Arterial hypertension is one of the most common diseases of the heart and blood vessels, affecting about 25% of the adult population. It is not for nothing that it is sometimes referred to as a non-infectious epidemic. High blood pressure with its complications significantly affects the mortality rate of the population. Estimates show that up to 25% of deaths in people over 40 years of age are caused directly or indirectly by hypertension. The likelihood of complications is determined by the stages of hypertension. How many stages does hypertension have, how are they classified? See below.
Important! According to the latest estimates from the World Health Organization in 1993, hypertension in adults is defined as a sustained increase in blood pressure up to 140/90 mm Hg. Art.
What is hypertension?
Hypertension (HD) is a chronic disease of the cardiovascular system, which is accompanied by increased blood pressure. leads to dysfunction of the heart, lungs, kidneys, brain, and nervous system. Also called arterial hypertension.
A number of factors contribute to the development of hypertension:
- person's age.
- his weight (being overweight).
- unhealthy diet: eating fatty, fried, salty foods.
- lack of vitamins and microelements.
- bad habits.
- psycho-emotional stress.
- wrong way of life.
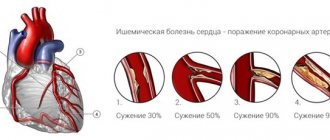
A person is able to influence these factors, which means he can prevent the development of hypertension, but there are factors that are determined by nature and cannot be influenced. These include: advanced age, genetic inheritance. As a person ages, his body ages and organs and blood vessels wear out. Cholesterol platelets accumulate on the walls of blood vessels, which narrow the lumen of blood vessels and lead to increased pressure (blood flow worsens).
Causes of the disease
One of the main and primary reasons is heart and vascular disease. The second most popular reason is obesity, especially at high risk.
Obesity can lead to hypertensive heart disease
Also, the causes of the development of the disease can be:
- Excessive consumption of alcoholic beverages;
- Poor nutrition (large amounts of salt in the diet, fatty, fried and smoked foods);
- Sedentary lifestyle;
- Hard work in hazardous work;
- Frequent stress and nervous tension;
- Lack of rest and sleep;
- Atherosclerotic vascular lesions;
- Endocrine system disorders.
The cause may also be genetic predisposition, serious hormonal imbalances and disorders in the endocrine system.
Characteristics of GB
According to the recommendations of the World Health Organization (WHO), normal blood pressure is with systolic (upper) pressure levels of 120-140 mm Hg. and diastolic (lower) pressure 80-90 mm Hg.
Men and women are equally susceptible to developing this disease. Often hypertension is accompanied by a complication such as atherosclerosis, which mutually complicates the course of hypertension. Such a tandem causes death for a person.
Symptoms
The severity of the clinical picture of hypertension depends on the level of blood pressure rise and target organ damage.
In the initial stages of the disease, the patient begins to complain of the following neurotic disorders:
- episodes of headache (it is most often localized in the back of the head or forehead and intensifies when moving or trying to bend down);
- dizziness;
- intolerance to bright light and loud sound for headaches;
- feeling of heaviness in the head and pulsation in the temples;
- noise in ears;
- lethargy;
- nausea;
- palpitations and tachycardia;
- sleep disorders;
- fast fatiguability;
- paresthesia and painful tingling in the fingers, which may be accompanied by pallor and complete loss of sensation in one of the fingers;
- intermittent claudication;
- pseudorheumatic muscle pain;
- coldness in the legs.
With the progression of the disease and a persistent increase in blood pressure to 140-160/90-95 mm. Hg Art. The patient has:
- chest pain;
- dull pain in the heart;
- shortness of breath when walking fast, climbing stairs, running and increasing physical activity;
- chill-like tremor;
- nausea and vomiting;
- feeling of a veil and flickering of flies before the eyes;
- nosebleeds;
- sweating;
- facial redness;
- puffiness of the eyelids;
- swelling of the limbs and face.
As the disease progresses, hypertensive crises become more frequent and prolonged (can last several days), and blood pressure rises to higher numbers. During a crisis, the patient develops:
- feelings of anxiety, worry or fear;
- cold sweat;
- headache;
- chills, tremors;
- redness and swelling of the face;
- blurred vision (blurred vision, decreased visual acuity, flickering spots);
- speech disorders;
- numbness of lips and tongue;
- bouts of vomiting;
- tachycardia.
Hypertensive crises at stage I of the disease rarely lead to complications, but at stages II and III of the disease they can be complicated by hypertensive encephalopathy, myocardial infarction, pulmonary edema, renal failure and strokes.
