The mobility and versatility of the human arm is due to the shoulder joint. Tendons and muscles provide the joint with strength and stability, thanks to which we can perform various arm movements and lift weights. A dislocation of the shoulder joint is a loss of stable position of the head of the humerus, which is located in the glenoid cavity. The causes of injury are joint dysplasia, trauma, congenital anomalies, and frequent microtrauma due to sudden swings of the arm. Professional swimming, volleyball, and tennis also provoke dislocation of the shoulder joint due to sprained ligaments.
Dislocation and subluxation can happen to anyone, so it is important to know how to provide first aid correctly and without harm, how dislocation is treated and how the shoulder joint is restored with the help of therapeutic exercises.
What is a shoulder dislocation?
Dislocation of the shoulder joint
The shoulder joint is the most mobile joint in the human body. It allows you to raise your hand, place it behind your back, and reach the back of your head.
It is believed that it was thanks to work and his hands that a person became a person, but it would not be an exaggeration to say that the entire variety of functions of the human hand is based precisely on the amazing mobility of the shoulder joint.
Movements in the shoulder joint are carried out in all three planes, but for an increase in the range of movements in the joint we have to pay for a decrease in its stability.
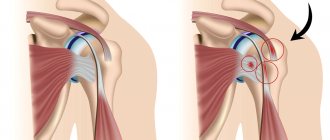
The area of contact between the head of the humerus and the glenoid cavity of the scapula is relatively small, even taking into account the cartilaginous lip that surrounds it and increases the contact area of the articular surfaces and the stability of the joint.
Thanks to the cartilage cushion located along the edge of the glenoid cavity and the connective tissue that forms the joint capsule, the head of the humerus is fixed in the correct position. The strength and stability of the joint is provided by the tendons and muscles with which it is surrounded on all sides.
The shoulder joint is formed by three bones: the head of the humerus, the glenoid cavity of the scapula and the clavicle, which is not anatomically connected to the joint, but significantly influences its function. The head of the humerus lies in the glenoid cavity of the scapula, like a basketball on a plate.
Having gained a large range of motion, the shoulder joint sacrificed stability. It is characterized by subluxations, dislocations, and ruptures of the joint capsule. Joint stability refers to the ability of the head of the humerus to remain in the correct place and not dislocate, that is, not move relative to the glenoid cavity of the scapula under the influence of external force.
Accordingly, instability of the shoulder joint is understood as a condition in which the head of the humerus can move out of the glenoid cavity of the scapula when an external force is applied or during any movements.
If normally there is only a small gap between the surfaces of the head of the humerus and the glenoid cavity of the scapula, allowing free movement in the joint, then with dislocation this small gap becomes much larger. As a result, the range of movements in the joint is significantly reduced, since the incorrect position of the articulating surfaces prevents them from being performed.
After all, in a joint, all surfaces in shape and size are carefully adjusted to each other, and if their relative position changes even slightly, the articular joint ceases to function normally.
Dislocations in the shoulder joint (it is more correct to call them dislocations of the humerus in the shoulder joint, or dislocations of the head of the humerus) are anterior, posterior and inferior, depending on where the head of the humerus has shifted.
A dislocation of the shoulder joint is, first of all, a violation of its stability. That is, under the influence of external forces, as a result of a large volume of movements performed, the head of the humerus appears outside the glenoid cavity.
Depending on the direction of its displacement relative to the articular surface of the scapula, several types of dislocations of the shoulder joint are distinguished, namely anterior, posterior and inferior.
Shoulder and its anatomical structure
The structure of the shoulder is designed in such a way that the head of the humerus fits into a special recess of the scapula (glenoid cavity) and is strengthened there by tendons and muscle fibers. Between them there is a small gap filled with a special liquid. This duet matches each other perfectly in size and roundness. All this allows a person to make various shoulder movements easily and painlessly. In the case when the structure of the presented mechanism is disrupted - the head of the humerus moves from its place, dislocation occurs.
Types of dislocations
Depending on the causes, nature and presence of complications, the entire set of dislocations of the shoulder joint is classified into the following types:
- Congenital shoulder dislocations;
- Acquired shoulder dislocations.
Acquired shoulder dislocations are divided into:
- Traumatic dislocations: uncomplicated and complicated dislocations.
- Non-traumatic dislocations (habitual): voluntary dislocation and chronic pathological dislocation.
Congenital shoulder dislocations are relatively rare and are the result of a birth injury received by a child while passing through the symphysis pubis. Diagnosis and treatment of congenital shoulder dislocations is carried out directly in the delivery room immediately after the birth of the child by a neonatologist or pediatric traumatologist.
