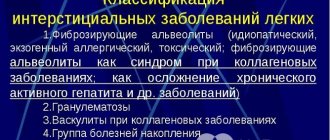
Hydrothorax of the lungs: causes of occurrence, mechanisms of development
The pleural cavities are the gap between the pleural layers - one of them lines the inside of the chest (parietal pleura), the other covers the lungs (visceral pleura). Normally, the pleural cavities are not completely dry - a certain amount of secretions is formed so that during respiratory movements there is no friction between the pleural layers of the chest and lung. But this amount of pleural secretion is so small (in addition, the reverse suction system works) that physiological hydrothorax is not distinguished as a separate concept.
The most common reasons why fluid may accumulate in the pleural cavities:
- heart failure at the stage when compensatory mechanisms no longer work, and congestion occurs in the systemic circulation;
various kidney diseases - primarily those in which the renal glomeruli are affected and nephrotic syndrome develops - massive edema, the presence of protein in the urine (proteinuria) and a decrease in the level of protein in the blood (hypoproteinemia). Most often, hydrothorax is observed with renal pathologies such as glomerulonephritis, and with renal amyloidosis (accumulation of amyloid, a substance that is not normally observed in the body);- cirrhosis of the liver - with it, congestion in the circulatory system is also observed;
- myxedema – a decrease in the production of thyroid hormones (extreme degree of hypothyroidism), due to which fluid accumulates in almost all tissues, as a result of which massive edema develops;
- large tumors that are localized in the mediastinum (a closed space bounded by the sternum, spine and both lungs) - they put pressure on large veins (primarily the vena cava and brachiocephalic veins), thereby causing congestion in them and provoking fluid effusion into nearby structures (including pleural cavities);
- sometimes – nutritional (associated with poor or insufficient nutrition) dystrophy. In this case, effusion into the pleural cavity is closely related to a lack of vitamins B and , as well as a deterioration in lymph outflow.
All the inconveniences and problems that hydrothorax provokes are mechanical in nature: accumulating in the pleural cavities, the fluid begins to put pressure on the lung tissue, and then on the mediastinal organs.
Due to gravity, due to which the fluid rushes to the lower point of the pleural cavities, the fluid pressure initially spreads to the lower parts of the lungs, which are less involved in the act of breathing (therefore, clinical symptoms are either not observed or they are not expressed). With a further increase in the amount of fluid in the pleural cavities, which are closed spaces, the parenchyma of the remaining parts of the lungs is gradually compressed, and then the mediastinum - until it is displaced to the healthy side (if the hydrothorax is unilateral).
The essence of pathology
You may be interested in: Glucosamine sulfate: instructions for use, analogues and reviews
When considering hydrothorax of the lung, one cannot help but pay attention to studying the very essence of this condition. In the human chest there are three special serous sacs, which are intended for each lung separately and for the heart. The pulmonary membrane consists of two layers at once and is called the pleura. The two separate layers are the visceral and parietal pleura. The small slit-like gap between them is called the pleural cavity. In a healthy person, this gap is extremely small and contains 1-2 ml of pleural fluid.
Under certain factors, the amount of fluid in the pleural cavity increases sharply and can reach 1-2 liters. This condition is called hydrothorax of the lung. However, the penetration of other liquids is also possible, and therefore the names change: with the accumulation of blood - hemothorax, lymph - chylothorax, air - pneumothorax.
A characteristic feature of this process is the absence of an inflammatory nature.
Signs of hydrothorax of the lungs
Hydrothorax in most cases develops gradually - several days, rarely several weeks. As the amount of fluid increases, the following clinical picture appears:
there is a feeling of heaviness in the chest. The feeling of discomfort in the chest decreases when lying on the painful side. If the amount of fluid increases even more, the patient tries to be in a semi-sitting position (the fluid rushes into the lower parts of the pleural cavity and does not put pressure on the lung parenchyma or puts much less pressure);- there is a subjective feeling that less air is entering the lungs;
- the patient begins to breathe more often and deeper - this does not always relieve him of the feeling of lack of air;
- cyanosis (blueness) of the skin and visible mucous membranes appears at later stages, so in the initial stages of hydrothorax, examination of the patient will not be informative. Cyanosis is explained by deterioration of pulmonary ventilation and an increase in the amount of carbon dioxide in the blood;
- due to the fact that this is a non-inflammatory process, body temperature is not increased - in some cases, even a decrease may be observed.
