- Structure of the liver
- Causes of liver cirrhosis
- Symptoms of liver cirrhosis
- Complications of liver cirrhosis
- Laboratory and instrumental methods for diagnosing the disease
- Disease prognosis
- Treatment of liver cirrhosis
An irreversible change in the structural organization of the liver as a result of chronic diseases, with a persistent violation of the functions it performs, and an increase in pressure in the portal vein system is called cirrhosis of the liver.
The disease is widespread and is in sixth place as a cause of death in the age group from 35 to 60 years, with the number of cases being about 30 per 100 thousand population per year. Of particular concern is that the incidence of the disease has increased by 12% over the past 10 years. Men get sick three times more often. The main peak incidence occurs after the age of forty.
The liver is the largest digestive and internal secretion gland in the body.
The most important functions of the liver:
- Neutralization and disposal of harmful substances entering the body from the external environment and formed in the process of life.
- Construction of proteins, fats and carbohydrates used to form new tissues and replace worn-out cells.
- The formation of bile, which is involved in the processing and breakdown of food masses.
- Regulation of the rheological properties of blood by synthesizing some of the coagulation factors in it.
- Maintaining the balance of protein, carbohydrate and fat metabolism through the synthesis of albumin, creating additional reserves (glycogen).
Causes
The main risk factors for the development of cirrhosis are considered to be:
- chronic alcoholism
- viral hepatitis
- toxic effects of industrial poisons, drugs (methotrexate, isoniazid, etc.), mycotoxins, etc.
- venous congestion in the liver associated with long-term and severe heart failure
- hereditary diseases - hemochromatosis, hepatocerebral dystrophy, alpha-one antitrypsin deficiency, galactosemia, glycogenosis, etc.
- long-term damage to the bile ducts
In approximately 50% of patients with liver cirrhosis, the disease develops due to the action of several causative factors (usually hepatitis B virus and alcohol).
Stages of the disease
The pathology progresses gradually, in total there are 4 degrees of cirrhosis:
Stages of the disease.
At the initial, 1st degree, it is difficult to identify the problem, since there are no characteristic signs of a violation. At this stage, compensated cirrhosis develops, which can be eliminated with timely drug treatment.- As grade 2 progresses, a focal fibrotic process develops in the liver, the number of destroyed hepatocytes increases, causing liver function to be impaired.
- At grade 3, liver failure is severe, the person’s condition rapidly deteriorates, most of the liver hepatocytes are destroyed. At this stage, the risk of developing complications such as pleurisy, pneumonia, hepatic coma, cancer, peritonitis, excessive internal bleeding, and liver abscess increases.
- At the last stage, organ rejection begins, since its functional tissues are completely destroyed. Even modern methods of conservative therapy are not able to stop irreversible changes, and surgical treatment will also be ineffective at stage 4. To reduce pain and suffering, the patient is prescribed strong painkillers in the form of a dropper.
Manifestations of liver cirrhosis
Complaints of weakness, increased fatigue, decreased performance and appetite, dyspeptic disorders (nausea, vomiting, bitterness in the mouth, belching, intolerance to fatty foods, alcohol).
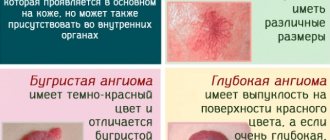
Characterized by a feeling of heaviness or pain in the abdomen, mainly in the right hypochondrium and epigastric region. Among the signs of liver cirrhosis, the so-called “liver signs” in the form of redness of the palms and spider veins (mainly on the skin of the upper half of the body) are important. Hemorrhages in the skin, as well as increased bleeding of the mucous membranes, are often observed.
Skin itching, joint pain, decreased hair in the armpits and pubic area, and decreased libido are noted. Body temperature rises moderately or remains within normal limits.
Asthenic syndrome is often observed, manifested by weakness, increased fatigue, irritability, tearfulness, and mood instability. Patients are impressionable, often touchy, picky, suspicious, and prone to hysterical reactions. Characterized by sleep disturbances - insomnia at night, drowsiness during the day.
The course of cirrhosis of the liver can be caused by colds, violation of the regime, and alcohol consumption.
Diagnostics
The diagnosis of liver cirrhosis in the early stages presents significant difficulties, since the disease develops gradually and initially does not have pronounced manifestations.
Ultrasound, X-ray and radionuclide research methods are essential in recognizing liver cirrhosis. Quite accurate information about the condition of the liver in cirrhosis can be obtained using computed tomography.
Radionuclide study of the liver - scintigraphy is inferior in its information content to ultrasound and computed tomography, but unlike them, it also allows one to assess the function of the organ.