Classification of hypertension according to the mechanism of action
According to this principle, WHO divides hypertension into primary and secondary.
- Primary - essential hypertension. A separate disease that occurs due to dysfunction of blood flow in the body.
Primary hypertension has five variants:
- Renal pathology: destruction of blood vessels or the lining of the kidneys.
- Abnormality of the endocrine system: diseases of the adrenal glands serve as an impetus for development.
- Destruction of the nervous system accompanied by increased intracranial pressure. ICP can be the result of trauma or a brain tumor.
- hemodynamic: abnormality of the heart and blood vessels.
- Drug-induced: poisoning due to drug overdose.
- Secondary - symptomatic hypertension. The disease manifests itself as a consequence of some other disease:
- Impaired kidney function, narrowing of the renal arteries, inflammation of the kidneys.
- Thyroid dysfunction - hyperthyroidism.
- adrenal dysfunction - hypercortisolism syndrome, pheochromoblastoma.
- Atherosclerosis, coarctation of the aorta.
Treatment principle
Treatment involves eliminating the main cause that caused the pathology, getting rid of negative symptoms, improving the functioning of the cardiovascular system and normalizing blood pressure. Medicines are prescribed individually, since there is no specific treatment regimen. Depending on the clinical picture, the cardiologist may prescribe a combination of drugs such as:
- ACE inhibitors;
- Diuretics (diuretics);
- Sedatives (calming);
- Calcium antagonists;
- Beta blockers.
Depending on the symptoms present, tranquilizers, drugs for arrhythmia/tachycardia, antispasmodics, drugs to normalize sleep and other medications may be prescribed.
Any medications are prescribed by the attending physician. Do not self-medicate - it could cost you your life
Classification of hypertension by stages
- Stage I - increased pressure, internal organs are not changed, their functionality is not impaired.
- Stage II - increased pressure accompanied by transformation of internal organs: hypertrophy of the left ventricle of the heart, coronary heart disease, modification of the fundus.
At least one of the symptoms of organ dysfunction is present:
- Hypertrophy of the left ventricle of the heart.
- General or segmental angiopathy of the retina.
- Significant protein content in urine, increased creatinine content.
- Vascular examination revealed symptoms of vascular atherosclerosis.
- Stage III - an increase in pressure accompanied by changes in internal organs and their functionality. This stage can lead to the development of a hypertensive crisis.
- On the part of the heart, angina pectoris and failure are observed, and myocardial infarction may develop.
- On the part of the brain, dysfunction of blood circulation in the brain is observed, a stroke and encephalopathy may develop.
- On the fundus side, hemorrhage and effusion are observed, accompanied by swelling of the optic nerve nipple or without.
- Chronic failure is observed on the part of the kidneys.
- On the vascular side, an aortic aneurysm is observed, blockage of the arteries of the upper and lower extremities.
Hypertensive disease primarily affecting the heart
- Temporary loss of consciousness and dizziness occur due to heart rhythm disturbances, as a result of which blood flow to the brain decreases and transient neuronal ischemia occurs
- People say that a hypertensive person is always “ruddy”; the symptom appears due to reflex dilatation of the vessels of the face in response to a narrowing of the blood vessels of the heart.
- High pulse and heart rate.
- Feeling as if “your heart is jumping out of your chest.”
- Patients are often disturbed by inexplicable fear and worry about something.
- The cardiac variant of hypertension is often accompanied by sudden changes in fever and chills.
- Heartbeat.
- Sensations of pulsation in the head.
- Nervousness.
- Swelling of the face and ankles is a consequence of heart failure.
- Visual hallucinations (floaters, stars, etc.).
In addition, tingling of the fingertips and numbness of the limbs may occur.
At the stage of an objective examination of the patient, the doctor performs palpation, percussion and auscultation of the projection area of the heart. With palpation examination, the doctor can determine a pathological cardiac impulse, or pathological changes in the physiological cardiac impulse.
Normally, the cardiac impulse is located in the fifth intercostal space on the right, it is limited and persistent. The “hypertensive” cardiac impulse, in turn, can shift to the left side, diffuse and weak.
During percussion, the doctor will pay attention to the expansion of the absolute and relative boundaries of the heart, which will indicate hypertrophy, and with auscultation, various kinds of pathological sounds can be detected.
To make a diagnosis of hypertension with myocardial damage, the following types of laboratory and instrumental diagnostics are used:
- Electrocardiographic examination of the heart. With the help of which, the doctor can assess the contractile function of the myocardium, the correctness of the rhythm, and conductivity. The presence of ventricular hypertrophy can be diagnosed by the axis deviation on the ECG tape.