Acquired shoulder dislocations, compared to congenital ones, constitute an incomparably larger group, since they are more common and are caused by various factors, and not just birth injuries. It is acquired dislocations that make up about 80% of all cases, and the remaining 20% are congenital.
Acquired dislocations, in turn, depending on the nature of the factor that provoked them, are divided into two large groups - traumatic and non-traumatic. Non-traumatic ones include voluntary and pathological (chronic) shoulder dislocations.
And traumatic ones are divided into two types - complicated and uncomplicated shoulder dislocations. Accordingly, uncomplicated dislocations represent an isolated injury to the shoulder joint, in which the surrounding tissues and anatomical structures are not damaged, which allows the problem to be eliminated by simple reduction.
Complicated dislocations constitute a much more diverse group, which includes dislocations that are combined with damage to surrounding tissues and structures, which makes simple reduction impossible.
Thus, the following possible options are classified as complicated traumatic shoulder dislocations:
- Open dislocation with damage to nerves and blood vessels;
- Dislocation with tendon damage;
- Dislocation with fracture of bones or cartilage (fracture dislocation);
- Pathological repeated dislocations;
- Old dislocation;
- Habitual dislocation.
Depending on the duration of the injury, dislocations are divided into three types:
- Fresh dislocation (the injury occurred within the next three days);
- Stale dislocation (the injury was received within the next three weeks);
- Old dislocation (the injury occurred more than three weeks ago).
Depending on the location and direction of divergence of the articulating surfaces, shoulder dislocations are divided into the following three types:
- Anterior dislocation (noted in 90% of cases) is a displacement of the head of the humerus towards the clavicle and deep under the scapula.
Since the head of the humerus in this type of dislocation extends under the coracoid process of the scapula, it is often called subcoracoid. However, if the head of the humerus shifts more towards the clavicle area and not under the scapula, then this type of injury is called a subclavian dislocation. With such a dislocation, the shoulder is slightly retracted to the side. - Posterior dislocation (occurs in 2% of cases) is a separation of the head of the humerus from the ligaments and tendons that hold it in its normal position, and a displacement simultaneously upward (towards the head) and towards the back. This type of dislocation usually occurs when falling on an outstretched arm.
- Inferior dislocation (occurs in 8% of cases) is a displacement of the head of the humerus downwards towards the legs. With such a dislocation, a person cannot lower his arm down and is forced to hold it above his head. With a lower dislocation, the arm is abducted from the body, and the person slightly tilts the torso towards it, holding it with the healthy arm. Let's look at a brief description of the different types of dislocations in the shoulder joint.
With this dislocation, the shoulder is abducted, flexed, and slightly rotated outward.
Anterior dislocation. It occurs most often (more than 98% of cases). Dislocation can occur as a result of injury, or it can also occur spontaneously during some unsuccessful movement (usually during movements such as “javelin throwing”). The head of the humerus moves forward and extends under the coracoid process of the scapula, which is why this dislocation is sometimes called subcoracoid.
If the head of the humerus moves further forward, it will end up under the collarbone (subclavian dislocation). In an anterior dislocation, the head tears the articular lip from the edge of the glenoid cavity of the scapula (Bankart injury). In addition, rupture of the joint capsule itself may occur.
Posterior dislocation. Occurs in 1-2% of cases. A typical mechanism of dislocation is a fall on an outstretched arm. In this case, the lip is also torn off, but not in the anterior section, but in the posterior one.
In addition to anterior and posterior dislocations, lower dislocations are extremely rare, in which the head of the humerus is displaced downwards (Latin - luxatio erecta). A distinctive feature of this dislocation is that the victim cannot lower his arm down and is forced to hold it above his head.
Causes of dislocation
Despite the relatively weak protection of the shoulder joint, habitual dislocation does not occur immediately. In a normal situation, getting this disease is almost impossible. The problem is that the life of a modern person is far from a normal situation from a physiological point of view.
A small amount of “benign” physical activity combined with a large amount of non-physiological effort (static tension during sedentary work, driving a car, carrying bags, etc.) leads to weakening of the muscles of the whole body - but specifically for the shoulder joint this can be especially fatal and lead to habitual dislocation.
However, even with weakened muscles, the first time a dislocation of the shoulder joint occurs most often due to injury, and a habitual dislocation develops as a result of improper or incomplete treatment.
Risk factors for developing recurrent shoulder dislocation include:
- Excessive mobility (hypermobility) of joints, or, as it is also called, gutta-percha. It is not so rare - in about 10% of people. People with hypermobility can perform any movement over a significantly larger range than others. Unfortunately, they are also predisposed to habitual dislocations.
- Incorrect development of the glenoid cavity of the scapula (dysplasia). It may not be as deep as in most people, or partially unformed (hypoplasia).
