attempts indicates the cessation of manipulation.
When delivering by caesarean section, epidural anesthesia is used (it is also used during natural childbirth as pain relief).
Spinal anesthesia is contraindicated as it significantly reduces blood pressure.
Preference is given to general anesthesia with the use of a ventilator.
Consequences
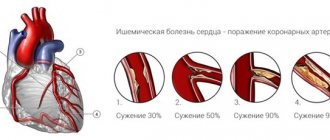
The consequence of untreated congenital heart disease in a newborn may be coronary heart disease.
If treatment is not started on time, there was no exposure to medications, or surgery was not performed, then the baby cannot avoid the consequences.
These children are more likely than usual to develop infections, coronary artery disease, or iron deficiency anemia. Unstable functioning of the heart stimulates the appearance of problems with the nervous system.
The most dangerous complication is endocarditis. It is caused by bacteria entering the heart, which have the ability to infect not only the lining of the heart muscle, but also the kidneys, liver and spleen. To combat this consequence, doctors recommend urgent therapy in the form of antibiotics.
Indications for caesarean section
ACS does not exclude the development of negative consequences for mother and child. When preparing for surgery, special attention is paid to the homeostasis system and the condition of the heart muscle and its valves.
Pregnancy with heart defects - indications for cesarean section:
- Combined insufficiency of the mitral and aortic valves;
- II–III stage of mitral stenosis;
- Endocarditis of bacterial etiology;
- Complications after correction of a heart defect;
- Valve prostheses (including multivalve);
- History of thromboembolism;
- Coarctation of the aorta.
Emergency surgery is performed during increasing fetal hypoxia, during presentation of the “baby place” and during premature placental abruption.
Absolute contraindications to surgical delivery:
- Cirrhosis of the liver;
- Cardiomegaly;
- Blue-type congenital heart disease with a complex course;
- Severe decompensated circulation as a result of cardiac abnormalities;
- Extreme degree of pulmonary hypertension.
Pregnant women with these signs of cardiac anomalies have an unfavorable prognosis at the time of labor and throughout the gestational period.
Author: Elena Yuryevna, obstetrician-gynecologist of the highest category Specially for the site kakrodit.ru
Heart defects. Complications after childbirth
In the first few days after childbirth, a woman may experience complications such as:
- thrombosis;
- bleeding;
- heart failure.
Therefore, you should maintain bed rest in a hospital setting for a week.
After about ten days, you need to undergo tests. Systematic monitoring of this kind after the birth of a child should also be carried out throughout the year.
The required period of hospitalization is at least two weeks. An important condition for discharge of a woman and her child home is mutual satisfactory condition and a guarantee of observation by a cardiologist at the place of residence.
Is it possible to breastfeed a child with heart disease (defects)?
This is possible and even desirable if decompensation did not occur after the birth of the child, and medication was not prescribed by a doctor.
A newborn child will definitely need to be examined for possible pathologies or their potential danger due to the fact that in such children the risk of heart disease increases many times over.
Development of congenital heart disease and treatment methods
In its development, CHD goes through three phases. The stage of the disease matters for the treatment provided. The primary adaptation phase (emergency) occurs with the use of all the body’s reserves to compensate for the dysfunction of the heart. When the body's capabilities are insufficient, the defect can lead to the death of the baby if cardiac surgery is not applied.
If the body copes with an extreme situation, it enters the stage of relative compensation and all systems and organs work with a certain stability. When the body's reserve capabilities are exhausted, the decompensation phase begins. The structures of the heart, blood vessels and lung tissue are no longer able to perform their functions, and heart failure develops.
The operation is usually performed in the compensation stage, when the body has adapted to increased demands. But sometimes surgery is needed urgently at the beginning of the emergency phase, when the baby cannot survive without it. The operation is usually no longer performed in the third phase of the disease. With irreversible changes in systems and organs, it becomes useless.
Not all types of defects can be eliminated with one operation. Sometimes doctors have to do palliative measures aimed at temporarily stabilizing the condition. They allow the child to live until he grows up, gets stronger and can undergo a full-fledged operation without complications and fully recover after it. Before and after surgery, antiarrhythmics, cardiotonic drugs and blockers are prescribed. The main condition for a favorable prognosis of the operation is timeliness.
puzikkarapuzik.com
What is hidden behind the terrible diagnosis?
The phrase “congenital heart defect” in itself is terrifying, and the mysterious abbreviations that the doctor writes in the child’s card can in this case drive parents to panic. However, you should calm down and find out which disorders are characterized by the letter combination of congenital heart disease.
The heart is one of the most important human organs, and its task is to ensure proper blood flow and, as a result, saturate the entire body with vital oxygen and nutrients. Due to the contraction of the heart muscles, venous blood saturated with carbon dioxide enters the lower chambers of the heart - the atria. Passing into the ventricles - the upper chambers of the heart, the blood is again enriched with oxygen and sent to the main arteries, through which it is delivered to the organs and tissues, giving them all the useful substances and taking away carbon dioxide and metabolic products. The blood then passes through the veins and enters the atrium again. The passage of blood from the chambers and its uniform and timely release into the arteries is regulated by muscle valves.
Blood circulation in the body occurs in two directions. The systemic circulation originates in the left atrium and ends in the right ventricle. This vascular pathway maintains the vital functions of all tissues and organs. However, the heart constantly needs oxygen, so the pulmonary circulation connects it only with the lungs, starting from the right atrium, passing through the pulmonary arteries and returning to the left ventricle.