- Electrocardiographic study with stress. This diagnostic method is advantageous for establishing the presence of coronary heart disease or angina.
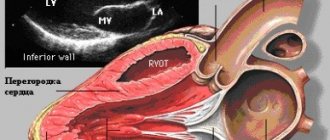
- Ultrasound of the heart or echocardiographic examination of the myocardium and its cavities. Using this method, the doctor can examine “congestive” myocardium, enlarged cavities and the condition of the valves.
- MRI and CT.
- Ultrasound of the cervical choroid plexuses and trunks of the carotid arteries to assess the intima/media complex. This indicator should not exceed 1 mm.
- Biochemistry of blood.
- Holter electrocardiogram monitoring
Additionally, Doppler examination of the vessels of the heart and neck can be used.
Having learned what a hypertensive heart is and about all its dangerous consequences, the patient is obliged to immediately begin treatment for his condition.
It is worth noting that in the case when the patient’s myocardium is damaged, this is already the third stage of arterial hypertension. A competent cardiologist can treat such a patient. The condition for achieving the goal of treatment is the patient’s absolute commitment to it.
First of all, the following are assigned:
- tablets to lower blood pressure (diuretics, beta blockers, calcium inhibitors, ACE inhibitors, etc.);
- cardioprotective agents;
- painkillers;
- nitrates for a more effective reduction in blood pressure in case of concomitant ischemic heart disease and reducing the myocardial need for O2;
- vitamin therapy;
- Exercise therapy, massage. Prescribed if the patient has no signs of cardiac decompensation.
Moreover, the criterion for recovery or remission is a radical change in lifestyle, that is, giving up bad habits, exercising, rest, calm and relaxation.
Heart attacks and strokes are the cause of almost 70% of all deaths in the world. Seven out of ten people die due to blockages in the arteries of the heart or brain.
What’s especially scary is the fact that a lot of people don’t even suspect that they have hypertension. And they miss the opportunity to fix something, simply dooming themselves to death.
- Headache
- Increased heart rate
- Black dots before the eyes (floaters)
- Apathy, irritability, drowsiness
- Blurred vision
- Sweating
- Chronic fatigue
- Swelling of the face
- Numbness and chills in fingers
- Pressure surges
Even one of these symptoms should give you pause. And if there are two of them, then have no doubt - you have hypertension.
How to treat hypertension when there are a large number of medications that cost a lot of money?
Most medications will do no good, and some may even be harmful! At the moment, the only medicine that is officially recommended by the Ministry of Health for the treatment of hypertension is Giperium.
Before
The Institute of Cardiology, together with the Ministry of Health, is conducting a “
no hypertension
” program.
Within the framework of which the drug Giperium is available free of charge
to all residents of the city and region!
Classification of headache by stages of its development
- Initial stage. Belongs to the transient. The main symptom is an unstable increase in pressure during the day (sometimes a simple increase, sometimes jumps). at this stage, the person does not notice the disease, complains about the weather conditions, etc. The person feels normal.
- Stable stage. She is characterized by long-term high blood pressure. It is accompanied by poor health, blurred vision, and pain in the head. Hypertension progresses gradually, affecting important organs and primarily the heart.
- Sclerotic stage. Changes in blood vessels to atherosclerotic occur, and other organs are also affected. The combination of these processes aggravates the overall picture of the disease.
Video
According to the nature of the disease, there is hypertension:
- Benign or slow flowing. The disease develops over a long period of time, and symptoms tend to increase gradually. The patient feels normal. There are periods of exacerbation, which is brief, and remission. This type of headache is treatable.
- Malignant. The disease is characterized by its transience, occurs with severe exacerbations and is life-threatening. This species is difficult to control and difficult to treat.
Hypertensive heart disease [hypertension primarily affecting the heart]
There are five types of hypertensive crises, of which three are the most common: hypertensive cardiac crisis, cerebral angiohypotonic crisis and cerebral ischemic crisis. Rare cases include cerebral complex crisis and generalized vascular crisis. Common to all hypertensive crises is their connection with a “disruption” of the nervous regulation of hepodynamics (due to stress, weather changes, tobacco abuse, physical overexertion, etc.).
Diagnosis of individual clinical and pathogenetic variants of crises, important for the choice of means for their optimal emergency treatment, is based on identifying the clinical symptoms or syndrome that are distinctive for each variant and does not require the use of instrumental research methods.
