Peritonitis is a severe complication, inflammation of the peritoneum caused by destruction of the abdominal organs as a result of inflammatory processes or unsuccessful abdominal surgery. Undetected peritonitis threatens the patient’s life and is the cause of death in 25-30% of cases in gastroenterology.
Causes and symptoms of peritoneal inflammation
The most common causes of inflammation of the peritoneum are diseases of the gastrointestinal tract and their complications. Often the starting point for the development of peritonitis is perforation of a gastric ulcer or duodenal ulcer. The sudden entry of the contents of these organs into the abdominal cavity causes a very strong reaction on its part.
In most cases.
Thin or thick perforation, which occurs due to various reasons (during typhus, tuberculosis, syphilis, fungal infection or intestinal cancer), causes similar consequences. As well as intestinal rupture due to direct injury. Acute appendicitis is another very common cause of inflammation of the peritoneum.
Another cause of peritonitis may be the transfer of infection to the peritoneum from the tissues surrounding the intestines. Determining this cause of peritoneal inflammation can be difficult if the patient is unable to give a comprehensive interview about the disease.
Pain, as a symptom of developing peritonitis, is initially localized in the area of the organ in relation to which the original cause of the disease is associated (for example, in the right lower abdomen with inflammation of the appendix).
The pain gradually covers the entire abdominal cavity. Its character largely depends on the underlying cause. The pain is often accompanied by vomiting or nausea. The development of inflammation of the peritoneum is accompanied by retention of gases and stool.
Other symptoms of peritonitis include:
- bloating;
- pain or tenderness in the abdominal area;
- fever;
- fluid in the abdominal cavity;
- gases, constipation;
- problems with urination;
- nausea and vomiting;
- polydipsia;
- chills.
Surgical treatment of peritonitis
Preoperative preparation of patients suffering from peritonitis begins with an infusion of crystalloid plasma substitutes: isotonic sodium chloride solution, glucose with the addition of potassium potassium chloride, vitamins, panangin. In order to restore the volume of circulating blood, colloidal and protein preparations (gelatinol, polyglucin, plasma, protein, albumin) are administered. It is almost impossible to completely correct hemodynamic disorders and water-electrolyte metabolism before surgery. Doctors are making every effort to stabilize arterial and central venous pressure and increase diuresis.
If there are signs of hypovolemic shock and cardiac dysfunction, the following drugs are added to the infusion solutions:
- Glucocorticoid hormones (prednisolone, hydrocortisone);
- Cardiac glycosides (strophanthin, korglykon);
- Antioxidants (tocopherol);
- Vitamins B and C.
In the presence of metabolic acidosis (shift in blood pH to the acidic side), sodium bicarbonate is administered.
Surgical intervention for peritonitis is associated with mechanical destruction of biological barriers that delimit foci of destruction. For this reason, doctors prescribe antibiotics to create their therapeutic concentration in tissues that are not affected by the infectious process. Preference is given to third-generation cephalosporins in combination with metronidazole-type drugs. At the late stage of widespread peritonitis, antibiotics of the carbopenem group (meronem, tienam) are used.
During the operation, surgeons perform the following main stages of surgery:
- Total laparotomy;
- Exhaustive examination of the abdominal cavity;
- Elimination of the source of peritoneal inflammation;
- Adequate sanitation of the abdominal cavity by chemical and physical means;
- Rational drainage with wide-lumen drainages located in the most sloping areas of the abdominal cavity);
- Decompression of the gastrointestinal tract (nasointestinal intubation);
- Temporary or final sealing of the abdominal cavity, taking into account the severity of purulent-inflammatory changes in the tissues of the abdominal cavity and abdominal wall.
The final stage of the operation is to create conditions for prolonged sanitation of the abdominal cavity in the postoperative period.
Prevention and treatment of peritoneal inflammation
The diagnosis of peritonitis is made based on characteristic symptoms, a physical examination and laboratory tests, which include blood tests, x-rays and computed tomography scans of the abdomen.
