- What it is?
- Classification
- Causes and risk factors
- Stages and symptoms
- Diagnostics
- Treatment of sinus arrhythmia of the heart
- Features in children
If the heart rhythm is disturbed and the rhythm of heart contractions is disrupted with the correct sequence of contractions of the heart chambers, the condition is called sinus arrhythmia. The disorder itself does not cause complications, but in combination with other diseases it can cause heart failure, so this diagnosis should not be neglected.
What happens with sinus arrhythmia?
work of the conduction system of the heart; the sinus node “starts” the cardiac cycle
Speaking about normal heart rhythm, it is necessary to keep in mind that it is characterized by a frequency of 60 to 90 heart beats per minute, and the coverage of the myocardium by electrical excitation is characterized by consistent, uniform conduction of waves through the heart muscle - starting from the sinus node in the right atrium appendage and to the apex hearts. Thus, the sinus node is a pacemaker, or pacemaker, of the 1st order. It is in this anatomical formation, measuring up to 1.5 cm, that electricity is self-generated throughout a person’s life, promoting regular heart contractions.
With the pathological influence of various factors on the sinus node, as well as with conduction disturbances (a block in the path of the impulse in the area of the sinus node or vice versa, repeated circulation of the impulse according to the type of re-entry mechanism), a violation of the sequential propagation of excitation throughout the myocardium (heart muscle) occurs. Of course, the latter mechanism often leads to more dangerous arrhythmias, but they can also be combined with sinus arrhythmia.
So, with sinus arrhythmia, impulses come from the pacemaker not with a certain periodicity, but after different periods of time. In the first minute of counting the pulse, for example, a person experiences rapid rhytachycardia [/anchor] - more than 90 per minute), in the second minute - bradycardia (decrease in rhythm less than 55 per minute), and in the third - normal heart rate.
Prevalence of sinus arrhythmia
To assess the incidence of sinus arrhythmia among the population, two concepts should be distinguished - sinus respiratory arrhythmia and sinus arrhythmia not associated with respiratory phases. The first form is a variant of the norm and occurs as a result of a reflex interaction between the respiratory and circulatory organs. This type of sinus arrhythmia occurs quite often, especially in childhood, adolescence and young adulthood.
respiratory sinus arrhythmia
Sinus arrhythmia, not associated with breathing, almost always occurs due to pathology of the cardiovascular system and is quite rare, mainly in older people.
Forecast
Only a cardiologist can predict the outcome of the disease after receiving research results and identifying the root cause of the development of sinus arrhythmia.
If the cause of heart rhythm disturbances is increased physical and mental stress, then to stabilize the condition it is necessary to adjust the daily routine. Redistributing loads in favor of proper rest will allow you to get rid of pathological symptoms without the use of medications.
But if the provoking factor is heart disease, then it is difficult to talk about a favorable outcome. The patient will be advised to take medication for life. In severe cases of sinus arrhythmia, it may be necessary to install a pacemaker, since the disease can cause death.
Causes of the disease
All diseases and conditions that can cause sinus arrhythmia can be divided into several groups:
Diseases of the heart and blood vessels
- Heart defects (congenital and acquired), leading to changes in the normal anatomical structure of the heart, as a result of which cardiomyopathy (hypertrophic, restrictive and dilated) gradually develops. These changes prevent the normal conduction of excitation through the heart, resulting in various arrhythmias, including sinus.
- Most often, sinus arrhythmia develops as a result of coronary heart disease (CHD), mainly after myocardial infarction - acute (especially localized along the lower wall of the left ventricle) or transferred to post-infarction cardiosclerosis (PICS).
- Consequences of myocarditis - as a result of inflammatory and cicatricial changes, cardiac conduction function is also impaired.
Diseases of other organs
- Lesions of the thyroid gland, in particular, thyrotoxicosis caused by autoimmune thyroiditis (Hashimoto's goiter), as well as nodular goiter.
- Diseases of the adrenal glands (pheochromocytoma), as a result of which the level of the hormones adrenaline and norepinephrine increases, causing various arrhythmias, including sinus.
