Pregnancy-associated plasma protein-A (PAPP-A) is one of the largest associated enzymes produced by the embryo and placenta (syncytiocytotrophoblasts).
This protein is thought to have several different functions, including preventing fetal recognition by the maternal immune system, matrix mineralization, and angiogenesis. PAPP-A levels increase depending on the week of pregnancy when tested and analyzed in the 1st trimester, which is considered normal.
What is PAPP-A?
Detection of the protein is possible in the 1st and 2nd trimester when performing a diagnostic test for aneuploidy, including trisomy 21 (Down syndrome).
Maternal serum concentrations are associated with subsequent fetal growth, and this relationship suggests that it may be used as a diagnostic test for adverse pregnancy outcomes (intrauterine growth restriction, preterm labor, preeclampsia, and stillbirth).
Alternative names: pappalisin 1, PAPP-A, PAPPA1, SP4, high molecular weight alpha-2 mobile pregnancy-specific protein, IGFBP4 protease (IGFBP-4ase), ASBABP2, DIPLA1, PAPA.
Biochemical screening
Biochemical screening makes it possible to form a high-risk group for having children with congenital malformations and chromosomal diseases. The method is based on determining serum markers in a woman’s blood. The concentration of these substances changes as the duration of pregnancy increases and when the condition of the fetus is impaired.
Indications for biochemical screening:
- Mother's age is over 35 years;
- Consanguineous marriage;
- The presence of a chromosomal rearrangement, hereditary disease or developmental defect in one of the spouses;
- The birth of a child with a hereditary disease or developmental defect;
- A history of spontaneous miscarriages, stillbirths, primary amenorrhea, primary infertility in spouses;
- Adverse effects of environmental factors in the early stages of pregnancy (radioactive radiation, inhalation of vaporous poisons, etc.);
- Taking embryotoxic drugs in early pregnancy;
- X-ray examination in the early stages.
At what stages of pregnancy is PAP-A testing performed?
For pregnant women, to assess the risk of a chromosomal disorder such as Down syndrome (trisomy 21) or Edwards syndrome (trisomy 18) in the child, a test is provided in the 1st trimester of pregnancy. It is usually carried out between 11-14 weeks. This test or screening in the 2nd trimester helps determine whether a diagnostic test is needed.
PAPP-A during pregnancy (the norm at 12-25 weeks (1st and 2nd trimesters) shows the same data values) is performed 1 time, but sometimes an additional test can be performed in the 3rd trimester to clarify the values.
Many women get tested as early as possible in the 1st trimester to find out if there may be a problem. However, if testing is not possible for unfounded or personal reasons, a woman has the right to undergo it after 18 weeks in the 2nd trimester.
What does the analysis determine?
Studies conducted during biochemical screening are aimed at determining the likelihood of developing chromosomal pathologies in the fetus.
At the end of the first trimester of pregnancy, you can already find out the risk of such diseases as:
- Down syndrome;
- Anencephaly;
- Edwards syndrome;
- Spinal canal cleft.
Down syndrome or trisomy 21 pairs of chromosomes is a fairly common disease in the modern world. Thus, we get not two, but three chromosomes.
Children with this diagnosis have a characteristic appearance. With broad features, slanted eyes and a fairly short nose.
The disease is accompanied by mental retardation, cerebral palsy and other multiple pathologies of the development of internal organs.
Anencephaly or absence of a brain. This pathology can be determined by ultrasound. Such children are not viable.
As in the case of Down syndrome, an extra chromosome appears in the 18th pair.
This disease is accompanied by a large number of concomitant pathologies. Unfortunately, these babies usually do not survive birth.
Spinal bifida, or spina bifida, is a neural tube disorder that affects the spinal cord.
After birth, babies will not be able to fully move and will most likely be paralyzed.
If this pathology has accompanying deviations of internal organs, then the child is not viable.
Advantages and disadvantages of the method
Over the past 10 years, various screening and diagnostic tests have been developed to detect Down syndrome, and the use of combined ultrasound and serum markers has been evaluated.