Crucial in the diagnosis of cirrhosis is the examination of liver tissue obtained by puncture biopsy - blind or targeted, carried out under ultrasound control or laparoscopy.
Complications
If liver cirrhosis is not treated promptly, the following serious consequences develop:
Without treatment, serious complications are possible.
ascites;- peritonitis;
- varicose veins of the digestive organs;
- hepatic encephaly;
- disturbance of consciousness;
- degeneration of fibrous tissue into a malignant tumor;
- hepatopulmonary syndrome;
- disruption of the digestive tract;
- death of the patient.
Treatment of liver cirrhosis
Limit mental and physical stress. In general good condition, therapeutic walking and therapeutic exercises are recommended. Women with active cirrhosis should avoid pregnancy.
Compensated inactive cirrhosis of the liver, as a rule, does not require drug treatment. In addition, you should generally limit your intake of medications, especially sedatives, as much as possible.
In sub- and decompensated forms, the choice of drug therapy is determined by the nature of the main manifestations of the disease. In case of low protein levels in the blood, anabolic steroids and transfusions of albumin and plasma solutions are prescribed. The presence of anemia is an indication for the prescription of iron supplements. For edema and ascites, limit fluid intake, exclude table salt from the diet, and prescribe diuretics (hypothiazide, furosemide) in combination with aldosterone antagonists (spironolactone). Paracentesis is performed according to vital indications, releasing no more than 3 liters of fluid at a time.
The so-called hepatoprotectors are also used - B vitamins, orotic acid, liver extracts and hydrolysates, silibinin (legal), Essentiale, etc.
If the process is active, the same drugs are used as for chronic active hepatitis, the main ones being hormones (prednisolone) and immunosuppressants (azathioprine, etc.). Their effectiveness is inversely related to the depth of structural restructuring of the liver tissue and in advanced stages of liver cirrhosis is close to zero.
To prevent infections, all patients with liver cirrhosis are prescribed prophylactic antibiotics during any interventions (tooth extraction, sigmoidoscopy, paracentesis, etc.). Antibacterial therapy is also indicated even for mild infectious processes.
General advice for patients with liver cirrhosis:
- Rest as soon as you feel tired.
- Avoid heavy lifting (this may cause gastrointestinal bleeding)
- Aim for stool frequency 1-2 times a day. Patients with liver cirrhosis are recommended to take lactulose (Duphalac) to normalize intestinal function and the composition of the intestinal flora in favor of “good” bacteria. Duphalac is prescribed in a dose that causes soft, semi-formed stools 1-2 times a day. The dose ranges from 1-3 teaspoons to 1-3 tablespoons per day, selected individually. The drug has no contraindications; it can be taken even by small children and pregnant women.
- To improve digestion, patients are prescribed multienzyme drugs. If there is fluid retention in the body (edema, ascites), it is necessary to limit the intake of table salt to 0.5 g per day, liquid intake to 1000-1500 ml per day.
- Measure your body weight and abdominal volume at the navel level daily (an increase in abdominal volume and body weight indicates fluid retention);
- Every day, count the fluid balance for the day (diuresis): count the volume of all liquid taken orally (tea, coffee, water, soup, fruit, etc.) and count all the liquid released during urination. The amount of fluid released should be approximately 200-300 ml more than the amount of fluid taken.
- To monitor the extent of damage to the nervous system, it is recommended to use a simple handwriting test: write a short phrase, for example, “Good morning,” in a special notebook every day. Show your notebook to your relatives - if your handwriting changes, contact your doctor.
Diet for liver cirrhosis
Excluded from the diet:
- mineral waters containing sodium;
- alcohol;
- salt, food must be prepared without adding salt (salt-free bread, crackers, cookies and crispbreads, as well as salt-free butter are consumed);
- products containing baking powder and baking soda (cakes, biscuits, cakes, pastries and regular bread);
- pickles, olives, ham, bacon, corned beef, tongues, oysters, mussels, herring, canned fish and meat, fish and meat pate, sausage, mayonnaise, various jarred sauces and all types of cheeses, ice cream.
It is recommended to use seasonings in cooking: lemon juice, orange zest, onion, garlic, salt-free ketchup and mayonnaise, pepper, mustard, sage, cumin, parsley, marjoram, bay leaf, cloves.
Allowed is 100 g of beef or poultry, rabbit or fish and one egg per day (one egg can replace 50 g of meat). Milk is limited to 1 glass per day. You can eat low-fat sour cream. You can eat boiled rice (without salt). Any vegetables and fruits are allowed, fresh or in the form of dishes prepared at home.