Pathological conditions
- Anemia, especially severe (hemoglobin content in the blood less than 70 g/l),
- Fever,
- Staying in conditions of high (tendency to tachyarrhythmia) or low (tendency to bradyarrhythmia) ambient temperature,
- Acute infectious diseases,
- Acute poisoning with chemicals, drugs, alcohol, medications, etc.
Vegetative-vascular dystonia
As a result of an imbalance between the sympathetic and parasympathetic parts of the central nervous system, one type of regulation of cardiac activity predominates in humans. For example, parasympathetic (vagus nerve, or vagus) slows down the heart rate, and sympathetic nerve fibers lead to increased heart rate. When the regulation of the heart is disturbed, the sinus node generates electrical impulses irregularly - arrhythmia occurs.
How do episodes of sinus arrhythmia manifest?
Symptoms of sinus arrhythmia may vary from patient to patient and depend not only on the severity of the arrhythmia, but also on the patient’s own perceptions.
Some people do not feel the arrhythmia at all, and then the rhythm disturbance is detected during a routine electrocardiogram.
Another part of the patients experience minor interruptions in the functioning of the heart, such as stopping or fading of the heartbeat, followed by a feeling of accelerated heartbeat. These attacks can also be accompanied by autonomic disorders - profuse sweating, paleness or vice versa, redness of the skin of the face, hands and feet, bluish coloration of the nasolabial triangle, a feeling of shortness of breath, increased anxiety and fear of death (like a panic attack), pain in the chest, trembling of limbs.
In adults with severe sinus arrhythmia, presyncope may occur. Fainting is also a common occurrence. This is due to the fact that during periods of low heartbeat (40-50 per minute), the blood supply to the brain suffers, and hypoxia (acute lack of oxygen) occurs in its cells.
Possible complications
If arrhythmia is not treated promptly, serious complications are possible, which can subsequently lead to death. These include the following:
- Formation of blood clots in blood vessels.
- Impaired blood circulation in the brain.
- Heart failure.
- Malfunction of the respiratory system.
- Brain stroke.
- Pulmonary edema.
- Sudden cardiac arrest.
Each of these pathologies requires special therapy.
Timely seeking medical help will help avoid such complications.
Diagnosis of sinus arrhythmia
The doctor can suspect the diagnosis during a conversation with the patient and his examination, based on complaints, when counting the pulse and listening to the heart area. As a rule, with moderate sinus arrhythmia, the beats per minute rarely reaches high values, as, for example, with atrial fibrillation and supraventricular tachycardia, when the heart rate is above 120. With sinus arrhythmia, the heart rate can be within the normal range (55-90 per minute), and also less (45-50 per minute) or more than normal (90-110 per minute).
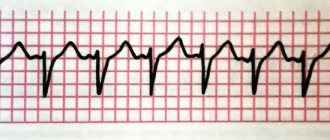
The main confirmation of sinus arrhythmia is an electrocardiogram and 24-hour (Holter) ECG and blood pressure monitoring.
The diagnostic criteria are a registered irregular sinus rhythm, not associated with respiratory phases, and periods of increased, decreased or normal heart rate, replacing each other.
After identifying and confirming sinus arrhythmia not associated with breathing, the doctor faces the next task - to determine whether this arrhythmia is a transient (transient) condition caused by fever, poisoning, or other acute conditions, or whether the cause of the arrhythmia is a more serious heart pathology. To do this, the doctor prescribes laboratory and instrumental methods of further examination - general blood and urine tests, biochemical blood tests, echocardioscopy.
If necessary, for example, in patients with coronary artery disease, coronary angiography (CAG) may be indicated to visualize the coronary arteries of the heart and assess their damage to atherosclerotic plaques, and for patients with heart defects, chest x-ray to identify venous stasis caused by heart failure.
How to treat sinus arrhythmia?
Therapy for this pathology consists of several components.
Firstly, every patient with sinus arrhythmia caused by heart pathology requires lifestyle correction.
For example, people with congestive heart failure need to monitor the amount of fluid consumed (no more than 1.5 liters per day) and the amount of table salt in food (no more than 3-5 grams per day). This is required in order not to overload the heart with excess fluid, since it is more difficult for it to pump blood through the vessels. If heart failure is compensated, then arrhythmia will manifest itself less, thereby increasing the patient’s quality of life.