Some doctors only offer these tests to women of a certain age, and the practice is controversial. ACOG has developed guidelines that evaluate the use of ultrasonography and serum markers for selective screening of aneuploidy in pregnant women.
Research has shown that in the 1st trimester there is an association between the size of the fluid collection at the back of the fetal neck (nuchal translucency) and the risk of trisomy 21.
Extensive assays have revealed that nuchal translucency can be combined with free beta-hCG and pregnancy-associated plasma protein A (PAPP-A) to screen for Down syndrome. PAPP-A and hCG measurements are effective for screening only in the 1st trimester, and alpha-fetoprotein, unconjugated estriol, and inhibin should only be performed in the 2nd trimester.
Pregnancy associated protein (PAPP-A)
RARR-A
(pregnancy-associated plasma protein A) is a macroglobulin, or plasma protein, produced in large quantities by placental fibroblasts during pregnancy.
Detected in the mother's bloodstream. Its concentration increases throughout pregnancy. This protein ensures the full growth and development of the placenta. During the first 8 weeks of pregnancy, the concentration of PAPP-A in the blood serum doubles every 4-9 days.
But due to the very low initial level of this protein in the bloodstream, most researchers reliably assessed its content only 5-6 weeks after conception, i.e. to the moment of the most dramatic increase in hCG concentration. PAPP-A concentrations increase throughout pregnancy. It also has the ability to break down one of the proteins that binds insulin-like growth factor. This causes an increase in the bioavailability of insulin-like growth factor, which is an important factor in fetal development during pregnancy. In addition, it is able to inactivate some enzymes in the blood (trypsin, elastase, plasmin) and modulate the immune response of the maternal body.
With a chromosomal abnormality
with fetal malformations, the concentration of PAPP-A in the blood decreases significantly from the 8th to the 14th week of pregnancy.
The most dramatic decrease is observed with trisomies on the 21st, 18th and 13th chromosomes. In Down syndrome,
the PAPP-A indicator is an order of magnitude lower than in the norm. The level of PAPP-A in the mother's blood serum drops even more sharply if the fetus has a genetic pathology with multiple malformations - Cornelia de Lange syndrome. The combination of measuring PAPP-A levels with determining the concentration of free beta-hCG in the blood and determining TVP using ultrasound at the end of the first trimester of pregnancy can identify up to 90% of women at risk of developing Down syndrome in the older age group (after 35 years). The test is optimally carried out at about 12 weeks of pregnancy (11 - 14 weeks). After 14 weeks of pregnancy, the diagnostic value of PAPP-A as a risk marker for Down syndrome is lost. The probability of false positive results is about 5%. Detection of deviations in the levels of biochemical markers in the mother’s blood is not an unconditional confirmation of fetal pathology, but, in combination with the assessment of other risk factors, is the basis for the use of more complex special methods for diagnosing fetal abnormalities. In non-pregnant women, small amounts of PAPP-A were found using immunochemical methods in granulosa cells and in the fluid of ovarian follicles, as well as in the mucous membranes of the fallopian tubes, cervix and endometrium. Progesterone had a stimulating effect on the secretion of PAPP-A by various cells of the female reproductive system. In men, the main producers of PAPP-A are Leydig cells, so its level in seminal fluid is 10–20 times higher than in blood plasma. An increase in PAPP-A is recorded after damage to atherosclerotic plaques in acute coronary syndrome and unstable angina. This protein is being actively studied as a marker for the prognosis of coronary heart disease, but has not yet received widespread use in cardiac laboratory tests.
No special preparation is required for the study. It is necessary to follow the general requirements for preparation for research.
GENERAL RULES FOR PREPARATION FOR RESEARCH:
1. For most studies, it is recommended to donate blood in the morning, from 8 to 11 o’clock, on an empty stomach (at least 8 hours must pass between the last meal and blood collection, you can drink water as usual), on the eve of the study, a light dinner with a restriction eating fatty foods. For tests for infections and emergency studies, it is acceptable to donate blood 4-6 hours after the last meal.