Peritonitis does not always lead to damage to any organ, however, the cause must be found as quickly as possible, and treatment must be taken as soon as possible, because inflammation of the peritoneum can be life-threatening and also cause various complications.
Complications depend on the specific type of inflammation. The most common ones include:
- intraperitoneal adhesions (abnormal permanent connections between two inflamed areas of the surface of the peritoneum; sometimes adhesions can occur between the peritoneum and intestines);
- recurrent intestinal obstruction - have a close connection with the adhesions described above, because they lead to difficulty in the movement of intestinal contents.
- intraperitoneal and subdiaphragmatic abscesses are closed cavities containing pus, separated from the rest of the abdominal cavity by adhesions. Their opening may be the starting point for re-inflammation of the peritoneum.
Treatment consists mainly of surgery and eliminating the cause of inflammation of the peritoneum, for example, filing a stomach ulcer or removing appendicitis. In addition, treatment with antibiotics and analgesics may be used.
Inflammation of the peritoneum (peritonitis)
develops when pathogenic microbes invade it or certain chemicals enter it. The peritoneum is a two-layer membrane that lines the abdominal cavity and surrounds the stomach, intestines and other abdominal organs. This membrane supports the abdominal organs and protects them from infection; however, sometimes the peritoneum itself can become infected with bacteria or other microorganisms. The infection usually spreads from organs within the abdomen. Inflammation can cover the entire peritoneum or be limited to only one abscess. A rupture anywhere in the gastrointestinal tract is the most common route for infection to enter the peritoneum. In most cases, microbes are transferred to the peritoneum directly from any inflammatory focus located in one or another organ of the abdominal cavity (acute appendicitis, cholecystitis, inflammation of the female genital organs, volvulus, etc.), as well as with penetrating wounds of the abdomen and with perforation of hollow abdominal organs (perforation of the stomach and intestines, gall bladder, etc.). Less commonly, the infection is introduced hematogenously from an inflammatory focus (angina, etc.).
Peritonitis causes a critical situation: the muscles in the intestinal walls become paralyzed and the movement of intestinal contents stops. However, with the advent of antibiotics, most people recover completely from peritonitis with proper treatment.
Methods of sanitation of the abdominal cavity for peritonitis
The main element of detoxification, which is used by doctors of the abdominal surgery department for peritonitis, is adequate intraoperative and postoperative sanitation of the abdominal cavity. For this purpose, surgeons use various methods - from simple abdominal drainage and peritoneal lavage to laparostomy and programmed relaparotomies. In the treatment of severe forms of acute diffuse peritonitis, preference is given to the last two options. They allow not only to effectively sanitize the abdominal cavity, but also to control the course of peritonitis.
Surgeons use many different drainage devices to improve drainage efficiency. Currently, silicone drainages are widely used, which are flexible, durable and do not cause bedsores of the intestinal wall if they remain in the abdominal cavity for a long time.
Drainage of the abdominal cavity, regardless of the number of drainage tubes and active aspiration, does not always contribute to adequate sanitation. In the presence of widespread peritonitis, most drainage tubes lose patency within 12-24 hours. The situation is improved by the use of active drainage.
For peritonitis, surgeons also rinse the abdominal cavity with antiseptic solutions (1-1.5% hydrogen peroxide solution, furatsilin solution at a dilution of 1:5000, 0.5% dioxidine solution, sodium hypochlorite, ozonated solutions). To rinse the abdominal cavity, surgeons usually use 4 to 6 liters of solution. Some doctors believe that it is necessary to use up to 10 liters of antiseptic solution. Washing does not always allow you to completely remove fibrin deposits, under which pathogenic microflora remains.
Surgeons sometimes use closed or open laparostomy to treat peritonitis. During closed laparoscopy, the laparotomy wound is not sutured, and the internal organs are delimited with napkins or film. In the second type of sanitation, the abdominal cavity is left open, and various frame devices are sewn into the edges of the wound (a device for bringing the edges of the wound together, zippers, ventrophils). In addition to providing a positive effect, this method leads to undesirable consequences:
- Large fluid losses;
- Disorders of all types of metabolism;
- Formation of intestinal fistulas;
- Formation of a massive adhesive process in the abdominal cavity;
- Formation of extensive defects of the anterior abdominal wall, which require repeated surgical intervention;
- Attachment of superinfection.
