One of the forms of manifestation of coronary heart disease (CHD) is angina pectoris. The disease is not a life-threatening disease; rather, it signals a possible danger. As a precursor to the development of serious pathology, angina pectoris indicates heart problems.
According to statistics, the first sign of the development of coronary artery disease is an attack of angina in 50% of patients. Moreover, increased physical activity most often leads to this. The disease is quite specific, so to make a correct diagnosis, the doctor only needs to analyze the symptoms.
general description
Myocardial damage that occurs when blood flow in the coronary arteries is disrupted is called coronary heart disease (CHD). By the way, this is precisely what is associated with the second name of this pathology - coronary heart disease.
IHD is quite common and is one of the main causes of disability and death in patients around the world.
The incidence of coronary heart disease in women is lower than in men. This is due to the presence of certain sex hormones in the female body, which reduce the risk of developing atherosclerosis. With the onset of menopause, the production of these hormones decreases, and the risk of developing coronary artery disease increases.
According to statistics, in developed countries, coronary artery disease and stroke account for more than 90% of all cardiovascular pathologies.
Classification of IHD according to the International Classification of Diseases
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Coronary heart disease is a pathology of the heart muscle associated with a lack of blood supply and increasing hypoxia. The myocardium receives blood from the coronary (coronary) vessels of the heart. In diseases of the coronary vessels, the heart muscle lacks blood and the oxygen it carries. Cardiac ischemia occurs when oxygen demand exceeds oxygen availability. In this case, the heart vessels usually have atherosclerotic changes.
The diagnosis of IHD is common among people over 50 years of age. With increasing age, pathology occurs more often.
Species and subspecies
Ischemic disease is classified according to the degree of clinical manifestations, susceptibility to vasodilating (vasodilating) drugs, and resistance to physical exercise. Forms of IHD:
- Sudden coronary death is associated with disorders of the myocardial conduction system, that is, with sudden severe arrhythmia. In the absence of resuscitation measures or their failure, instantaneous cardiac arrest when confirmed by eyewitnesses, or death after an attack within six hours of its onset, a diagnosis of “primary cardiac arrest with fatal outcome” is made. If the patient is successfully resuscitated, the diagnosis is “sudden death with successful resuscitation.”
- Angina pectoris is a form of coronary artery disease that causes a burning pain in the middle of the chest, or more precisely, behind the sternum. According to ICD-10 (International Classification of Diseases, 10th revision), angina pectoris corresponds to code I20.
It also has several subspecies:
- Angina pectoris, or stable, in which the supply of oxygen to the heart muscle is reduced. In response to hypoxia (oxygen starvation), pain and spasm of the coronary arteries occurs. Stable angina, unlike unstable angina, occurs during physical activity of the same intensity, for example, walking 300 meters at a normal pace, and is relieved with nitroglycerin preparations.
- Unstable angina (ICD code - 20.0) is poorly controlled by nitroglycerin derivatives, attacks of pain become more frequent, and the patient's exercise tolerance decreases. This form is divided into types:
- first appeared;
- progressive;
- early post-infarction or post-operative.
According to the international classification 10 (ICD-10), angiospastic angina (Prinzmetal's angina, variant) corresponds to 20.1 (Angina with confirmed spasm). Angina pectoris - ICD code 20.8. Unspecified angina was assigned code 20.9.
- Myocardial infarction. An attack of angina that lasts more than 30 minutes and is not relieved by nitroglycerin ends in a heart attack. Diagnosis of a heart attack includes ECG analysis, laboratory testing of the level of markers of damage to the heart muscle (fractions of the enzymes creatine phosphokinase and lactate dehydrogenase, tropomyosin, etc.). Based on the extent of the lesion, they are classified as:
- transmural (large focal) infarction;
finely focal.
According to the international classification of the 10th revision, acute infarction corresponds to code I21, its varieties are distinguished: acute extensive infarction of the lower wall, anterior wall and other localizations, unspecified localization. The diagnosis of “recurrent myocardial infarction” was assigned code I22.