If a lot of fluid has accumulated, it interferes with the mobility of the chest, causes the affected half to lag in the act of breathing and leads to the fact that the intercostal spaces become smoothed, and then protrude - this can be seen when examining the patient.
Hydrothorax is often accompanied by:
- hydropericardium (presence of fluid in the pericardial cavity);
- ascites (accumulation of free fluid in the abdominal cavity).
In these cases, in addition to symptoms from the respiratory system, the following symptoms will appear:
- from the heart - pressing chest pain, fatigue, increasing shortness of breath, cardiac dysfunction (determined by ECG);
- from the abdominal cavity - a feeling of fullness in the abdomen, pressing and aching not too intense pain, heartburn, increasing nausea, often resulting in vomiting, protrusion of tissue in the navel area, bloating and changes in the shape of the abdomen (in the patient’s supine position it is spread out, in the sitting position – sags downwards), a pronounced venous network on the skin of the anterior abdominal wall.
There have been cases where hydrothorax, although it developed first, was less pronounced than the accompanying hydropericardium and ascites, and only a medical analysis made it possible to determine the presence of fluid in the pleural cavity.
X-ray for hydrothorax
Subtotal right-sided hydrothorax (diagram).
The mediastinum is shifted to the left. Using an x-ray, it is impossible to determine the nature of the fluid in the pleural cavity (inflammatory exudate, pus, blood, transudate in heart failure, etc.), since different contents cause the same x-ray picture.
darkening with hydrothorax usually does not occupy the entire pulmonary field, but its lower and middle sections, as well as the area of the costophrenic sinus.
A small upper part of the pulmonary field remains “free” (subtotal hydrothorax). When there is a large amount of content, the pulmonary field becomes darkened completely (total hydrothorax), and sometimes a “pleural window” is identified - an area of clearing in the inner zone of the upper parts of the pulmonary field.
With hydrothorax, the X-ray has an intense, uniform darkening; against its background, the elements of the pulmonary pattern and the root of the lung are usually not determined (or poorly distinguishable), it overlaps the shadow of the heart and merges with it (if it is located on the left side). The dome of the diaphragm on the side of the hydrothorax is poorly differentiated (or becomes completely indistinguishable).
The upper border of the darkening is arcuate, “curved” downwards, it is directed from the outer part of the pulmonary field downwards and towards the middle shadow; this border may not be entirely clear. The transparency of the lung in the area immediately above this border is usually reduced due to compression of the lung by contents in the pleural cavity or due to pathological changes in the lung itself, for example, with pneumonia. If the amount of fluid is large, then the pulmonary field is shadowed throughout (total hydrothorax) and the upper limit of the contents in the pleural cavity is not determined.
Subtotal left-sided hydrothorax (a) x-ray in the frontal projection, (b) x-ray in the left lateral projection. The left pulmonary field is shadowed in the middle and lower sections, the upper border of the darkening is arcuate. The mediastinum is shifted to the right (which can be determined by the displacement of the cardiac shadow to the right). The upper border of the left-sided hydrothorax is somewhat unclear, the transparency of the overlying parts of the lung is reduced.
An important sign of pleural effusion on x-ray with hydrothorax is the displacement of the mediastinal shadow in the direction opposite to the pathology. It is easier to identify such a displacement by focusing on the displacement of the trachea; the corresponding displacement of the cardiac shadow is also determined (in this case, the position of the subject must be symmetrical - it is necessary to evaluate the position of the sternal ends of the clavicles, they are at approximately the same distance from the spinous processes of the thoracic vertebrae). With hydrothorax, the displacement of the mediastinal shadow on the x-ray is not always expressed due to the fact that the lung on the affected side is “pressed” (compressed) by the contents in the pleural cavity (the so-called compression atelectasis of the lung is formed). Also, hydrothorax can be combined with atelectasis of the lung on the affected side as a result of bronchial obstruction (for example, by a tumor).