A more effective method of treating peritonitis is program relaparotomy. Its essence is that after the operation is completed, the surgeon only sutures the skin. Surgeons perform programmed relaparotomies in the presence of the following indications:
- Forming abdominal abscesses;
- Uncertainty about the viability of the abdominal organs;
- Massive deposits of fibrin and non-viable tissue that cannot be removed immediately;
- Postoperative peritonitis;
- Intra-abdominal hypertension syndrome;
- Peritonitis with spread of the inflammatory process to the retroperitoneal tissue.
When using this method, surgical trauma may occur as a result of repeated intervention, purulent complications of the abdominal cavity and anterior abdominal wall may develop, fistulas may form, and intra-abdominal bleeding may occur.
Minirelaparotomy is the least traumatic, when the surgeon removes 1-2 sutures from the edges of the wound and examines the abdominal cavity using the “rummaging catheter” method. Doctors at the Peritonitis Surgery Clinic use innovative methods for sanitation of the abdominal cavity - laparoscopic technologies. They allow you to perform the following tasks:
- Sanitize the abdominal cavity, correct the location of drainages, monitor the condition of intestinal anastomoses and sutures, perform suturing if a defect in a hollow organ is detected;
- Perform puncture and drainage of intra-abdominal abscesses;
- Stop bleeding using hemostatic polymer materials, perform vascular suturing, coagulation, clipping;
- Dissect emerging and formed adhesions between the abdominal organs.
- Perform laser irradiation of the abdominal cavity or treatment of the peritoneum and abdominal organs with ultrasound in an antiseptic solution.
There are two types of laparoscopic sanitation: hydropressive (mechanical impact with a washed solution) and physical (ultrasonic treatment, laser irradiation). Programmed sanitation is performed in the presence of the following indications:
- The duration of the disease is more than 24 hours;
- The source of peritonitis is pathology of the colon;
- Severe inflammatory changes in the parietal and visceral peritoneum, which are accompanied by massive, dense fibrin deposits;
- Presence of exudate with feces;
- Fluid retention after peritoneal lavage;
- Bile leakage;
- The need for visual dynamic control.
In addition to the positive aspects, laparoscopic sanitation has a number of disadvantages: the inability to perform nasointestinal intubation, the impossibility of adequate sanitation of the abdominal cavity in case of massive bacterial contamination and fibrinous deposits, poor visibility in the presence of paralytic intestinal obstruction.
Peritonitis is a serious complication of acute inflammatory diseases of the abdominal organs, violation of the integrity of hollow organs, and abdominal injuries. Despite the modern treatment methods used by the doctors of the surgery clinic, innovative methods of sanitation of the abdominal cavity, infusion therapy with the latest drugs, antibacterial therapy with the latest generation of antibiotics, the prognosis is not always comforting. If you suspect peritonitis, immediately call an ambulance and call the Yusupov Hospital. When the patient arrives, a team of surgeons, anesthesiologists, and intensive care doctors will be ready to begin providing emergency care any day of the week, regardless of the time of day.
What is the peritoneum and why its inflammation is dangerous
The peritoneum is a serous membrane covering the abdominal cavity and the surface of individual organs. Consists of pariental and visceral layers. Between them there is a cavity in which there is a small amount of sterile liquid. The shine and healthy appearance of internal organs depends on it.
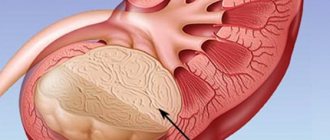
The leaves have several layers, and there are small holes on their surface. Through them, fluid can be absorbed from the abdominal cavity. The peritoneum therefore plays a critical role in maintaining a constant composition of the internal environment of the body. And if it is damaged or inflamed, then this is reflected in the activity of the whole organism. In the photo you can see characteristic changes in the internal organs during peritonitis of the abdominal cavity.