2. ATTENTION! Special preparation rules for a number of tests: strictly on an empty stomach, after a 12-14 hour fast, you should donate blood for gastrin-17, lipid profile (total cholesterol, HDL cholesterol, LDL cholesterol, VLDL cholesterol, triglycerides, lipoprotein (a), apolipo-protene A1, apolipoprotein B); The glucose tolerance test is performed in the morning on an empty stomach after 12-16 hours of fasting.
3. On the eve of the study (within 24 hours), avoid alcohol, intense physical activity, and taking medications (in consultation with your doctor).
4. 1-2 hours before donating blood, refrain from smoking, do not drink juice, tea, coffee, you can drink still water. Avoid physical stress (running, quickly climbing stairs), emotional excitement. It is recommended to rest and calm down 15 minutes before donating blood.
5. You should not donate blood for laboratory testing immediately after physiotherapeutic procedures, instrumental examination, X-ray and ultrasound examinations, massage and other medical procedures.
6. When monitoring laboratory parameters over time, it is recommended to conduct repeated tests under the same conditions - in the same laboratory, donate blood at the same time of day, etc.
7. Blood for research must be donated before starting to take medications or no earlier than 10–14 days after they are discontinued.
To assess the control of the effectiveness of treatment with any drugs, a study should be conducted 7-14 days after the last dose of the drug. If you are taking medications, be sure to notify your doctor.
When are plasma proteins A detected in a woman’s body?
PAPP-A during pregnancy, the norm at 8-12 weeks of which practically does not differ from the data in the 2nd trimester, can be estimated only approximately (with the exception of fibrinogen, when testing is carried out on condensed samples):
- With a typical reference range of 60–80 g/L, 1 plasma protein makes up about 7% of plasma by weight 2 and 0.5% of total body weight.
- Serum albumin makes up about 55% of plasma protein (typical reference range: 35–55 g/L), about 3.4. It maintains plasma osmotic pressure and is involved in the transport of calcium, lipids and steroid hormones.
- Globulins make up approximately 35% of plasma protein (typical reference range: 20–35 g/L) – 5.6 values. Globulins are involved in a number of processes, including the transport of ions, hormones and lipids, and acute phase reactions.
Globulins are divided into 4 subgroups:
- 2 alpha-1 (mainly alpha-1 antitrypsin);
- alpha 2 (including haptoglobin and ceruloplasmin);
- beta (contains transferrin and some complement components);
- gamma (includes mainly immunoglobulins and C-reactive protein).
Fibrinogen is a soluble protein that makes up about 6.5% of plasma protein. The conversion of fibrinogen to insoluble fibrin is a process that is critical for blood clotting.
The remaining plasma proteins contain hundreds of different protein molecules. Individually they are present in small quantities, but together they constitute approximately 1% of plasma protein and play important roles as regulatory proteins such as enzymes, proenzymes and hormones.
Plasma proteins are heterogeneous in nature and are involved in many complex body functions.
Abnormalities in plasma proteins can be:
- primary (cause of specific pathologies);
- secondary (the result of a wide range of disease processes).
Abnormal proteinuria can also result from various medical conditions.
Reasons why a gynecologist may perform plasma protein measurements include studies of symptoms, allergies, and immunity:
- Investigation of a specific symptom such as peripheral edema, diagnosis of an inflammatory process or autoimmune disorder: for example, testing of antinuclear antibodies in the evaluation of systemic lupus erythematosus.
- Diagnosis of bone marrow disorders, including multiple myeloma: assessment of allergies, testing for immunodeficiency in patients with recurrent infections, assessment of immunity to infections such as hepatitis B or rubella.
Specific antibody tests test for total immunoglobulin A (IgA) and tissue transglutaminase IgA antibodies.
Assessment of pregnancy-associated plasma protein A (PAPP-A) together with human chorionic gonadotropin (hCG) measurement and ultrasound are suggested for analysis in early pregnancy (10–14 weeks) when the fetus may be at risk for chromosomal abnormalities: Down syndrome (trisomy 21) or Edwards syndrome (trisomy 18).