You should always carefully evaluate changes in the opposite lung; they can help in identifying the cause of the effusion (inflammatory infiltrates, manifestations of venous stagnation in the pulmonary circulation, tuberculous changes, space-occupying formations). The condition of the ribs should also be assessed - “fresh” fractures on the affected side can be combined with accumulation of blood in the pleural cavity (hemothorax), destruction of the ribs can be caused by metastatic tumor lesions.
Source: NewVrach.ru
Possible complications
The main immediate complication of hydrothorax is acute respiratory failure. It occurs due to compression of the lung tissue by fluid that accumulates more and more in the pleural cavity, which is too much for the pleural layers to absorb.
With untreated hydrothorax, severe respiratory failure often develops during the first week from the moment when fluid begins to accumulate in the pleural cavities. With increased fluid production (due to severe diseases leading to hydrothorax, or congenital characteristics of the pleural layers), respiratory failure may develop in the first days after the onset of hydrothorax.
If an infection occurs, hydrothorax can be complicated by pleural empyema - a diffuse purulent lesion of the pleural layers.
Features of the appearance of fluid in the pleural cavity
The accumulation of fluid (transudate) in the pleural cavity occurs if the pressure inside the pleural capillaries increases to such an extent that it exceeds the colloid-osmotic plasma pressure. Such conditions cause large amounts of plasma to leak out through the walls of the capillaries. It accumulates in the pleural cavity. The ICD code for hydrothorax of the lung is J94.
An increase in the volume of fluid occurs due to a decrease in the volume of the lung, as a result of which the volume involved in breathing is reduced, and displacement of the internal organs develops.
Diagnostics
Complaints and changes in the patient’s appearance are not specific to pneumothorax; they can also be observed with other types of respiratory pathology. Therefore, to identify fluid in the pleural cavities, a physical examination of the patient is necessary (palpating the chest, tapping with fingers and listening with a phonendoscope), as well as additional instrumental diagnostic methods.
Due to the accumulation of fluid, bulging tissue in the intercostal spaces is felt. When tapping on the chest, the sound becomes dull (normally, when tapping objects with cavities, it is characteristic, as if tapping on a box or drum). When listening, the doctor will hear weakening of breathing, as the fluid puts pressure on the lungs and does not allow them to expand normally. In more severe cases (with advanced hydrothorax or an atypical rapid increase in the amount of fluid), the lung may not breathe at all due to the fact that it does not expand at the site of fluid accumulation.
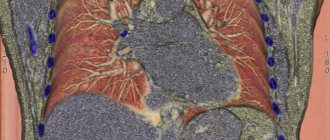
To confirm the diagnosis of hydrothorax, instrumental methods of examining the chest organs are used, such as:
- fluoroscopy and graphy;
- ultrasonography;
- CT scan;
- magnetic resonance imaging.
X-rays are performed in a vertical and horizontal position - the diagnosis of hydrothorax is confirmed by the fact that a uniform darkening in the image caused by fluid is located in the lowest parts of the pleural cavities, and when the position of the body changes, it shifts to the lowest point.
Computed tomography is a more accurate method that, in addition to identifying free fluid in the pleural cavities, will help identify the reasons why it formed:
- mediastinal tumors;
- enlarged lymph nodes that put pressure on the veins, impairing drainage and promoting fluid accumulation
and so on.
Ultrasound examination is used for targeted examination of pleural cavities. It not only detects effusion in the pleural cavities, but thanks to it it is possible to more accurately determine the volume of fluid.
MRI of the chest organs allows you to accurately detect changes in the chest when there is confusion in diagnosis.