Other forms of IHD - codes I24-I25:
- Painless form (according to the old classification of 1979).
- Acute heart failure develops against the background of myocardial infarction or during shock conditions.
- Heart rhythm disturbances. With ischemic damage, the blood supply to the conduction system of the heart is also disrupted.
ICD-10 code I24.0 is assigned to coronary thrombosis without infarction.
ICD code I24.1 - post-infarction Dressler syndrome.
Code I24.8 according to the 10th revision of the ICD - coronary insufficiency.
Code I25 according to ICD-10 - chronic ischemic disease; includes:
- atherosclerotic ischemic heart disease;
- previous heart attack and post-infarction cardiosclerosis;
- cardiac aneurysm;
- coronary arteriovenous fistula;
- asymptomatic ischemia of the heart muscle;
- chronic unspecified ischemic heart disease and other forms of chronic ischemic heart disease lasting more than 4 weeks.
Risk factors
The tendency to ischemia is increased with the following risk factors for ischemic heart disease:
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
- Metabolic, or syndrome X, in which the metabolism of carbohydrates and fats is impaired, cholesterol levels are elevated, and insulin resistance occurs. People with type 2 diabetes are at risk for cardiovascular diseases, including angina and heart attack. If your waist circumference exceeds 80 cm, this is a reason to be more attentive to your health and nutrition. Timely diagnosis and treatment of diabetes mellitus will improve the prognosis of the disease.
- Smoking. Nicotine constricts blood vessels, increases heart rate, and increases the heart muscle's need for blood and oxygen.
- Liver diseases. With liver disease, cholesterol synthesis increases, this leads to increased deposition on the walls of blood vessels with further oxidation and inflammation of the arteries.
- Drinking alcohol.
- Physical inactivity.
- Constantly exceeding the caloric intake of the diet.
- Emotional stress. With anxiety, the body's need for oxygen increases, and the heart muscle is no exception. In addition, during prolonged stress, cortisol and catecholamines are released, which narrow the coronary vessels, and cholesterol production increases.
- Lipid metabolism disorders and atherosclerosis of the coronary arteries. Diagnostics - study of the lipid spectrum of the blood.
- Syndrome of excessive colonization of the small intestine, which disrupts liver function and causes vitamin deficiency of folic acid and vitamin B12. This increases cholesterol and homocysteine levels. The latter disrupts peripheral circulation and increases the load on the heart.
- Itsenko-Cushing syndrome, which occurs with hyperfunction of the adrenal glands or with the use of steroid hormones.
- Hormonal diseases of the thyroid gland, ovaries.
Men over 50 and women during menopause are most likely to suffer from angina and heart attacks.
Risk factors for coronary heart disease that aggravate the course of coronary heart disease: uremia, diabetes mellitus, pulmonary failure. IHD is aggravated by disturbances in the conduction system of the heart (blockade of the sinoatrial node, atrioventricular node, bundle branches).
The modern classification of coronary artery disease allows doctors to correctly assess the patient’s condition and take the right measures to treat it. For each form that has a code in the ICD, its own diagnostic and treatment algorithms have been developed. Only by freely navigating the varieties of this disease can the doctor effectively help the patient.
The doctor will definitely take into account the presence of contraindications. For example, if a patient has a peptic ulcer or erosion of the gastrointestinal tract, then preference will be given to a protected drug, or another antiplatelet agent will be selected. In any case, additional medications may be prescribed to protect the gastric mucosa.
None of the drugs will be used if there is intolerance to the components, aspirin asthma, pregnancy, blood clotting disorders and childhood.