The problem of early diagnosis of peritonitis and its timely treatment is relevant, despite the development of surgery.
Features of the disease
To put it briefly and precisely, peritonitis is an inflammatory process occurring in the peritoneum.
The abdominal cavity is the volume located below the chest. It contains certain organs, such as the small and large intestines. And the peritoneum is the inner lining of the abdominal cavity.
When fecal peritonitis occurs, the activity of many organs is disrupted.
If appropriate measures are not taken in a timely manner, the pathology can cause serious damage to human health and even lead to the death of the patient.
Medical statistics show that the mortality rate from this pathology is high.
The peritoneum is a semi-permeable film, one might say - a membrane. In the body, this membrane performs many different and very important functions.
Among the main ones the following stand out:
- barrier;
- resorptive;
- exudative.
The peritoneum protects the internal organs of the abdominal cavity from the penetration of microbes. When diffuse peritonitis occurs, this protection is significantly weakened.
The resorptive function is reduced to absorbing exudate and lysis products, and the exudative function is to secrete serous fluid.
In the presence of fecal pathology, all these processes slow down or stop.
The pathogenesis of fecal peritonitis is determined by a large number of components. The rate of development of the disease depends on the volume of toxins that are absorbed by the peritoneum.
The larger the inflamed surface area, the faster toxins enter the blood. An aggravating factor in the development of fecal peritonitis is intense dehydration.
When fluid loss per day exceeds the five-liter mark, it can cause an attack of heart failure. Symptoms of this kind are associated not only with fecal peritonitis, but also with other types of peritonitis.
Depending on the type of pathology, a course of treatment and postoperative rehabilitation is prescribed.
Successful experience in the treatment of peritonitis shows that the symptoms of the pathology are ambiguous, so it is very important to pay attention to them in a timely manner.
Most often, the first signs of the disease indicate acute poisoning or stomach upset. With the fecal variety of pathology, the clinical picture looks standard.
Only an experienced doctor is able to determine the level of danger of existing signs. To distinguish between certain stages of disease development, a classification system has been created.
READ Signs and treatments for general peritonitis
According to this system, peritonitis is divided into primary and secondary.
In the first case, infection of the peritoneum occurs in the absence of an inflammatory focus in the abdominal cavity.
In this case, infection occurs through the hematogenous or lymphatic routes, and the fecal variant of peritonitis is impossible.
Secondary peritonitis spreads from purulent foci that have formed in the abdominal cavity.
For a more accurate description, experts distinguish the following types of peritonitis:
- local;
- common;
- spilled.
Local pathology affects one area of the abdominal cavity. In the second option, the lesion spreads to several anatomical sites.
Diffuse peritonitis can affect the entire abdominal cavity.
Causes
There are extremely many causes of inflammation of the peritoneum in adults and children, but they are all associated with the spread of infection into the abdominal cavity. Primary infection is rare. It is associated with infection entering the peritoneum with blood.
Secondary infection occurs as a result of a violation of the integrity of the organs of the abdominal cavity and pelvis. The causes of the development of microbial peritonitis are such pathologies.
- Appendicitis is an inflammation of the appendix. It is the cause of peritonitis in about half of the cases. This complication develops if the patient does not have the appendix removed. Due to inflammation, it ruptures and infects the peritoneum with microbes. Appendicitis and peritonitis are related: the disease is a complication of acute phlegmonous or gangrenous inflammation of the appendix.
- Perforation of a stomach or duodenal ulcer. This cause leads to peritonitis in approximately 15% of all cases. Perforation of the ulcer leads to the contents of the affected organs leaking into the abdominal cavity. Chemical, physical and bacterial damage to the peritoneum occurs, and the higher the acidity of the stomach juice, the stronger the burn.
- Gynecological and obstetric pathologies - salpingitis, salpingoophoritis, accumulation of pus in the fallopian tubes, rupture of cysts in the ovary or damage to the fallopian tube. The progression of peritonitis in women in such cases can be very severe. The disease can occur in approximately 10% of cases.