Hypertensive cardiac crisis is characterized by acute left ventricular heart failure with a sharp increase in blood pressure - usually above 220/120 mm Hg. Art. At lower blood pressure levels, the development of such a crisis is possible with some symptomatic forms of arterial hypertension (renal form, paroxysmal hypertension with pheochromocytoma). Early signs of a crisis include complaints of anxiety that appear against the background of a significant increase in blood pressure. Later, a tendency to tachycardia, weakening of the first heart sound, equalization of the volume of the second heart sound over the aorta and the trunk of the pulmonary artery, and the appearance of shortness of breath are detected. Symptoms of the advanced phase of the crisis (up to pulmonary edema) and its drug therapy are presented in the table. Differential diagnosis is carried out in two directions: firstly, primary heart pathology is excluded - acute myocardial infarction, myocarditis (by ECG, activity of cardiac-specific blood enzymes, etc.), secondly, diseases with symptomatic arterial hypertension, primarily pheochromocytoma, with which the use of ganglion blockers and sympatholytics is contraindicated.
Cerebral angiohypotonic crisis corresponds to the so-called hypertensive encephalopathy, caused by overstretching of the intracranial veins and venous sinuses with blood with increased pressure in the capillaries of the brain, which leads to edema-swelling of the brain and an increase in intracranial pressure. The crisis is based on an insufficient tonic reaction of the cerebral arteries in response to increased blood pressure, causing a “breakthrough” of excess blood flow to the brain under high pressure, as well as hypotension of the cerebral veins, impeding outflow. The main distinguishing symptom of a crisis is a typical headache: initially localized in the occipital region, radiating to the retro-orbital spaces (a feeling of pressure above the eyes, behind the eyes), then becomes diffuse; increases in situations that impede the outflow of blood from the veins of the head (horizontal position, straining, coughing, tight collar, etc.), decreases (in the early stages of development) with a vertical position of the body, after taking drinks containing caffeine. The diagnosis of a crisis requiring emergency care is established from the moment the occipital pain irradiates into the retro-orbital spaces, after which the intensity of the pain quickly increases, it becomes diffuse and painful. In the late phase of the crisis, various autonomic disorders appear, most often nausea, then repeated bouts of vomiting, which briefly alleviate the patient’s well-being. Injection of blood vessels in the sclera and conjunctiva, sometimes cyanotic facial hyperemia, are detected; “General cerebral” neurological disorders are determined (lethargy, dissociation of reflexes in the upper and lower extremities, nystagmoid movements of the eyeballs, etc.). A crisis often begins with a moderate increase in blood pressure, for example to 170/100 mm Hg. Hg ; it increases as the crisis develops to 220/120 mm Hg. Art. or more, but sometimes even in the late phase does not exceed 200/100 mm Hg. Art. (leading significance of regional angiodystonia).
Cerebral ischemic crisis is caused by an excessive tonic reaction of the cerebral arteries in response to an extreme increase in blood pressure (sometimes systolic pressure is higher than the maximum of the tonometer scale). Distinctive clinical symptoms are focal neurological disorders dependent on the zone of cerebral ischemia; they appear in the late phase of the crisis. They are often preceded (sometimes several hours before) by signs of diffuse ischemia of the cerebral cortex, expressed by euphoria, irritability, which are replaced by depression, tearfulness; sometimes aggressive behavior appears. In this phase of the crisis, the patient’s uncritical attitude towards his condition is often noted, which makes early diagnosis difficult. A crisis differs from a dynamic cerebrovascular accident only in the lesser severity and relative short duration of focal neurological disorders (less than a day).
A complex cerebral crisis is characterized by the appearance of focal neurological disorders at the height of the clinical manifestations of an angiohypotonic crisis, less often in the initial phase of its development. In the latter case, the leading factor in the pathogenesis of the crisis is the pathological opening of arteriovenous anastomoses in the brain, which contributes to overstretching of the veins and leads to focal ischemia due to the phenomenon of “stealing” capillaries.
A generalized vascular crisis, in addition to an extreme increase in blood pressure with severe diastolic hypertension, is characterized by polyregional angiodystonia with signs of impaired blood supply to several organs simultaneously: the brain (headache, neurological disorders), the retina of the eyes (visual disorders with loss of visual fields), the heart (angina pectoris, arrhythmias), the kidneys (protheinuria, hematuria). Acute left ventricular failure often develops.