Heart aspirin may help prevent cancer
Analogues of Aspirin cardio
This question interests every patient whose financial capabilities are limited. The following analogues exist on the pharmaceutical market:
- Thrombo ACC;
- Acecardole;
- Cardiomagnyl;
- CardiASK;
- Aspicard;
- Polocard;
- Aspicor;
- ASK;
- Magnecard;
- Upsarin UPSA
In conclusion, it should be especially noted that the choice of drugs for the prevention of thrombosis requires a responsible approach. Considering what has been said in the article, you need to understand that any drug is not only useful, but can also be harmful to our body. Therefore, before starting to take Aspirin medications, it is necessary to consult with your doctor, telling about concomitant non-cardiological pathology and/or side effects from the medication that have occurred previously.
Causes of IHD
The development of coronary heart disease occurs under the influence of the following factors:
- Atherosclerosis. With this disease, the level of cholesterol in the body increases, which leads to the formation of atherosclerotic plaques. These plaques are deposited on the walls of blood vessels, narrowing their lumen and impairing blood circulation, which can lead to the development of coronary artery disease. In the initial stages, ischemia manifests itself in the form of angina pectoris, but as metabolism deteriorates, the blood supply to the myocardium continues to decrease, pain increases, and heart failure develops. If a plaque breaks off and the coronary vessel becomes completely blocked, blood stops flowing to the heart and a heart attack develops, the outcome of which can be fatal.
- Psycho-emotional factors. Some researchers believe that people with high social status are less susceptible to CHD.
- Poor nutrition. Leads to excess cholesterol synthesis and the formation of atherosclerotic plaques.
- Diabetes. Leads to disruption of carbohydrate metabolism, which can provoke the development of coronary artery disease.
- Obesity. Recent studies by scientists have confirmed the existence of a connection between obesity and mortality from coronary artery disease.
- Constant stress, emotional overstrain. Under these conditions, the body synthesizes a substance that promotes the deposition of cholesterol on the walls of blood vessels.
- Physical inactivity or, conversely, increased physical activity. In both cases, an excessive load is created on the myocardium, which can lead to lack of nutrition and the development of ischemia.
- Bad habits. Alcohol abuse and smoking have a negative effect on the condition of the heart and blood vessels.
Patient examinations
The cardiologist reviews the patient's medical history, performs a physical examination, an electrocardiogram, and an echocardiogram. Holter monitoring is used if cardiac arrhythmias are suspected.
The existence of underlying structural heart disease is confirmed in most cases by clinical history. The ECG also shows certain markers of a previous heart attack:
- the presence of Q waves in the corresponding segments;
- jagged or wide QRS complexes
- low QRS voltage;
- combination of ventricular tachycardia morphologies;
- prolonged paroxysms.
Dynamics of ECG changes during myocardial infarction (registration in three standard leads)
Extrasystole of organic nature IHD manifests itself:
- QRS amplitude ≤ 10 mm;
- axis displacement higher or lower;
- QRS width > 12 ms;
- the appearance of teeth;
- symmetry of T waves;
- inversion or reversal of the ST segment.
Extrasystoles in IHD can be rare (less than 30 per hour), frequent (more than 30 per hour), multiple, repeated - group attacks of ventricular tachycardia.
Diagnostic methods include ECG, stress test, 24-hour monitoring, echocardiography and CT with drug tests. After myocardial infarction, electrophysiological studies are required.
Differential diagnosis is carried out with supraventricular tachycardias caused by His bundle block when the impulse is conducted along the accessory pathway.
Symptoms of coronary heart disease
It is known that the clinical manifestations of IHD depend on the form of the disease. In cardiology, the main classification is considered to be IHD, according to which the following types of disease are distinguished: sudden coronary death, angina pectoris, post-infarction cardiosclerosis, various types of arrhythmias, circulatory failure, myocardial infarction, microvascular IHD, new ischemic syndromes.
Sudden coronary death . It is the most severe form of coronary heart disease, as it has a high mortality rate. It is quite difficult for doctors to respond to this form of the disease, since the attack develops suddenly, quickly, and death can occur within the next few hours or even instantly.