A urine protein test is performed to diagnose urinary infection, primary kidney disease, including nephrotic syndrome, and secondary kidney disease.
Why is screening done?
A pregnant woman is wary of any examination prescribed by a doctor. After all, the main thing now is that nothing threatens the baby. Therefore, when a gynecologist gives a referral for screening at 13 weeks 6 days, the expectant mother often does not know what to expect from all this and is very worried.
In fact, prenatal examination is as safe as possible and is prescribed to absolutely everyone at 11–13 obstetric weeks due to the simple methods of its implementation:
- ultrasonography;
- screening biochemical blood test.
The first prenatal screening is prescribed at 11 - 13 weeks 6 days. It is during this period that this survey is most informative.
It is especially important for a woman with a complicated pregnancy or previous unsuccessful attempts to carry a baby to undergo the study. These risk factors include:
- a woman whose age is 35+;
- the presence of previous pregnancies that ended in spontaneous miscarriages or non-developing pregnancy;
- there is already a child growing up in the family with a chromosomal or genetic pathology;
- during real pregnancy in the early stages up to 13 weeks, a serious infectious disease was suffered;
- the influence of harmful factors associated with a woman’s profession;
- the expectant mother's addiction to alcohol and drugs.
An ultrasound examination is performed first, and then on the same day blood is donated for biochemical screening. Compliance with this sequence together guarantees a reliable research result. The first screening requires the most correct gestational age, down to the day. Only an ultrasound diagnostic doctor can determine the exact period. In addition, only an ultrasound will give a result about whether the pregnancy is singleton or multiple. Without this information, it is generally not advisable to donate blood, since you will not get high-quality results.
Norm PAPP-A by week
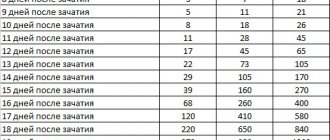
PAPP-A during pregnancy can be performed approximately 32 days after ovulation, when the level of substances increases.
Then every 3 weeks the values double, reaching the norm. Electroimmunoassays can detect circulating hormone levels of 10 μg/L as early as 5 weeks of pregnancy. Serum PAPP-A level was 8.03 ± 2.75 mIU/L (mean ± standard deviation).
A sharp increase in PAPP-A indicates an increased risk of trisomy 21, and a decrease is associated with an increased risk of trisomy 18. Low PAPP-A levels in the first trimester (<0.4 months) are associated with an increased incidence of adverse obstetric outcomes.
Normal PAPP-A during pregnancy
RAPP-A decoding is performed by a specialist who takes into account the ratio of plasma protein A, hCG and ultrasound screening. In addition, it is necessary to take into account the body weight of the expectant mother, smoking, conception through IVF, taking certain medications, diabetes mellitus and the presence of multiple pregnancies.
There are different rates of PAPP-A:
| Week of pregnancy | PAPP-A, mcd/ml |
| From 8 to 9 weeks | 0.17-1.54 |
| 9 to 10 weeks | 0,32 — 2,42 |
| 10 to 11 weeks | 0.46-3.73 |
| From 11 to 12 weeks | 0,79 — 4,76 |
| From 12 to 13 weeks | 1.03-6.01 |
| From 13 to 14 weeks | 1,47 — 8,54 |
What do changes in protein levels indicate?
Deviations both upward and downward from the norm in hCG and PAPP-A levels indicate a risk of developmental abnormalities in the child.
A decrease in the amount of PAPP-A in a woman’s blood, together with an increase in hCG levels, signals a risk of Down syndrome.
Elevated hCG levels can occur in the presence of diabetes, multiple pregnancy, or severe toxicosis.
A low level may also indicate existing problems.
A decrease in the concentration of this protein is observed when:
- ectopic pregnancy;
- development of Edwards syndrome;
- threat of premature termination of pregnancy;
- placental insufficiency.