Persons who have coronary artery disease as a cause of rhythm disturbances are strongly recommended to reconsider their diet - exclude fatty and fried foods, first of all limiting the consumption of animal fats and products containing them (cheese, egg yolks) since these are rich in cholesterol, deposited in the coronary arteries. arteries in the form of plaques.
In addition to diet, all patients with episodes of sinus arrhythmia are recommended to spend more time in the fresh air, perform feasible physical activity, for example, walking, swimming, if there are no contraindications, etc. You should also follow a work and rest regime with at least a night's sleep. 8 hours, and also eliminate stressful situations.
Secondly, patients are prescribed medication.
Thus, in case of anemia, correction of the hemoglobin level with iron-containing drugs (sorbifer durules, totema) is required, up to and including blood transfusion when the hemoglobin level is critical.
For diseases of the thyroid gland, the endocrinologist prescribes thyreostatic drugs (tyrosol, etc.) to suppress the hyperproduction of thyroid hormones into the blood.
In case of fever, acute infectious diseases, or poisoning, detoxification therapy is carried out using droppers and copious fluid intake as prescribed by a doctor.
If cardiac pathology is detected, it is recommended to prescribe medications such as:
- Beta-blockers, if the patient has a rapid heartbeat (for example, Coronal 5 mg in the morning, Egilok 12.5 mg twice a day, etc.),
- ACE inhibitors or ARA 11 blockers for heart failure, after myocardial infarction (lisinopril 5 mg/day, Prestarium 5 mg/day, Lorista 50 mg/day, Valz 40-80 mg/day, etc.),
- Diuretics for heart failure caused by heart defects, post-infarction cardiosclerosis or consequences of myocarditis - veroshpiron 25-50 mg/day, furosemide (Lasix) 20-40 mg/day, indapamide 1.5 - 2.5 mg/day, etc.
In addition to these groups of drugs, after examination the patient may be prescribed other medications.
Thirdly, surgical treatment may be indicated as a treatment for the causative disease leading to sinus arrhythmia..
For example, removal of thyroid nodules helps normalize hormonal status, which affects heart contractions.
Cardiac surgical treatment, in turn, comes down to the installation of stents or coronary artery bypass grafting for persons with coronary artery disease and acute myocardial infarction.
In addition, persons with severe bradyarrhythmia, fraught with frequent fainting and cardiac arrest, are advised to install an artificial pacemaker; and for persons with severe tachyarrhythmia, which can lead to more serious, life-threatening types of tachycardia, installation of a cardioverter-defibrillator may be indicated. Both devices are types of pacemaker (pacemaker).
In any case, individual treatment regimens are prescribed to each patient only based on the results of an in-person examination by a doctor.
Preventive measures
Prevention of sinus arrhythmia allows you to avoid its relapses and speed up the recovery process. It is enough for the patient to follow these rules:
- exclude fatty, fried and smoked foods from the menu;
- saturate your diet with vegetables, fruits and berries;
- choose low-fat meat, fish and dairy products;
- limit salt intake to 5 g per day;
- give up strong tea, energy drinks and coffee;
- sleep at least 7-8 hours a day;
- avoid stressful situations;
- to refuse from bad habits;
- monitor your weight;
- increase resistance to stress (yoga, hardening);
- monitor blood pressure and pulse levels;
- follow all recommendations of a specialist;
- be fully examined once a year;
- rest more, take breaks at work;
- undergo sanatorium-resort treatment annually;
- play sports (running, swimming).
Sinus arrhythmia has many varieties, but rarely provokes serious disruptions in hemodynamics. An exception is an abnormal heartbeat due to organic damage. This problem gradually develops and can lead to dangerous complications. To avoid this, it is recommended to undergo a full examination to identify the causative factor. Based on the results obtained, the doctor will recommend effective treatment methods.
Features of the course of sinus arrhythmia in children
In healthy newborn infants, young and school-aged children, sinus arrhythmia is common, but in most cases it is closely related to breathing. That is, if a child has respiratory sinus arrhythmia, then most likely he is healthy. However, the child needs to consult a cardiologist.