The causes of the disease are arrhythmias, complete blockage of the heart arteries. Taking large doses of alcohol can trigger an attack. Many patients do not even realize that they are suffering from coronary artery disease before the attack.
Angina pectoris . This condition is manifested by severe burning pain behind the sternum, on the left. The patient has difficulty breathing, he feels pressure and heaviness, as if a concrete slab was placed on his chest.
The nature of the pain may vary. It can be stabbing, burning, pressing, radiating under the left shoulder blade, into the lower jaw. In addition to pain, the patient feels severe weakness, cold sweats, and a fear of dying. Sometimes, instead of pain, asphyxia occurs (a condition when a person feels a lack of air).
The attack lasts several minutes. Since the pain intensifies with movement, the patient stops during an attack of angina and tries to take a stationary position to reduce the intensity of the pain.
Myocardial infarction . An extremely severe and dangerous form of IHD for humans. Clinically manifested by tearing severe pain behind the sternum, which radiates to the left shoulder blade, lower jaw, and arm.
The pain is not relieved by nitroglycerin and does not go away for a long time. This is a hallmark of a heart attack and allows it to be differentiated from other conditions with a similar clinical picture (for example, angina pectoris).
In addition to pain, the patient feels a lack of air, he experiences severe weakness, cold sweat, nausea, vomiting, blood pressure drops, and a fear of death appears.
The area of the myocardium that is deprived of blood supply loses elasticity and dies. At the same time, the healthy part of the heart, trying to compensate for losses, begins to work at maximum, which can lead to rupture of the dead area during myocardial contractions (popularly this condition is called heart rupture). The point of therapeutic measures is to prevent rupture and ensure that the site of the heart attack heals and the heart can begin to work further.
Heart failure . Symptoms of coronary heart disease in this case are due to the fact that the myocardium cannot provide the body with a sufficient amount of blood.
The disease can develop after the death of part of the myocardium during a heart attack. Clinically, this pathology is manifested by shortness of breath, which in advanced forms can appear even at rest, a feeling of general weakness, swelling of the veins of the neck, enlarged liver, and swelling of the lower extremities. On auscultation, wheezing is heard in the lungs.
Conduction disorders and arrhythmias . This is also one of the forms of IHD, which has many different types.
Symptoms of coronary heart disease in this case are manifested by a feeling of interruptions in the functioning of the heart. The patient feels bubbling in the chest, sometimes it seems to him that the heart has stopped. The causes of arrhythmia can be metabolic and endocrine disorders, taking certain medications, and intoxication of the body. The disease can also occur as a complication of other cardiovascular diseases.
In some cases, the course of IHD is asymptomatic, which significantly complicates diagnosis and can lead to the development of a number of severe complications, including the death of the patient.
Therefore, you need to listen carefully to your body and consult a doctor when the first alarming symptoms appear:
- general weakness;
- chest pain radiating to the neck, arm;
- causeless nausea and vomiting;
- feeling of heaviness, burning, squeezing in the chest;
- shortness of breath, periodic asphyxia;
- feeling of increased anxiety.
Medications
In case of acute and chronic myocardial ischemia, it is necessary to take medications. The choice of certain agents is determined for each patient separately, depending on the diagnostic study.
Doctors generally prescribe antiplatelet agents, in particular, such as Cardiomagnyl, Aspirin Cardio, and Thrombo Ass. They normalize the blood circulation process and also reduce the load on the myocardium.
Beta blockers such as Nebivolol, Carvedilol and Bisoprolol will help reduce the number of heart contractions and myocardial oxygen demand. Statins and fibrates lower cholesterol levels and prevent the progression of atherosclerosis. Such drugs include Lovastatin and Fenofibrate.
ACE inhibitors such as Captopril and Enap normalize blood pressure and also eliminate arterial spasms. Diuretics are required to eliminate excess fluid, which creates additional stress on the heart. Such drugs include Lasix and Indapamide.