The reliability of deciphering the results of this test does not exceed 70%. Therefore, in addition to a blood test, it is necessary to undergo an ultrasound examination. It will help determine the diagnosis more accurately.
There are variants of false negative results. In this case, most likely, the diseases will be detected at the 2nd perinatal screening at 18-20 weeks.
Why is it not enough to do only an ultrasound during pregnancy?
Screening for aneuploidy can identify the risk of developing Down syndrome and trisomy 13 or 18. If the screening test is positive and the patient decides to proceed with a diagnostic procedure (eg, CVS, amniocentesis), there is a higher chance of finding an aneuploid fetus than if the woman had not been screened .
Diagnostic testing can detect all autosomal sex chromosome trisomies, large deletions, chromosome duplications, and mosaicism.
The best time to take nuchal translucency measurements is between 12 and 13 weeks of pregnancy. Combined screening is effective for testing for Down syndrome.
For women under 35 years of age, combined screening in the 1st trimester reveals a rate of symptoms similar to that of quadruple screening in the 2nd trimester. For women 35 years of age and older, combined screening will show up to 90% of pathologies.
One of the benefits of 1st trimester screening is the early availability of information. In addition, if a woman is at increased risk of fetal aneuploidy, genetic counseling and CVD, as well as 2nd trimester amniocentesis, may be offered.
Those who choose only one screening in the 1st trimester, or who have good CVS results, should undergo neural tube defect screening (eg, ultrasound, serum alpha-fetoprotein test) in the 2nd trimester.
Women additionally need to undergo fetal echocardiography if the fetal nuchal translucency is at least 3.5 mm. It is unknown whether ultrasound in the 2nd trimester will help if the readings in the 1st trimester are negative.
There are other diagnostic methods:
- Integrated Screening – This is when 1st and 1st trimester markers are used to adjust the patient's age-related risk and are reported after testing. The analysis can be performed using serum markers.
- Potential markers of Down syndrome include nonvisualized nasal bone, tricuspid regurgitation, lumbar length, femur and shoulder length, head and trunk volume, and umbilical cord diameter.
The decision to undergo screening or invasive testing should not be based solely on age, but should take into account patient preference.
Test procedure for plasma protein levels A
PAPP-A during pregnancy (the norm at 12-24 weeks is practically the same in terms of values) may indicate the presence of pathologies. If, after receiving the screening results, a woman is at risk of having a child with Down syndrome, she will be asked to take a test for plasma protein A:
- A needle is inserted through the abdominal wall into the amniotic sac.
- 20-40 cm3 of amniotic fluid is collected.
- During diagnosis, ultrasound is used to select the appropriate puncture site.
After it, the woman must abstain from intimate relations for 3 days.
Preparation
It is recommended not to empty your bladder before testing. The pregnant woman's abdomen is disinfected so that the tissue remains sterile during the examination.
Carrying out
If 1st trimester screening results are concerning, diagnostic tests such as amniocentesis or chorionic villus sampling (CVS) may be recommended. Blood must be taken from a vein in the arm or finger. The ultrasound may be performed from outside the abdomen (transabdominal), or a probe may be inserted into the vagina (transvaginal).
A blood sample is taken between 9 and 13 weeks and 6 days of pregnancy, but preferably between 9 and 12 weeks. This test is used to check the levels of 2 hormones in the blood that change during pregnancy (free B-hCG and PAPP-A).
Ultrasound allows you to measure the thickness of the fluid in the collar area. A computer program then combines the results of these tests with the baby's weight and correct gestational age to determine the risk of having a baby with the condition.
Decoding the results
“Not increased risk” means that the risk of having a baby with Down syndrome is very low.
The rates are less than 1% per 300, or 0.33%. “At increased risk” the risk of having a child with Down syndrome is greater than 1% in 300 (<1 and >2).
Calculation of MoM RAPP-A
There is a calculation formula: the value of the indicator in the woman’s blood serum / the median value.
Eg:
- Median = 2, serum value = 1.
- MoM will be equal to 0.5.