Treatment: a mentally gentle environment for the patient, emergency administration of seduxen (or droperidl) and fast-acting antihypertensive drugs, selected depending on the severity of the crisis, blood pressure level and pharmacological history; the use of vasoactive and symptomatic agents in accordance with the clinical and pathogenetic variant of the crisis. The initial type of hemodynamics (hyper- or hypokinetic) in most cases is not decisive for the choice of antihypertensive drug, but in a cardiac crisis, peripheral vasodilators that do not reduce cardiac output are preferred.
Approximate tactics of emergency drug therapy for the main types of hypertensive crises are presented in Table. 6. In case of complex cerebral crisis, Devincan or a combination of no-spa with aminophylline is preferred among vasoactive drugs; symptomatic therapy coincides with that for cerebral hagiohypotonic crisis. In case of generalized vascular crisis, antihypertensive therapy begins with intravenous administration of clonidine with furosemide; if the effect is insufficient, ganglion blockers are administered (intravenous drip with control blood pressure measurements at least every 2 minutes).
Classification of hypertension according to blood pressure level
The presented classification is the most relevant and practical. Because the main thing for understanding hypertension is pressure indicators and their changes.
Table
| View | Pressure indicators |
| Optimal | 12 0 at 80 mm Hg. Art. And |
| Normal | 12 0-1 30 at 80-85 mmHg. Art. |
| Closer to normal | 1 30- 1 40 at 85-90 mmHg. Art. |
| I degree of headache | 1 40-1 59 at 90-99 mmHg. Art. |
| II degree of headache | 1 60-1 79 per 1 00-1 09 mm Hg. Art. |
| III degree of headache | 1 80 to 11 0 and above |
The last III degree of hypertension entails the development of a hypertensive crisis, which has disastrous consequences.
Basic concepts and pathogenesis
Arterial hypertension (AH) is characterized by a persistent increase in blood pressure, which has an upper (systolic) and lower (diastolic) limit.
The unit of measurement for blood pressure on the walls of blood vessels is millimeters of mercury. Blood pressure may rise several times a day and be temporary or persistent. A mild form of the disease, when systolic pressure is within the range of 140-159 mmHg. Art., and diastolic 90-99 mm Hg. Art. Blood pressure increases abruptly and normalizes without the use of medications.
Jumps in systolic pressure reach 160-179 mmHg. Art., and the diastolic reaches 100-109 mmHg. This is a moderate form of the disease, in which the indicators are maintained for a long time and cannot return to normal on their own. Second degree hypertension requires drug treatment.
A severe form of the disease, in which diastolic readings exceed 180 mmHg. Art., and systolic reaches 110 mm Hg. Art. This degree of pathology requires systematic monitoring of blood pressure and a serious therapeutic approach.
Highlighted by some experts. This is a very severe form, indicating a sharp increase in blood pressure and deterioration of the patient's condition. In medical practice it is called a “hypertensive crisis.” If the patient was saved, he will still require long-term rehabilitation.
There is also isolated systolic hypertension (ISH), a form of the disease in which systolic pressure exceeds 140 mmHg. Art., and the diastolic remains normal.
Classification of the degrees of hypertension is necessary for correct diagnosis of the disease and selection of effective treatment.
This is the most severe complication of hypertension, in which the power of the heart decreases, so blood passes through the chambers more slowly. As a result, the organ is not sufficiently saturated with nutrients and oxygen. Hypertensive disease with primary damage to the heart has several stages of development:
- At the first stage, hypertrophy of the left ventricle occurs due to increased load on the heart muscle.
- The second stage is characterized by the development of diastolic dysfunction (impaired ability of the myocardium to completely relax in order to fill with blood).
- At the third stage, systolic dysfunction of the left ventricle occurs (violation of its contractility).
- The fourth stage occurs with a high probability of complications.
Hypertensive heart is a term that refers to the enlargement of the left ventricle due to constantly elevated blood pressure. The reason is a set of anatomical, physiological and biochemical processes that occur in the myocardium during hypertension from the very beginning of the disease (when there are no symptoms) to the last stage (when heart failure develops).
The pathogenesis of the disease can be described as follows:
- High blood pressure causes vasospasm, which makes it difficult for blood to flow through them.
- The heart begins to work harder to push blood through, which leads to hypertrophy (enlargement) of its muscles.
- The vessels that feed the heart do not supply the required volume of substances for the enlarged organ.
- Due to low amounts of nutrients, the heart muscle weakens and wears out.
The heart undergoes the following changes:
- enlargement of the left ventricle of the heart;
- impaired diastolic function;
- development of systolic dysfunction.
Risk factors
If we consider the causes of hypertension, they include the following:
- Age: men over 55 years old, women over 65 years old.
- Violation of the lipid ratio in human blood.