- Intestinal and biliary pathologies. In about 10% of cases, inflammation of the peritoneum can be a complication of intestinal obstruction, intestinal diverticulosis, Crohn's syndrome, inflammation of the gallbladder, or the accumulation of stones in this organ. In extremely rare cases, peritonitis can be caused by tooth infections.
- Open or closed abdominal lesions. With penetrating wounds, direct infection occurs due to the presence of microbes in the environment. With closed injuries, the disease develops due to a violation of the integrity of the abdominal organs, as well as the urinary organs.
- Factors in the development of aseptic peritonitis are fluids that are aggressive to the peritoneum - blood, urine, gastric or pancreatic juice, feces. Sometimes the disease is caused by enzymatic fluids.
Diagnostics
Timely diagnosed peritonitis in the initial stage is a person’s chance to survive. At the first suspicion of it, if the patient is not in a surgical hospital, but at home, his relatives need to know how to act competently. Acute pain in the abdomen, no matter what causes it, is a reason to immediately call an ambulance. Before her arrival, you cannot give the patient food or water, give an enema, give painkillers or a laxative. Otherwise, this will blur the clinical picture, and making a diagnosis will be difficult.
There are practically no permanent symptoms characteristic only of peritonitis. They are usually similar to its root cause - acute appendicitis, intestinal obstruction, perforated gastric or duodenal ulcer.
However, an experienced doctor will immediately establish the absence of peristalsis, abdominal breathing, tense state of the abdominal wall, acute pain on palpation, especially when the fingers are quickly removed (Shchetkin-Blumberg symptom).
Using a general blood test, it is determined that the patient has a high level of leukocytes and blood thickening is noted. A urine test reveals red blood cells. Instrumental methods for diagnosing peritonitis are radiography, ultrasound, and MRI of the abdominal organs. Laparoscopy and laparocentesis (puncture) can provide definitive confirmation of the diagnosis.
Types of peritonitis
There is a rather complex classification of peritonitis. Doctors divide the types of inflammation of the peritoneum according to many criteria.
Depending on the cause, peritonitis can be:
- traumatic;
- perforation;
- postoperative;
- bacterial.
Depending on the traumatic factor, peritonitis can be microbial or aseptic. According to the mechanism of infection, primary or secondary peritonitis is distinguished. Depending on the degree of spread, peritonitis can be local, diffuse and total.
Based on the nature of the inflammatory agent, the following types of disease are distinguished:
- serous;
- purulent;
- hemorrhagic;
- fibrinous.
Depending on the presence of exudate, exudative and dry peritonitis are distinguished.
There are also forms of the disease caused by certain bacteria. It can be caused by streptococci, mycobacterium tuberculosis, clostridia, and gonococci.
Classification
There are three stages of development of acute peritonitis: reactive, toxic and terminal. The reactive stage manifests itself and lasts the first day or two, characterized by severe pain and hyperemia of the peritoneum. Peritonitis is localized at the site of inflammation, without initially affecting other parts of the intestine. In effusion with a small amount of fibrin, there are few or no microbes and bacteria.
From the third day, acute peritonitis passes into the toxic stage, which lasts on average three days. It spreads to several parts of the intestine. The effusion becomes larger, it has a serous-putrefactive character, exudate appears, and the number of bacteria becomes significant. If there has been perforation of the organ, the exudate immediately acquires a foul odor and a dirty gray color. Intoxication of the body and dehydration occurs.
The terminal stage is final, peritonitis becomes diffuse. Purulent exudate fills the entire abdominal cavity, intestinal paresis turns into paralysis, severe swelling of the peritoneum is observed, the intestines are covered with fibrinous purulent plaque, in places the loops are glued together with it, all the volvuluses are filled with fetid liquid. The body's defenses are depleted, and the disruption of its vital functions becomes irreversible. The terminal stage lasts from 6 to 21 days. Leads to death.