It is obvious that the heart and blood vessels are a clear, impeccably streamlined system, where unimportant details simply do not exist. The slightest error in the functioning of any of the components of the organ can cause disturbances in the body as a whole, and in particularly serious cases, even lead to death. Therefore, improperly functioning heart chambers, untimely opening valves or damaged large vessels are classified as heart defects.
According to statistics, for every thousand healthy babies there are 6-8 children with heart pathologies. Congenital heart disease in newborns is the second most common disease of the cardiovascular system.
Most often, the occurrence of pathologies of the heart and blood vessels is caused by the following reasons.
- Infectious diseases in early pregnancy. Such diseases are especially dangerous in the first trimester, between 3 and 8 weeks of pregnancy, when the baby’s heart and blood vessels are forming. The most insidious disease is rubella, which causes severe damage to the fetus.
- Age and health status of the mother. With age, the body's defenses gradually weaken, and during pregnancy, the endocrine and immune systems are rebuilt in such a way as to maximally support the woman's health, even to the detriment of the unborn child. Therefore, the older the expectant mother and the more chronic diseases she has, the higher the risk of improper formation of the baby’s cardiovascular system.
- Failure to maintain a healthy lifestyle during pregnancy - smoking, drug use, alcoholic beverages, uncontrolled use of medications or working in hazardous industries - negatively affects the body, and primarily the functioning of the heart.
- Heredity. Unfortunately, the tendency to heart pathologies can be transmitted at the genetic level. And if among your maternal or paternal relatives someone has been diagnosed with a congenital heart defect, then the pregnancy must be monitored very closely, since the risk of the disease is extremely high.
No one can give a 100% guarantee that a child will not develop a heart defect. However, the expectant mother is able to minimize this risk. Proper nutrition, giving up bad habits, strengthening the immune system and careful pregnancy planning will ensure the normal development and proper formation of all organs of the unborn baby.
How does pathology manifest itself?
Often, after identifying a child’s heart pathologies, parents are frightened not so much by the diagnosis itself as by the lack of necessary information. The formulations used by doctors often not only fail to clarify the situation, but also create even more fear. Therefore, it is important to roughly understand what is meant by a particular diagnosis.
In total, about one hundred types of congenital heart defects are classified, but the following pathologies are the most common.
- Hypoplasia is insufficient development of one of the ventricles. With this disorder, only part of the heart works effectively. It does not occur too often, but is one of the most serious defects.
- Transposition of the great vessels (TMS) is an extremely severe heart defect, which is characterized by a mirror arrangement of the arteries. In this case, the process of enriching the blood with oxygen is disrupted.
- Obstruction defects. Associated with improper formation of openings in blood vessels. Most often, in children with heart disease, stenosis (abnormal narrowing of blood vessels or heart valves) and atresia (partial closure of the lumen of blood vessels) are determined. Particularly dangerous is coarctation of the aorta, a narrowing of the largest blood vessel in the body.
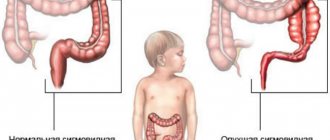
- Atrial septal defect (ASD) is a violation of the development of tissue between the chambers of the heart, as a result of which blood moves from one atrium to another, and the stability of blood circulation is disrupted.
- Ventricular septal defect (VSD) is the most common heart defect. It is characterized by underdevelopment of the tissue wall between the right and left ventricles, which leads to incorrect blood circulation.
Often heart defects are combined with each other, so when making a diagnosis it is necessary to indicate all lesions of the heart and blood vessels. Hence the possible numerous abbreviations in children's cards, which frighten parents so much.
Circulatory disorders primarily affect the color of the skin. Based on this, heart defects are divided into two groups: pale and blue .
Pale or white defects are abnormal narrowing of blood vessels, defects in the septa between the chambers of the heart. Arterial and venous blood do not mix. Children with such pathologies have unhealthy pale skin. Blue heart defects include transposition of the great vessels and tetralogy of Fallot (complex heart defect with vasoconstriction, septal defect and underdevelopment of one of the ventricles). With such disorders, the autonomy of all cardiac chambers is impaired, as a result of which arterial and venous blood is mixed. Because of this, the skin acquires a bluish or grayish tint, which is especially noticeable on the skin of the extremities and in the area of the nasolabial triangle.
In addition to an unhealthy skin tone, the following symptoms of congenital heart disease in newborns are noted:
- severe shortness of breath;
- cardiopalmus;
- fast fatiguability;
- poor appetite, slow weight gain, frequent regurgitation;
- heart murmurs when listening with a stethoscope.
Each of these symptoms separately does not indicate the presence of a heart defect. However, the presence of more than two unfavorable signs requires immediate contact with specialists, since any heart defect leads to serious complications. If mild disturbances in the functioning of the heart and blood vessels can lead to slow development of the child, frequent fainting and dizziness, decreased immunity, then more severe ones at any time can lead to acute heart failure and death. Therefore, if there is a suspicion that there is something wrong with the child’s heart, you should not wait: in this case, every second counts, and the examination must be carried out as soon as possible. Heart disease is especially dangerous because it may not manifest itself in any way in the first year of life. That is why ultrasound of the heart at the age of 6-9 months is included in the list of mandatory examinations for children in the first year of life.