- Diabetes.
- Overweight.
- Bad habits.
- Heredity.
- Nervous overstrain.
- Excessive consumption of salty, fried and fatty foods.
In accordance with the symptoms of hypertension and their effect on organs, four types of risk are distinguished, namely:
- Risk 1. 1-2 manifestation factors were detected, stage 1 hypertension. Other organs are not affected, the possible occurrence of death in the next ten years is minimal - 10%.
- Risk 2. Stage 2 hypertension, manifestation factors remain unchanged. One of the target organs is affected, the possible death rate in the next decade is 15-20%.
- Risk 3. Stage 3 hypertension, 2-3 manifestation factors were detected. Complications appear that worsen the course of the disease. The probability of death is 25-30%.
- Risk 4. Stage 3 hypertension, but there are more than three factors. All important target organs are affected, the probability of death is high - 35% or more.
Hypertension and pregnancy
Hypertension during pregnancy is the most common cause of premature birth of a child or perinatal fetal death. Typically, a woman already has hypertension before pregnancy and then simply becomes more active, because carrying a child is a kind of stress for the body.
Considering the high risk for the mother and the unborn child, if the disease is diagnosed, it is important to determine exactly the degree of this risk in order to decide on further bearing the fetus or terminating the pregnancy. Doctors distinguish three degrees of risk (based on the stage of arterial hypertension):
- Risk level 1 – pregnancy complications are minimal, crises rarely develop. Possible angina. Pregnancy in this case is acceptable;
- Level 2 risk – pronounced. Complications develop in 20–50% of cases. A pregnant woman experiences hypertensive crises, insufficiency of the coronary vessels of the heart, and high blood pressure. Termination of pregnancy is indicated;
- 3 degree of risk. Pregnancy complications occur in 50% of cases. Perinatal mortality is observed in 20% of cases. Possible placental abruption, uremia, and impaired blood circulation in the brain. Pregnancy poses a danger to the mother's life, so it is terminated.
The effect of hypertension on various organs
Patients who continue to be pregnant must visit a doctor once a week so that he can monitor their condition. Treatment of hypertension is mandatory. The following antihypertensive drugs are allowed:
- antispasmodics;
- saluretics;
- sympatholytics;
- clonidine derivatives;
- rauwolfia preparations;
- ganglion blockers;
- beta blockers.
Also, in order to treat illness during pregnancy, doctors resort to physiotherapy.
The role of the sympathetic nervous system in the development of hypertension
The sympathetic nervous system has a significant influence on hypertension, namely its state of tension. This complex of symptoms is called sympathicotonia, when the tone of the sympathetic nervous system exceeds the tone of the parasympathetic nervous system. Manifests itself due to excessive consumption of sodium, alcohol, smoking, etc.
Sympathicotonia increases heart rate, vascular tone and total peripheral vascular resistance. Increases the load on blood vessels and increases blood pressure.
Diagnostics
To make an accurate diagnosis, you will have to undergo more than one diagnostic procedure. It is almost impossible to detect pathology with a routine visual examination. Most often prescribed:
- Electrocardiogram of the heart;
- Echocardiogram;
- Electroencephalography of the brain.
As an additional diagnosis, consultations with highly specialized specialists (endocrinologist, neurologist and others), biochemical blood tests, and ultrasound of the kidneys can be prescribed.
Note. To help make an accurate diagnosis, regular blood pressure monitoring is helpful. In this case, all data after measurements are recorded in a notebook, which is provided to the doctor at the next appointment. This will help to track the dynamics of changes in pressure indicators and make more correct prescriptions.
What can be the complications of hypertension?
The primary threat of hypertension is a complication in the functioning of the heart and blood vessels. According to WHO, decapitated hypertension is hypertension combined with damage to the heart and left ventricle. This type of hypertension has irreversible consequences and difficult treatment.
If pressure drops are not treated, pathology may occur in the functioning of any organ. May develop:
- Angina pectoris.
- Myocardial infarction.
- Brain infarction.
- Acute cerebral circulatory disorder with vascular rupture.
- Swelling of the lungs.
- Retinal detachment.
Which human organs are affected by hypertension?
Hypertensive disease primarily affecting the heart
- Temporary loss of consciousness and dizziness occur due to heart rhythm disturbances, as a result of which blood flow to the brain decreases and transient neuronal ischemia occurs
- People say that a hypertensive person is always “ruddy”; the symptom appears due to reflex dilatation of the vessels of the face in response to a narrowing of the blood vessels of the heart.
- High pulse and heart rate.