Depending on the causes, age of the patient, characteristics of the body, the transition from one stage to another of acute peritonitis may be faster or more subtle; not all stages may occur. It is optimal to diagnose and treat at the very beginning of its development, at the reactive stage.
Peritonitis can be classified depending on the type of peritoneal effusion:
- serous;
- purulent;
- putrefactive;
- gall;
- fecal;
- hemorrhagic.
Peritonitis can be local and diffuse, acute and chronic. Local are divided according to location: subhepatic, interintestinal, appendicular.
There are also the following forms of peritonitis:
- tuberculosis – infection by hematogenous route;
- adhesive (sticky) – development of an adhesive process of inflammatory origin;
- chronic nonspecific – rarely diagnosed;
- postpartum – against the background of postpartum infection;
- pneumococcal – characteristic of childhood.
Main symptoms of the disease
The first sign of peritonitis is pain. With perforation of hollow organs it is very pronounced. In its strength, it resembles a sharp blow from a dagger. When the pancreas ruptures and necrosis, the pain is so severe that it can lead to painful shock.
The localization of pain is initially limited to the site of the lesion. But after a few hours, due to the spread of the pathological process, it spreads to the entire abdomen. In this case, they speak of diffuse peritonitis. Sometimes there may be a change in the location of pain.
Dangerous! The subsidence of pain is a bad symptom. This phenomenon is caused by paralysis of the intestines and accumulation of fluid in the abdominal cavity.
An equally characteristic sign is muscle tension. Maximum tension occurs with a perforated ulcer. In this case, they speak of a “board-shaped belly.” Tension may not be observed in frail and elderly patients.
A positive Shchetkin Blumberg sign is characteristic. The patient is in a supine position with the lower limbs bent. Slow pressure on the abdomen causes pain. It intensifies if the doctor suddenly removes his hand.
General symptoms of the disease are:
- elevated temperature;
- uncontrollable vomiting;
- tachycardia;
- decreased blood pressure;
- oliguria;
- sharpening of facial features (Hippocratic mask);
- acidosis;
- confusion.
Clarifying the diagnosis
Inflammatory lesions of the abdominal cavity involve listening to the patient’s complaints and taking an anamnesis. The nature of the painful sensations is clarified and the degree of intoxication is determined. During a clinical examination of the patient, palpation of the abdominal wall and abdominal cavity is performed.
Instrumental diagnostic procedures include the following:
- ultrasonography;
- radiography;
- puncturing;
- puncture through the posterior vaginal fornix;
- diagnostic laparoscopy;
- computed tomography.
These methods are necessarily used to confirm the diagnosis in combination with a physical examination and blood test.
Features of the course of different types of peritonitis
Different types of inflammation of the peritoneum may have characteristic features. It is necessary to know the manifestations of such peritonitis, since first aid and treatment should be provided as early as possible.
Dangerous! For peritonitis, any self-medication is prohibited. The patient should not be given food, drink, a heating pad, an enema, painkillers or any other medications. This can erase the characteristic clinical picture, and improper treatment can result in death.
Course of exudative peritonitis
With this disease, fluid accumulates in the abdominal cavity. It can be up to several liters. As the pathology further develops, intoxication occurs. All poisons that accumulate in the abdominal cavity are distributed throughout the body. Due to poisoning, the patient experiences multiple organ failure.
Simultaneously with the concentration of fluid in the abdominal cavity, dehydration progresses. The body also loses water during vomiting and diarrhea. Severe dehydration further aggravates the patient's condition.
Dry inflammation
In this case, a small amount of exudate accumulates in the abdominal cavity. But it contains a large amount of fibrinogen, a protein that is the main component of a blood clot. Because of this, adhesions are formed. Such peritonitis is complicated by severe hypovolemia.
Dry peritonitis often occurs during the tuberculosis process. The development of pathology leads to organ deformations.
Purulent form of the disease
This pathology is caused by pathogenic flora. As a rule, it is combined with the formation of a large amount of exudate. Most often, such peritonitis is a complication of acute purulent appendicitis.