- If the MoM value is closer to 1, the indicator is closer to the mean of the population data.
Next, the values are adjusted due to the weight and age of the mother, the weight of the fetus, race, IVF and the presence of diseases. At stage 3 the risks can be calculated. MoM indicators take into account different types of pathologies, and for a more accurate assessment they need to be combined with the levels of hCG, inhibin A, and free estriol.
How to test for -hCG and PAPP
To get the most reliable results of a biochemical blood screening, you need to properly prepare for it.
The preparatory activities are extremely simple. The day before, you should refrain from eating fatty, smoked or too salty foods. Try to minimize the use of spices.
The analysis is given on an empty stomach. Therefore, it would be wise to take food with you so that you can have a snack immediately after donating blood.
Blood for analysis is taken from a vein.
The referral for this study is given by an obstetrician-gynecologist. The results are also reported by the local doctor.
It is very important not to miss the required deadline for carrying out this analysis. Otherwise, you may get unreliable results.
Reasons for deviations from the norm. Possible pathologies
The result of the RAPP-A analysis cannot be considered separately from the hCG analysis and ultrasound results. Suspected abnormalities in the fetal chromosome region should be diagnosed only by combining data after conducting combinations of studies if PAPP-A is reduced and hCG is elevated.
With this outcome, an additional ultrasound is performed to determine the thickness of the collar space. It must be more than 3 mm to confirm the presence of pathology.
Increased performance
If the RAPP-A indicator is higher than normal, this does not mean that the woman is at risk of abnormal fetal development. Perhaps the gestational age is set incorrectly, and it is advisable to re-screen after some time.
In this case, it is necessary to take into account the cellular outer layer of the fetus, which can synthesize a larger amount of plasma protein. RAPP-A analysis cannot guarantee a 100% result without additional studies. It allows you to identify the risk of developing chromosomal disorders, but does not provide an accurate assessment.
Reduced performance
If RAPP-A is lower than normal, this may mean that the unborn child is at risk for the following diseases:
- Edwards disease is a disorder of chromosome 18, which combines many abnormalities of constitutional and mental development.
- Down's disease is an anomaly of the 21st pair of chromosomes, characterized by signs of delayed mental and physical development.
- Amsterdam dwarfism syndrome (Cornelia de Lange) is a gene mutation disease that manifests itself in delayed psychomotor development to varying degrees.
- Other chromosomal abnormalities (Rubinstein-Taybi disease, mental underdevelopment with hypertrichosis).
For a pregnant woman, a decrease in PAPP-A may mean the risk of miscarriage.
PAPP-A during pregnancy (the norm at 12 weeks is 0.7-4.6) decreases if the child does not gain weight. In the 2nd half of the 2nd trimester, pathology can be accurately diagnosed.
Otherwise, the woman is forced to monitor the development of the fetus weekly. If there are no concerns about the baby's growth, scans will be carried out at 3-week intervals between 28 weeks before birth.
Causes of increased and decreased PPP during pregnancy
Decoding the analysis involves determining the level of ppp a, taking into account that with each week of gestation the parameters increase significantly.
The study is the main tool for diagnosing Down syndrome in percentage terms. During the examination, the combination of all three markers (ultrasound, Papp-A and hCG) is taken into account; the effectiveness in such a situation will be no more than 80%. In addition, for analysis, an anamnesis is collected and an interview with a geneticist is conducted. The doctor must find out about the facts of smoking, the method of conceiving a fetus, information is needed about taking potent medications and the presence of concomitant diseases.
If the indicator is lowered, this indicates chromosomal abnormalities, the development of Down syndrome, Cornelia de Lange or Edwards. Also, a low prr a becomes a reason to assume a threat of miscarriage or to assume the possibility of a frozen pregnancy.
The decoding of indicators above the norm is compared with the numbers from the hCG analysis, since protein A itself can increase when the soft tissues of the body are damaged. If the indicator is elevated, then this often indicates an incorrect calculation of the gestational age, a violation of the research technique, and also the human factor of influence and the associated error cannot be excluded. Therefore, high assessment parameters should not be a cause for concern.