Antiarrhythmic drugs are required to detect cardiac arrhythmias. Very often doctors prescribe Amiadron and Cordarone. Organic nitrates, in particular, such as Isoket and Nitroglycerin, are used when pain in the heart occurs. For ischemia and myocardial infarction, the doctor may additionally prescribe other medications.
Diagnosis of coronary heart disease
Modern medicine has a large range of different diagnostic techniques for detecting myocardial ischemia. The simplest and most accessible methods for diagnosing IHD are:
- collecting anamnesis, interviewing the patient;
- external examination - signs of IHD are cyanosis of the skin and mucous membranes, swelling of the extremities;
- Auscultation is listening to heart sounds using a phonendoscope;
- functional tests with physical activity (for example, bicycle ergometry) - allow you to identify heart failure and other types of ischemia.
These simple examination methods for coronary artery disease allow you to diagnose the disease, find out its nature and draw up a plan for further action. If the cardiologist wants to clarify the diagnosis and more accurately determine the form and severity of the disease, the patient may be prescribed additional examinations.
Most often, the diagnosis of IHD is made based on the results of the following studies:
- An ECG is one of the most informative methods for diagnosing coronary artery disease; based on changes in the waves on the cardiogram, a cardiologist can make a diagnosis with a high degree of confidence; in addition to a standard ECG, a stress ECG can be performed (for example, to diagnose heart failure);
- ECHO KG - detects lesions in individual areas of the heart muscle;
- coronary angiography - with the help of this study, the localization and degree of damage to the heart arteries is determined, the degree of their narrowing by cholesterol plaque is diagnosed, and differential diagnosis of coronary artery disease is carried out from similar pathologies;
- blood test (biochemical) - determine the presence of an inflammatory reaction in the body, disorders of fat metabolism;
- radioisotope diagnostic methods - determine the obstruction of the patency of the heart vessels.
Diagnosis of the disease
Patient complaints are very important to make a correct diagnosis. The doctor will need information about:
- the location of pain and irradiation of pain to other parts of the body;
- frequency of angina attacks, their duration and strength.
- whether physical activity provokes attacks;
- how the patient manages to relieve pain.
Laboratory tests include a blood test to check for the development of atherosclerosis, as the main possible cause of vascular damage. To make a correct diagnosis, instrumental examinations are also carried out:
- Electrocardiogram as the main way to obtain information about cardiac disorders;
- Daily Holter monitoring to track the dynamics of changes during each attack of angina;
- An echocardiogram, which allows you to see the changes that have occurred during the development of coronary artery disease;
- Velgoergometry, which allows you to determine the maximum physical activity that a patient can endure without the threat of developing coronary artery disease.
- Diagnostic coronography, which allows you to assess the condition of the heart arteries.
Treatment of coronary heart disease
The approach to therapy for coronary artery disease depends on the type of ischemia, the severity and severity of the disease, the age and individual characteristics of the patient. Depending on these factors, treatment of coronary heart disease can be either conservative or surgical.
If the pathology is diagnosed at an early stage, does not manifest itself clinically and is not accompanied by a significant disturbance in the blood supply, then non-drug measures may be sufficient.
The patient must change his lifestyle, normalize his work and rest schedule, start eating right, and give up smoking and alcohol abuse.
Long walks in the fresh air and adherence to a special diet that prevents the deposition of fat in the body and the formation of atherosclerotic plaques on the walls of blood vessels, which is the most common cause of the development of coronary artery disease, will be useful.
It is necessary to give up fatty, fried, spicy, salty, smoked, pickled foods, and introduce more fresh fruits and vegetables into the diet, rich in fiber, as well as vitamins and microelements beneficial to the body. In addition, you should reduce the amount of liquid you drink per day to reduce the likelihood of edema.
If the patient has no complaints of chest pain, only occasionally he experiences slight discomfort in the heart area, then in order to prevent further progression of the pathological process, sanatorium treatment can be prescribed.