Complications
Acute peritonitis is a condition that requires emergency care. If medical procedures are not performed in a timely manner, there is a high probability of developing such consequences as:
- formation of an abscess in the peritoneum;
- spread of the inflammatory process to the liver;
- damage to the central nervous system by toxic substances;
- dysfunction of several internal organs at the same time, which in the medical field is called multiple organ failure;
- swelling of the brain;
- the appearance of an inflammatory process in the lungs;
- severe dehydration;
- lack of intestinal motility;
- dehiscence of the postoperative wound;
- the appearance of fistulas.
In order to avoid such complications, it is necessary to promptly eliminate the diseases that caused acute peritonitis, in particular appendicitis, as well as ulcerative lesions of the stomach and duodenum. This is the only preventative measure for acute peritonitis.
Stages of peritonitis
In total, there are 3 stages of the disease.
The reactive phase lasts approximately 24 hours. The patient lies on his back with his legs bent towards the abdominal cavity. The temperature rises sharply, and the heart rate increases significantly. At the same time, nausea and vomiting appear. Consciousness is mostly clear. A positive Shchetkin Bloomberg sign is noted.
If surgical care for adults or children has not been provided within 24 hours, the disease enters the toxic stage. Its duration is up to 72 hours from the onset of the pathology. At this time, symptoms of body poisoning are observed. First of all, signs of liver and kidney failure are noted.
The main clinical phenomena are associated with dehydration and an increase in water and electrolyte disturbances. The patient is tormented by a strong and indomitable thirst. Fluid leaks into the abdominal cavity along with impaired vascular permeability. Blood pressure drops, tachycardia intensifies to 140 or more beats per minute.
With oliguria, the patient's condition worsens. The accumulation of carbamide and uric acid in the body leads to increased dehydration. All symptoms of peritoneal irritation are erased, intestinal peritonitis develops, followed by paresis of this organ.
If peritonitis is not treated and help was not provided at this time, then after 3 days from the onset of peritonitis, its advanced - terminal stage develops.
Pay special attention! The prognosis for this stage of peritonitis is unfavorable. The patient develops severe dehydration and a precomatose state. The likelihood of curing the disease is extremely low.
At the tertiary stage, the patient's face has the so-called Hippocratic mask. Facial features become sharp, and the skin becomes almost black. Sunken eyes and cheeks. Due to severe dehydration, the temples are retracted.
Symptoms
There are local and general symptoms. The first category is characterized by local abdominal pain and muscle tension. They intensify when pressed (palpation). Severe pain forces a person to lie only in the fetal position: on his side with his legs bent and brought to his stomach.
The slightest movement or attempt to change position results in severe pain
Common symptoms are nausea, weakness, rapid heartbeat, fever up to 37-390, confusion and other disorders that do not occur in the abdomen.
Fact: in this case, the abdominal muscles are in constant tension, regardless of the stage.
Stages of inflammation
Table 1. Stages of inflammation
| Stage | Local symptoms | General symptoms |
| First | Continuous abdominal pain. If you try to change your body position, the pain intensifies. | Increased blood pressure, rapid heartbeat, feeling of nausea, vomiting, dry mucous membranes. |
| Second | Soreness and tension subside as intoxication begins. | Pronounced bloating, profuse vomiting, stool retention, increased heart rate, increased temperature to 38-39 degrees, decreased blood pressure. |
| Third | Local symptoms may be mild or completely absent due to deterioration of the person’s general condition | Severe intoxication and dehydration. Dry mucous membranes, pale skin, bloating, tachycardia and low blood pressure, frequent and shallow breathing, lack of peristalsis, severe vomiting of intestinal and stomach contents. Due to the serious condition, nervous system disorders appear - delirium, confusion, mood swings. |
Treatment
Therapeutic measures are aimed at eliminating the cause of peritonitis. The patient needs urgent surgery.
In preparation for the intervention, the patient is given an anesthetic, the gastrointestinal tract is emptied, and intravenous infusion of infusion solutions is performed to replenish the volume of circulating blood.