Sinus arrhythmia, not associated with breathing, can also occur in a healthy child due to the immaturity of his autonomic nervous system.
However, most often sinus arrhythmia in newborns is caused by prematurity, birth and hypoxic lesions of the central nervous system, as well as congenital organic damage to the myocardium.
In older children and adolescents, sinus arrhythmia can be caused by the consequences of rheumatic heart disease and heart defects.
Clinically, sinus respiratory arrhythmia in most children does not manifest itself with any symptoms and can be detected during a routine ECG. Sinus “non-respiratory” arrhythmia usually does not manifest itself either, however, some older children who are already able to formulate their complaints experience:
- Feeling of interruptions in the heart,
- Tingling pain in the heart area,
- Increased fatigue.
In infants, parents may notice signs of sinus arrhythmia, for example:
- Increased fatigue and shortness of breath during physical activity and even during breastfeeding,
- Bluish coloration of the nasolabial triangle,
- General pallor
- Weakness,
- Feeling short of air.
Treatment for respiratory sinus arrhythmia is usually not required. But it is better for parents to learn about this from a cardiologist or pediatrician who will examine the baby in person.
Treatment of sinus arrhythmia, especially caused by heart pathology, should be carried out only under the supervision of a cardiologist. Even if sinus arrhythmia detected in a newborn or an older child is not associated with heart pathology (for example, according to the results of ultrasound of the heart), but is due to other reasons, the baby should still be observed by a cardiologist in a children's clinic for some more time. time (a year or more, depending on whether the arrhythmia persists or not).
The prognosis for sinus arrhythmia is generally favorable, but it is determined by the course of the underlying disease. For example, with heart defects, the prognosis is more favorable the earlier treatment is started. The same can be said about other cardiac and non-cardiological pathologies. In any case, sinus arrhythmia requires close monitoring by a cardiologist, as well as timely treatment and exclusion of more dangerous heart rhythm disturbances.
Treatment
Treatment is determined on an individual basis and must be comprehensive with mandatory monitoring by a doctor. Therapy consists of:
- following a diet - caffeine-containing products, alcohol, fatty, fried, spicy, too spicy foods are prohibited;
- categorical cessation of smoking;
- taking medications from the groups of sedatives, tranquilizers, antiarrhythmic drugs, beta-adrenergic receptor and calcium channel blockers, taking cardiac glycosides;
- in severe cases, they resort to installing a pacemaker.
Among the sedatives used are Valocordin, Corvalol, Validol, ankylosing spondylitis, and preparations with valerian extract. Among the tranquilizers, Diazepam, Phenazepam, Gidazepam, Phenibut, Afobazol, Buspirone are indicated. Antiarrhythmic drugs include Asparkam, Panangin, Adenosine, and preparations with magnesium sulfate. Among beta-blockers, Bisoprolol, Atenolol, Esmolol, Carvedilol, Nebivolol, etc. are widely used. Calcium channel blockers include Verapamil, Gallopamil, Nifedipine, Diltiazem, Clentiazem, Cinnarizine, Bepridil, Amlodipine. Cardiac glycosides are represented by Digoxin, Strophanthin, Korglykon, Adoniside, Celanide, Lantoside, etc.
Drugs should be used with extreme caution in children, especially young children. Since the child has not yet developed the mechanisms of metabolism and detoxification of the body, there is an enzyme deficiency, which is why drugs can accumulate in the body for a long time and have a toxic effect. Dosages in children should be selected individually, depending on age, body weight, and the presence of concomitant pathologies. Only in emergency cases can you resort to prescribing ½ adult dose to a child.
In case of a sudden attack, seek emergency help:
- place the patient on his back with the head end raised and the foot end down;
- move the patient's head to one side;
- provide a flow of fresh air;
- if necessary, unfasten or remove the patient’s clothing;
- call an ambulance or take the patient to the hospital yourself;
- if you have the skills to treat with medications, give medications to the patient;
- in case of respiratory and cardiac arrest, immediately resort to cardiopulmonary resuscitation for 30 minutes. continuously.