Sample daily menu for a patient with cirrhosis of the liver:
- Breakfast: cereal porridge (semolina, buckwheat, millet, barley, oatmeal) with cream and sugar or baked fruit. 60 g of salt-free bread, or bread (slices), or salt-free crackers with unsalted butter and marmalade (jelly or honey), 1 egg, tea or coffee with milk.
- Lunch: 60 g beef or poultry or 90 g white fish, potatoes, herbs, fruits (fresh or baked)
- Afternoon snack: 60 g of salt-free bread or crispbread, unsalted butter, jam or tomato, tea or coffee with milk.
- Dinner: soup without salt, beef, poultry or fish (as for lunch), potatoes, greens, fruit or jelly made from fruit juice and gelatin, sour cream, tea or coffee with milk.
Read more about nutrition for liver cirrhosis in our separate article.
Forecast
Life expectancy with liver cirrhosis depends on the degree of compensation of the process. Approximately half of patients with compensated (at the time of diagnosis) cirrhosis live more than 7 years.
With decompensated cirrhosis, 11-41% remain alive after 3 years. With the development of ascites, only a quarter of patients survive 3 years. Cirrhosis has an even more unfavorable prognosis, accompanied by damage to the nervous system, in which patients in most cases die within a year.
The main causes of death are hepatic coma and bleeding from the upper gastrointestinal tract. Patients with liver cirrhosis have limited ability to work (disability group III), and with decompensated cirrhosis, active forms of the disease and complications, they are disabled (disability groups II and I).
Pathological anatomy
Liver cirrhosis in the initial stage is manifested by obesity of hepatic epithelial tissue. Fatty liver leads to enlargement of the organ. The liver can remain in the obese stage for many years. Over time, obese liver cells become necrotic, and in their surroundings a reaction from mesenchymal elements develops and connective tissue grows. This is how epithelial hepatitis turns into cirrhosis of the liver.
Alcohol affects the peripheral zones of the hepatic lobules earlier and more severely. Naturally, the connective tissue grows mainly in the peripheral parts of the lobules, which creates an ampullary, or interlobular, type of cirrhosis. Instead of dead cells, new ones are formed, and the entire organ is permeated by foci of regeneration, creating a perverted pattern (restructuring) of the liver parenchyma.
Very often, degenerative phenomena are hardly noticeable in the liver tissue. In particular, there is no obesity of the epithelium. Although the decrease in the cellular composition of the organ can be significant and the liver appears atrophied, changes are striking not in the parenchyma, but in the mesenchyme. In such cases, connective tissue manages to accumulate in the liver in large quantities. Over time, it undergoes wrinkling. For alcoholic cirrhosis of the liver, the intense and relatively early nature of this wrinkling is typical, therefore, often in such cases, the first symptoms in the clinical picture are congestion in the portal vein, in particular, ascites. But sometimes degenerative changes turn out to be especially extensive and occur so quickly that patients die with a picture of liver functional failure before the signs characterizing the second stage of the disease appear.
Laennec cirrhosis is characterized by changes in the vascular system of the liver. They are studied through the pouring method. This reveals not only a general decrease in the vascular bed, especially the branches of the portal vein, but also a distortion in the course of the vessels and the architecture of the vascular network. So, if you fill the portal vein with a contrast mass, you can see that some of its branches flow directly into the hepatic veins, bypassing significant areas of the parenchyma, especially the nodes of the newly formed liver tissue (the vessels of these nodes can only be filled through the hepatic artery). Some sections of the liver tissue are completely devoid of hepatic veins.
A characteristic element in the pathological picture of Laennec cirrhosis is the development of numerous anastomoses or collaterals of the veins of the abdominal viscera. Alcoholic cirrhosis of the liver more often than other forms and especially early leads to portal hypertension. From this point of view, portal cirrhosis is presented as a special vascular disease in which the liver suffers as a result of disorders of the portal system. Some confirmation of this is provided by changes in the umbilical vein and its branches (veins of Sappey, Burov), which are normally closed, but in patients with cirrhosis appear to have retained their lumen. In this regard, the so-called Cruvelier-Baumgarten disease (syndrome) is especially instructive, in which an exceptional degree of dilatation of the veins of the umbilical region is observed due to the complete preservation of the lumen of the umbilical vein of congenital origin. In this form, in addition, there is usually stenosis of the inferior vena cava at the junction of the hepatic veins. However, these abnormalities in the venous system are observed only in some cases of portal cirrhosis and cannot refute the general idea that portal hypertension is usually still a secondary syndrome dependent on primary liver damage.