During the operation:
- providing access to the affected area;
- elimination of the infectious focus;
- washing;
- intestinal decompression;
- washing the abdominal cavity.
Drug therapy is aimed at getting rid of the pathological focus, correcting metabolic disorders and preventing complications. The following groups of drugs are prescribed.
- Antibiotics – Benzylpenicillin, Ampicillin, Gentamicin, Sigmamycin.
- Refortan, Perftoran, glucose and other solutions for infusion.
- Calcium chloride.
- Furosemide (prescribed very carefully for disorders of water and electrolyte metabolism).
- Ibuprofen and other NSAIDs.
- Anticholinesterase drugs – Proserin, Ubretide.
- Anticoagulants.
- Anabolic steroids – Retabolil, Insulin in combination with glucose.
Note! In acute peritonitis, the use of analgesic drugs is prohibited. This applies to all pathologies belonging to the category of acute abdomen. It is forbidden to administer laxatives.
Treatment at home, as well as treatment with folk remedies and other methods of peritonitis, is impossible. Traditional methods of treatment and other recipes can cause death.
After surgery, parenteral nutrition is prescribed. In the future, as recovery progresses, the diet expands slightly.
General stages of development
The clinical picture of peritonitis depends entirely on the duration of the disease, on the nature of the inflammatory process, on the patient’s age and medical history. In surgical and gastroenterological practice, stages of peritonitis are distinguished.
First stage
The first stage (reactive stage) develops rapidly and lasts about a day. The symptoms are local in nature, the general condition of the patient is serious, and there is an expression of obvious suffering on the face. The main features include:
- severe pain;
- forced position of the patient's body;
- pallor or bluishness of the skin;
- sweating;
- uncontrollable vomiting;
- signs of intoxication;
- increase in body temperature.
The pain is constant, often localized in the area of inflammation, but there is generalization of the pain focus. Sometimes patients experience imaginary well-being due to a decrease in the intensity of pain, but the next attacks of pain occur after a couple of hours. On palpation, pain intensifies immediately after moving the hand away from the peritoneum (Shchetkin-Blumberg symptom). The patient tries in every possible way to reduce suffering by adopting a forced body position. The usual poses are on your side or on your back with your legs brought up to your stomach.
Second stage
The second stage (toxic stage) begins 72 hours after the first signs of peritonitis. Local signs gradually fade or disappear completely. The patient's facial features become noticeably sharper, the skin becomes pallor, and the nail plates turn blue. The extremities become cool or even cold. Patients are in a confused state of mind, showing complete indifference to what is happening (excessive emotional arousal occurs less often). Excitement is common in young children, for whom screaming is the only way to draw attention to pain and suffering. There is occasional loss of consciousness. The abdomen is painless on palpation. Thirst and dry mouth become painful, and constant deep vomiting does not bring any relief. The vomit takes on a dark brown color mixed with blood and has an unpleasant smell of rotting. Urinary retention is often observed, up to complete loss of urinary function. The temperature reaches 42 degrees, the pulse is barely palpable.
Third stage
The terminal stage is irreversible. The countdown begins 3-4 days after the onset of the disease. In some cases, the third stage of peritonitis almost always ends in the death of the patient. The nature of the disease is particularly severe; the external manifestations of peritonitis are the same for all patients:
- pale skin with a bluish tint;
- sharp facial features;
- no pain;
- lack of muscle tension in the peritoneum;
- breathing problems, even to the point of its absence;
- lack of pulse and blood pressure.
In the terminal stage of peritonitis, patients remain in intensive care units and are connected to artificial life support machines. At the last stage, severe multiple organ failure develops with dysfunction of almost all organs and systems.
Important! Acute diffuse peritonitis develops precisely at the second stage of pathology, when intoxication becomes more pronounced. The liver ceases to perform its detoxification function, and irreversible changes occur in the kidney structures.
Peritoneal dialysis or hemodialysis are ineffective. Laboratory blood tests reveal characteristic signs of diffuse peritonitis (increased erythrocyte sedimentation rate, pronounced leukocytosis, etc.).