Classic laboratory methods for hydrothorax are not decisive - they play a supporting role in clarifying the causes of hydrothorax:
- indicators of a general blood test may worsen in case of kidney diseases that provoke hydrothorax, and tumors of the mediastinum - such diseases are confirmed by an increase in the erythrocyte sedimentation rate (ESR, or ROE) and manifestations of anemia (decreased number of red blood cells and hemoglobin);
- changes in the general urine test with hydrothorax are observed if it is caused by kidney diseases that significantly impair their function. This is manifested by the release of a large amount of protein in the urine, the detection of red blood cells, leukocytes and specific formations - cylinders - in the urine, as well as an increase in the relative density of urine;
- a detailed (biochemical) blood test worsens with pneumothorax caused by cirrhosis of the liver, kidney disease or nutritional dystrophy. The main changes that can be detected are a decrease in the amount of protein in the blood, an increase in the level of nitrogenous waste, an increase in the amount of bilirubin and alanine aminotransferase.
Of greater importance for hydrothorax are:
- puncture of the pleural cavity and examination of the resulting fluid;
- Rivolta test, which helps determine whether fluid has formed in the pleural cavity due to inflammation or not;
- cytological examination (examination under a microscope, carried out to identify cells that are not normally found in the pleural cavity and on the pleural layers);
- bacteriological examination for the presence of microorganisms.
If hydrothorax is suspected, puncture of the pleural cavity is performed not only to confirm the presence of effusion in the cavity, but also for laboratory examination of the fluid in order to clarify the diagnosis . It is necessary to find out whether this fluid is a transudate, which is non-inflammatory in nature, or an exudate formed during inflammatory processes. This has implications for further treatment tactics. Transudate extracted from the pleural cavity with classic hydrothorax has the following characteristics:
- it is a clear liquid;
- light yellow in color (in some cases slightly light greenish);
- has an alkaline reaction;
- without flakes, sediment and impurities. Sometimes the transudate has a bloody admixture, but this should not frighten the patient, who is undergoing a puncture under local anesthesia, which means he observes the process - the presence of blood is explained by injury to small vessels when the puncture needle punctures the chest wall.
Rivolta's test is a determination of the presence of protein in punctate (liquid obtained during puncture), which is carried out using ordinary acetic acid. When it is added, the liquid formed during classic hydrothorax does not become cloudy. If it is an inflammatory exudate, then when the liquid and acetic acid are mixed, cloudiness forms in the form of a cloud.
Cytological examination of effusion formed in the pleural cavity is necessary to distinguish hydrothorax from exudative pleurisy caused by a tumor. During the tumor process, atypical cells are found.
Bacteriological study of pleural effusion is primarily necessary to exclude damage to the pleura due to tuberculosis. The liquid is sown on a nutrient medium and observed to see if there is any characteristic growth of colonies.
Treatment of pulmonary hydrothorax
Methods used to treat hydrothorax:
- conservative (non-invasive - that is, without penetration into the pleural cavity);
- invasive - this is a pleural puncture.
The treatment of hydrothorax is based on conservative methods aimed at curing the diseases that provoked it. It is necessary to understand that it is necessary not only to rid the patient of hydrothorax, but also to cure the cause of its occurrence . If, with liver cirrhosis, glomerulonephritis or other diseases that provoke hydrothorax, fluid is removed from the patient using regular pleural punctures, thereby draining the pleural cavity, but doing nothing to cure the provoking diseases, effusion will still be produced, the effect of pleural puncture will be short-lived. Often, with well-chosen conservative therapy and a small amount of fluid in the pleural cavity, it disappears on its own due to reverse absorption - a pleural puncture may not be necessary.
In case of heart failure that provokes hydrothorax, the following tactics are followed:
- the patient must optimize his regime of work, physical activity and rest, avoid psycho-emotional factors leading to stress, and normalize sleep;
- he should adhere to diet No. 10 or 10a - it involves limiting the intake of liquids and table salt, as well as split meals (it is necessary to eat small portions up to 5-6 times a day);
- drug treatment is prescribed.
The basis of drug treatment for heart failure, which has led to the occurrence of hydrothorax, is unloading the circulatory system , due to which the blood does not stagnate and effusion in the pleural cavity does not form. The following medications are used:
drugs that enhance weakened contractility of the heart muscle (cardiac glycosides and β-adrenergic receptor stimulants);- means that reduce the load on the left ventricular muscle (these include vasodilators, which can be venous, arterial or mixed, as well as ACE inhibitors (drugs with an inhibitory effect), which, in addition to heart disease, also treat renal failure - such a double the effect may be relevant for hydrothorax;)
- diuretics, which remove excess fluid from the body (carbonic anhydrase inhibitors, potassium-sparing diuretics and other types of diuretics).