If the disease is already quite advanced, then the above measures will not be enough, since the pathological changes in the cardiovascular system are already quite large. In this case, the cardiologist prescribes drug treatment for coronary heart disease using special medications.
The treatment regimen is compiled individually for each patient, taking into account his current condition, age, and the presence of concomitant diseases. The following groups of drugs can be prescribed for the treatment of ischemic heart disease:
- β-blockers - reduce heart rate, reduce the need for oxygen in the heart muscle;
- nitrates (Nitroglycerin) - reduce the load on the heart, affect the contraction of vascular smooth muscles, relieve pain;
- antiplatelet agents - thin the blood, preventing blood cells from sticking to each other and preventing them from depositing on the walls of blood vessels;
- diuretics - help relieve swelling;
- drugs that reduce the concentration of cholesterol in the body (fibrates, statins) - taking these drugs reduces the risk of the formation of atherosclerotic plaques, which are one of the main causes of the development of coronary artery disease;
- anticoagulants;
- ACE inhibitors - reduce blood pressure and a number of others.
If emergency conditions develop, as well as if conservative treatment of ischemia does not help and the disease continues to progress, significantly reducing the patient’s quality of life and posing a threat to his health and life, surgical treatment is indicated.
Surgical treatment of coronary artery disease, depending on the indications, may include:
- stenting;
- coronary bypass surgery;
- balloon angioplasty.
Clinical picture
Manifestations of IHD with arrhythmias are variable. If ischemia is complicated by rhythm disturbances, the patient experiences:
- rapid heartbeat in addition to chest pain if the arrhythmia is stable;
- syncope and sudden cardiac death due to hemodynamically unstable ventricular fibrillation.
With arrhythmias associated with healed scars, complications are asymptomatic. The clinical picture is complemented by rapid heartbeat, shortness of breath, and chest discomfort. Clinical tolerance to tachycardias is related to speed, the presence of retrograde conduction, baseline ventricular function, and the integrity of peripheral compensatory mechanisms. Continuous tachycardia, even against the background of stable hemodynamics, leads to heart failure.
IHD prognosis
The outcome of the disease depends on many different factors (the general health of the patient, his age, the presence of chronic diseases, the degree of neglect of ischemia, the timeliness of treatment, and a number of others).
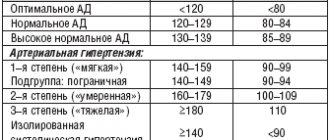
The prognosis becomes unfavorable if complications of coronary artery disease such as arterial hypertension, diabetes mellitus, and severe lipid metabolism disorders develop. In this case, therapy can only slow down the progression of the disease. It will no longer be possible to completely cure IHD.
Angiotensin receptor antagonists
These are new generation drugs that normalize blood pressure and have almost no side effects.
Most popular groups:
- angiotensin receptor antagonists;
- sartans;
- angiotensin receptor blockers.
Hypertension negatively affects myocardial vessels. Untreated hypertension increases the risk of progression of ischemia, stroke, and chronic heart failure.
Angiotensin receptor inhibitors lower blood pressure and prevent cardiac enlargement or hypertrophy. They must be taken over a long period of time under the supervision of a physician.
To improve the patient's condition, the following is prescribed:
- Perindopril;
- Lisinopril;
- Ramipril;
- Enalapril.
Anti-ischemic drugs alleviate the course of the disease and improve the quality of life of patients.
Prevention of coronary artery disease
The main measures to prevent coronary heart disease are:
- regular sanitation of foci of chronic infection in the body;
- rejection of bad habits;
- weight control, preventing the development of obesity;
- timely treatment of pathological conditions of the body that can lead to the development of coronary artery disease;
- balanced, proper nutrition - foods that are good for the heart and blood vessels are seafood, lean meats, fresh fruits and vegetables, low-fat dairy products, legumes, nuts, cereals, meals should be fractional (meals should be taken 5-6 times a day, small in portions);
- giving up a sedentary lifestyle, which leads to the development of congestion in the cardiovascular system - regular walking, swimming, physical exercise to strengthen the heart muscle;
- avoidance of stress and other psycho-emotional disorders;
- refusal to take uncontrolled medications; all medications should be prescribed only by the attending physician; self-medication is unacceptable and can lead to the development of a number of serious complications;
- regular monitoring of blood pressure;
- Regular preventive examinations and ECGs will help identify ischemia at an early stage, which will significantly facilitate subsequent treatment and avoid the development of complications.