- Feeling as if “your heart is jumping out of your chest.”
- Patients are often disturbed by inexplicable fear and worry about something.
- The cardiac variant of hypertension is often accompanied by sudden changes in fever and chills.
- Heartbeat.
- Sensations of pulsation in the head.
- Nervousness.
- Swelling of the face and ankles is a consequence of heart failure.
- Visual hallucinations (floaters, stars, etc.).
In addition, tingling of the fingertips and numbness of the limbs may occur.
At the stage of an objective examination of the patient, the doctor performs palpation, percussion and auscultation of the projection area of the heart. With palpation examination, the doctor can determine a pathological cardiac impulse, or pathological changes in the physiological cardiac impulse.
Normally, the cardiac impulse is located in the fifth intercostal space on the right, it is limited and persistent. The “hypertensive” cardiac impulse, in turn, can shift to the left side, diffuse and weak.
During percussion, the doctor will pay attention to the expansion of the absolute and relative boundaries of the heart, which will indicate hypertrophy, and with auscultation, various kinds of pathological sounds can be detected.
To make a diagnosis of hypertension with myocardial damage, the following types of laboratory and instrumental diagnostics are used:
- Electrocardiographic examination of the heart. With the help of which, the doctor can assess the contractile function of the myocardium, the correctness of the rhythm, and conductivity. The presence of ventricular hypertrophy can be diagnosed by the axis deviation on the ECG tape.
- Electrocardiographic study with stress. This diagnostic method is advantageous for establishing the presence of coronary heart disease or angina.
- Ultrasound of the heart or echocardiographic examination of the myocardium and its cavities. Using this method, the doctor can examine “congestive” myocardium, enlarged cavities and the condition of the valves.
- MRI and CT.
- Ultrasound of the cervical choroid plexuses and trunks of the carotid arteries to assess the intima/media complex. This indicator should not exceed 1 mm.
- Biochemistry of blood.
- Holter electrocardiogram monitoring
Additionally, Doppler examination of the vessels of the heart and neck can be used.
Having learned what a hypertensive heart is and about all its dangerous consequences, the patient is obliged to immediately begin treatment for his condition.
It is worth noting that in the case when the patient’s myocardium is damaged, this is already the third stage of arterial hypertension. A competent cardiologist can treat such a patient. The condition for achieving the goal of treatment is the patient’s absolute commitment to it.
First of all, the following are assigned:
- tablets to lower blood pressure (diuretics, beta blockers, calcium inhibitors, ACE inhibitors, etc.);
- cardioprotective agents;
- painkillers;
- nitrates for a more effective reduction in blood pressure in case of concomitant ischemic heart disease and reducing the myocardial need for O2;
- vitamin therapy;
- Exercise therapy, massage. Prescribed if the patient has no signs of cardiac decompensation.
Moreover, the criterion for recovery or remission is a radical change in lifestyle, that is, giving up bad habits, exercising, rest, calm and relaxation.
Heart attacks and strokes are the cause of almost 70% of all deaths in the world. Seven out of ten people die due to blockages in the arteries of the heart or brain.
What’s especially scary is the fact that a lot of people don’t even suspect that they have hypertension. And they miss the opportunity to fix something, simply dooming themselves to death.
- Headache
- Increased heart rate
- Black dots before the eyes (floaters)
- Apathy, irritability, drowsiness
- Blurred vision
- Sweating
- Chronic fatigue
- Swelling of the face
- Numbness and chills in fingers
- Pressure surges
Even one of these symptoms should give you pause. And if there are two of them, then have no doubt - you have hypertension.
How to treat hypertension when there are a large number of medications that cost a lot of money?
Most medications will do no good, and some may even be harmful! At the moment, the only medicine that is officially recommended by the Ministry of Health for the treatment of hypertension is Giperium.
Before
The Institute of Cardiology, together with the Ministry of Health, is conducting a “
no hypertension
” program.
Within the framework of which the drug Giperium is available free of charge
to all residents of the city and region!
Survey plan
- First of all, you need to measure your blood pressure at rest. The measurement must be carried out at least twice with a break of a couple of minutes on each hand. One hour before the start of the procedure, you should not expose yourself to physical activity, drink alcohol, coffee, smoke, or take antihypertensive medications. If this is a primary measurement, it is better to repeat an additional one during the day to achieve an accurate result. Patients under 20 years of age and over 50 years of age should additionally measure the pressure in each leg.
- It is necessary to take a general blood test, which is carried out in the morning on an empty stomach. If hypertension is long-lasting, the level of red blood cells and hemoglobin may increase.