Treatment regimen for hydrothorax caused by kidney disease (especially in the presence of nephrotic syndrome):
- bed rest (it promotes urine production);
- diet No. 7, which provides for a strict limitation in the intake of table salt, and in case of edema syndrome - its complete exclusion;
- control of the liquid drunk (its amount can exceed the amount of daily urine by no more than 200-300 ml);
- in case of hypoproteinemia - replenishment of depleted protein reserves in the body.
Correction of protein metabolism disorders is carried out:
- sufficient protein intake from food (primarily meat, beans);
- medication prescriptions.
Drug regulation is carried out using medications such as:
- drugs that reduce the loss of proteins in the urine (ACE inhibitors);
- protein fractions that are introduced into the body intravenously (in particular, albumin is used);
- diuretics (potassium-sparing drugs).
The basis of prescriptions for hydrothorax caused by cirrhosis of the liver is:
- diet No. 7 with a limitation on the amount of liquid drunk (no more than 1.5 liters per day) and table salt eaten;
- control over the consumption of a sufficient amount of proteins (their daily dose should be at least 70-80 grams);
- if necessary, diuretics;
- hepatoprotectors (drugs that protect liver tissue).
If conservative treatment is ineffective and requires time for correction or is started late, a large amount of effusion accumulates in the pleural cavity. In this case, it is necessary to resort to pleural puncture. It plays both a diagnostic and therapeutic role.
Pleural puncture is an invasive, but technically simple and non-hazardous procedure , in which the chest wall is pierced and introduced into the pleural cavity in order to collect fluid and, if necessary (for example, for the purpose of reinsurance against infection), introduce medications into the cavity. Despite the fact that the pleural cavity is a rather narrow space, the patient should not fear that during pleural puncture the doctor will injure the lungs - their parenchyma is elastic and cannot be easily punctured.
A pleural puncture is performed with a special needle under local anesthesia so that the patient can be in a sitting position - thanks to this position, the fluid flows into the lower parts of the pleural cavity. In this case, the patient sits half-bent and leaning on his hands. After treating the puncture site (this is the 8th intercostal space along the mid-axillary line), layer-by-layer tissue anesthesia is performed, while the needle is pushed deeper and deeper.
When it enters the pleural cavity, a feeling of “sinking” occurs. After this, the liquid is sucked off. Suction is carried out slowly; no more than 1.5 liters of fluid are removed per puncture (even if more has accumulated). When a large amount of fluid is quickly sucked out, negative consequences of pleural puncture are possible:
- displacement of mediastinal organs;
- decrease in blood pressure.
After the procedure is completed, the needle is slowly removed, holding it perpendicular to the chest wall, and a sterile bandage is applied to the puncture site. The next day, a repeat x-ray is taken to check whether fluid is re-accumulating in the pleural cavity.
Puncture of the pleural cavity does not require special preparation of the patient. If necessary (if conservative therapy has not yet stopped the process of fluid formation in the pleural cavity), pleural puncture can be repeated several times.
Forecast
With timely detection of hydrothorax and adequate treatment, the prognosis for health and life is favorable. If the diagnosis and treatment of this condition were carried out late, hydrothorax can aggravate the severity of the underlying disease - especially for cardiovascular insufficiency.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
35, total, today
( 185 votes, average: 4.67 out of 5)
Bronchial adenoma: types, signs, treatment
Pneumococcal pneumonia: causes, symptoms, treatment, prevention
Related Posts
Localization
You will be interested: Vishnevsky Institute in Moscow: services, doctors, address, patient reviews
This pathological process can occur in several forms, the distinguishing feature being its localization:
- right-sided;
- left-sided hydrothorax of the lung;
- double-sided
The most common occurrence is bilateral hydrothorax. This phenomenon can be explained by the following fact. The presence of an underlying disease causes the accumulation of pleural fluid first in one lung (right or left). The absence of pronounced symptoms most often means the absence of correct treatment, which means that over time a similar process develops in the second lung.