Good health to you!
Treatment of ischemia (CHD) with folk remedies
Alternative medicine offers its own options for alleviating the condition of ischemic disease. The most effective recipes contain only natural ingredients and help quickly improve the patient’s well-being.
- Grind the horseradish root with a blender or meat grinder. Add boiling water to the mixture and let it brew for 24 hours. After this, add a little carrot juice into the container and add honey to taste. Drink 1 tbsp. l. per day.
- Steam 20 g of strawberry leaves. Take the decoction in small portions throughout the day.
- Chop the garlic. Pour 50 g of gruel with 100 ml of vodka and leave for 3 days. After this, strain and consume 3-4 drops three times a day.
- Add 1-2 tablespoons of fresh or dried dill to a glass of boiled water. Divide the decoction into 4-5 doses and drink throughout the day.
- Mix two parts of the herb gray jaundice, dill and reed sunflower flowers with one part of coltsfoot. Mix all ingredients thoroughly and brew with boiling water. After the infusion has cooled, it should be strained and consumed a tablespoon twice a day.
All folk remedies provide additional help. They can only be used after prior consent from the doctor. It is very important that the patient simultaneously receives high-quality and timely medical treatment. In the absence of adequate therapy, ischemia in elderly men and women leads to severe disability or death.
First aid
First aid for acute cardiac ischemia includes:
- Call an ambulance.
- Providing rest to the patient.
- Giving the correct position. In case of acute ischemia, you need to place the person on his back, slightly raising his head and shoulders. They should be at an angle of 30-40º.
- Removing restrictive clothing.
- Ensuring a flow of clean air. You need to open a window or window.
- Taking medications. Nitrates are used (Nitroglycerin, Sustak Forte, Nitrocor, Nitrong Forte). The tablets are placed under the tongue and dissolved. In the absence of symptoms of pulmonary edema, you can additionally give the patient an Aspirin or Clopidogrel tablet to chew. These are antiplatelet agents that are effective against thrombosis.
- Normalization and control of blood pressure. If blood pressure is elevated, antihypertensive drugs (beta blockers) can be used. After stabilization of the condition, ACE inhibitors are used.
- Carrying out resuscitation measures. They are required when the heart stops and breathing stops.
- Constant monitoring of breathing rate, pulse and pressure.
Important information: How to treat vascular ischemia of the lower extremities and what are the symptoms of ischemic leg disease
Further treatment may include:
- Strict bed rest.
- Strict diet.
- Defibrillation (restoring the heart rhythm with electric current). Indications for its implementation are ventricular flutter and fibrillation, ventricular tachycardia.
- Oxygen therapy. In severe cases (when a person is unable to breathe on their own), intubation and mechanical ventilation (artificial ventilation) are required.
- Normalization of pressure.
- The use of symptomatic drugs (narcotic analgesics, anticonvulsants, antiarrhythmic drugs). For pain syndrome, the combination of Droperidol with Fentanyl is effective.
- The use of antiplatelet agents, anticoagulants, thrombolytics, calcium antagonists and other agents.
In severe cases, surgical interventions are resorted to:
- Coronary bypass surgery. It involves creating bypass paths for blood movement. This operation is open and is performed after the patient’s condition has normalized. In the acute period, shunting is dangerous.
- Percutaneous coronary intervention.
- Installation of pacemakers or pacemaker.
- Excision of the aneurysm.
- Coronary angioplasty.
- Stenting (artificial dilation of blood vessels using metal structures to improve blood flow).