- It is necessary to take a general urine test in the morning.
- Analysis of daily urine, which is collected every three hours in a separate jar.
- It is necessary to conduct a biochemical blood test.
- An ECG is performed to determine damage to the left ventricle.
- Echocardiography is performed to determine the presence of a hypertensive heart.
- The fundus of the eye is examined for changes in it.
- Phonocardiography is performed to determine the heart tone. If hypertrophy develops, the size of the first tone oscillations decreases. Heart failure is characterized by the third and fourth sounds.
- Rheoencephalography is performed to determine vascular tone.
How to properly and effectively treat yourself
You can treat hypertension at home, but it is advisable to discuss all your actions with your doctor so that the treatment is beneficial and not harmful.
There are many effective and safe methods of lowering blood pressure that traditional medicine offers. How to treat arterial hypertension without drugs?
Baths. The use of hot foot baths effectively and quickly reduces blood pressure, especially when adding mustard powder to the water.
Pomegranate. The fruit itself is very useful for hypertension. But you can also treat yourself with pomegranate peels. They are brewed instead of tea and drunk in unlimited quantities.
Currant. It is useful in any form, especially fresh. You can make compote, drink juice, make jam, it is very tasty and healthy to eat fresh berries pureed with sugar. It will remove the unpleasant symptoms associated with high blood pressure.
Healthy vegetables. Arterial hypertension can be treated by eating various vegetables. Beets are useful in any form. Its juice copes well with atherosclerosis and lowers blood pressure. Potatoes baked in their jackets contain a lot of potassium, which is good for the heart and blood vessels. Onions and garlic fight blood pressure and strengthen blood vessels; you should eat them every day.
Healing elixir. Ingredients: onion (1 pc.), garlic (4 cloves), dried rowan (tablespoon). Grind all this, add cold water (1 liter) and cook after boiling for 15 minutes over low heat. After this, add a pinch of herbs: dried herbs, dill, parsley. Mix all this well and cook for another 15 minutes.
After cooking, cool and strain. Next, we get rid of high blood pressure by taking one and a half spoons up to 4 times a day. You should drink the product before meals, half an hour before. The entire course will take about ten days. After taking a break of 21 days, undergo the course of treatment again.
Rosehip with honey. Brew a tablespoon of dry rosehip (fruit) in boiling water (500 g), then heat over low heat for 10 minutes. Then cool and pass through cheesecloth. You can drink the recommended remedy in any quantity, adding honey (1 tbsp.) to the drink.
Mineral water drink. Add honey (1 tbsp), lemon (juice from half a fruit) to mineral water (200 g), stir everything. To cope with hypertension, you need to drink the medicine before meals in the morning, one glass for a week.
Differential diagnosis
Establishing a differential diagnosis is required to exclude a disease that, based on certain symptoms and manifestations, is not suitable, in order to ultimately diagnose one suitable disease.
There are many diseases that have common manifestations with hypertension, but also differ:
- Chronic pyelonephritis is an inflammatory process with damage to the renal tubules. In half of the cases, this disease is accompanied by hypertension, which can be malignant. The formulation of the diagnosis takes into account: whether there have previously been kidney stones, cystitis, pyelitis, developmental pathologies; signs that are not characteristic of hypertension, pain in the lumbar region, etc.
. The appearance of urinary syndrome before hypertension, previous nephritis, nephropathy.
Chronic glomerular nephritis- Renovascular hypertension is secondary hypertension, expressed in impaired blood supply to the kidneys due to narrowing of the renal arteries.
- Coarctation of the aorta is a pathology that manifests itself in the narrowing of the aorta, which results in an imbalance of blood circulation in the body. It is characterized by weakness in the lower extremities, muscle cramps, etc.
- Isolated systolic hypertension is an increase in upper (systolic) pressure with normal lower pressure. Hypertension is characterized by an increase in lower pressure.
- Pheochromocytoma is a hormonally active tumor that actively produces catecholamines.
- Conn's syndrome is an increased production of aldosterone in the adrenal glands. Inherent in hypertension in combination with increased urine production; disorders in the urinary system; feeling of thirst, muscle weakness, etc.
Character of the course
The concept of hypertension is not limited to the strength of its blood pressure. There are classifications based on the progression of the disease:
- Benign hypertension - characterized by a slow course, correlates with the first three degrees, when pathological processes in the body are not very pronounced.
- Malignant hypertension is a rapidly progressing stage that begins to develop in childhood. It has a severe course with signs of encephalopathy, epilepsy, and coma.