If significant deviations in the upward direction have been identified, then doctors may recommend planned interruption of intrauterine development at an early stage of gestation, since at the present stage of development of medicine there is no way to correct intrauterine chromosomal abnormalities.
At-risk groups
Women aged 35 years and older are generally considered to be at greatest risk of having a child with Down syndrome. Screening methods for these include chorionic villus sampling (CVS) or genetic counseling and amniocentesis.
Women younger than 35 years of age may be screened using human chorionic gonadotropin (hCG) and unconjugated estriol in combination with maternal serum alpha-fetoprotein levels.
When all 3 of these markers are used (triple screening), the detection rate for Down syndrome is about 70%. About 5% of all pregnancies screen positive.
Adding inhibin A to triple screening (4x screening) can increase the detection rate of Down syndrome to approximately 80%. Screening using biochemical markers, ultrasound, or both is increasingly being offered to more accurately assess risk.
Why is human chorionic gonadotropin determined in parallel?
Human chorionic gonadotropin (hCG) is a hormone produced by the placenta in large quantities during pregnancy. In the 1st trimester, you can use either free beta subunit or total hCG.
Levels of both indicators typically rise rapidly in a pregnant woman's blood during the first 8 to 10 weeks, then decline and stabilize at lower levels throughout the remainder of pregnancy.
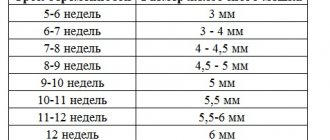
Nuchal (collar) translucency - measurement made by ultrasound. An ultrasound scanner measures fluid collection between the spine and the skin in the fetal neck.
How to confirm or refute the results of the study?
If a risk of developing pathologies has been identified based on the results of screening tests, it is necessary to further confirm or refute the potential diagnosis.
To do this you need:
- Perform amniocentesis or CVS to refute or confirm the analysis data.
- Analyze data from combinations of serum tests performed up to 14 weeks and in the 2nd trimester up to 24 weeks.
- Combine analysis of tests with ultrasound and screening data to predict the development of pathologies.
- Study the ultrasound indicator (neck fold thickness) and 7 different serological indicators - PAPP-A, hCG, free beta-hCG, unbound estriol, alpha-fetoprotein, inhibin A, ADAM
- Separately study and compare the 7 markers listed above with each other and with the results of other studies.
- As a result of the analysis, 32 screening tests with different data can be obtained. 22 studies may have positive results, which indicates a high risk of pathology. But it is too early to confirm such a diagnosis.
Next, you need to take into account the data from checks in the 2nd trimester. They should be more sensitive in the presence of pathologies and give 9/10 values. According to statistics, in 5% of women with an increased risk of having a child with Down syndrome, no pathologies were found after the birth of the baby.
PAPP-A during pregnancy cannot clearly indicate pathologies and diseases. In the early stages of pregnancy, the normal value changes periodically depending on the weight of the fetus and mother. It is important that in the 1st and last weeks of pregnancy the indicator increases evenly and corresponds to the norm in the presence of other research results.
The essence of the analysis
Analysis of pappa during pregnancy is nothing more than pregnancy-associated protein apppa, the volume and concentration of which normally increases in accordance with the gestational age.
The test is mainly carried out in the period from the 8th to the 14th week of gestation, the scope is due to the fact that in other periods the information content is significantly reduced. In this case, the study involves determining hCG, the indicators of which are most optimal at 11-13 weeks, so the time frame is significantly narrowed. There are a number of conditional indications when it is recommended to undergo this study:
- category of women over 35 years of age;
- the birth of older children with genetic disorders;
- miscarriage during a previous conception;
- presence of infectious diseases;
- any genetic abnormalities in close relatives;
- work activities associated with the risk of exposure.
Blood is drawn only in the morning and on an empty stomach, and the examination itself is carried out within up to 2 days. In this case, on the eve of the analysis, it is necessary to limit the consumption of sweets and eliminate physical activity.