- Frequent microtraumas (sometimes reaching sprains) of the ligaments and joint capsule, which occur during a very wide swing (swing with a maximum or even supermaximal amplitude).
- Playing sports does not eliminate the risk of developing a habitual dislocation, and sometimes is even a provoking factor. For example, these are almost inevitable movements when practicing volleyball, tennis or certain swimming styles at a professional level (breaststroke, crawl, butterfly, and even more so when swimming on the back).
It should be especially noted that the formation of instability of the shoulder joint is a common consequence of errors in the treatment of primary dislocation. It is the resulting instability of the joint that is the main factor in the formation of habitual dislocation.
The causes of any type of dislocation may be as follows:
- Trauma (for example, a blow, a fall on your hand, etc.);
- Diseases of the joints that occur with the destruction of the articular surfaces of the articulating bones;
- Congenital anomalies of bones and joints, for example, hypermobility, shallow scapular cavity, etc.;
- Incorrect reduction of dislocation.
Symptoms characteristic of injury
After a shoulder dislocation occurs, the patient notices a loss of the oval contour of the joint, it becomes similar to an epaulette. The subclavian fossa may disappear (in the case of anterior dislocation) or, on the contrary, become convex (in the case of subclavian dislocation). The shoulder itself may look short; you can palpate the head of the joint.
If a lower dislocation of the shoulder joint occurs, there is a strong abduction of the limb, which can sometimes reach a right angle. When the head of the joint is strongly displaced, injury to the nerve fibers can occur, which ultimately leads to paresis or even paralysis of the limb, so all patients need to check the sensitivity of the end and the mobility of the fingers.
If the patient experiences severe swelling of the joint, unbearable pain or subcutaneous hemorrhages, then avulsion of the greater tubercle of the humerus can be suspected.
In order to definitively diagnose a dislocation of the shoulder joint, it is necessary to take an x-ray, based on the results of which the specialist will select the most correct and optimal method for eliminating the pathology.
Any attempts to reduce a dislocation before the X-ray image appears are medical errors, since it is impossible to palpate the full complexity of the dislocation and diagnose possible associated complications.
The appearance of the victim is characteristic: the head is tilted towards the dislocation, the shoulder girdle is lowered, the arm is moderately abducted, bent at the elbow and supported by the healthy arm. The shape of the joint is changed, a depression is determined along its upper anterior surface. There are no active movements, passive movements are sharply painful. Only adduction of the elbow joint is possible.
By palpation it is possible, but not necessary, to identify the head of the humerus in the armpit.
- Deformation of the shoulder joint caused by the displacement of the head of the humerus beyond the glenoid cavity;
- Limited movement: the hand can “spring”, but directed movements of the limb are excluded;
- Acute pain in the area of the damaged joint during primary dislocation and muted pain during habitual dislocation, especially during palpation and an attempt to move;
- Loss of sensitivity in the limb, possible numbness, tingling, as a result of nerve damage.
Symptoms of shoulder subluxation
The danger of untimely diagnosis of subluxations leads to disastrous results. Very often, a person takes recurrent pain in the shoulder area for granted and is in no hurry to seek medical help.
As a result, a pathology develops that is difficult to get rid of. Therefore, to maintain health and physical activity, it is important to promptly recognize the symptoms of the disease and carry out the necessary treatment.
The first thing you should pay attention to is the limitation of the functionality of the shoulder joint.
In addition, there are general symptoms characteristic of subluxations, regardless of their location:
- Pain of various types in the area of the damaged joint;
- Visible deformation of the connection;
- Swelling, redness of the skin, feeling of heat in the joint area and around it.
Taking into account the listed symptoms, a hardware examination is carried out using objective methods - computed tomography or fluoroscopy, MRI of the shoulder joint.
They make it possible to diagnose subluxation, in which, while maintaining the points of contact, the surfaces of the articulation are displaced, and a complete disruption of their anatomical functions occurs.
Diagnostics
The diagnosis of humeral dislocation is made based on the results of examination and additional research methods (x-ray, computed tomography, magnetic resonance imaging). During the examination, the doctor will ask you about the circumstances of the injury. Try to be as detailed as possible, but at the same time succinctly tell about what happened.
Be sure to report the symptoms described above if you have them (numbness, etc.). The doctor will examine the area of the shoulder joint itself and may conduct some tests.
The gold standard for diagnosing shoulder dislocations is radiography, which allows not only to assess the location of the head of the humerus (correct, in the anterior, posterior or inferior dislocation), but also damage to the bones themselves.
In doubtful cases, computed tomography and magnetic resonance imaging are used to clarify the dislocation. During the examination, the doctor identifies a visible deformation of the shoulder joint and tries to determine where its parts are located. After a visual examination, the traumatologist begins to carefully palpate the dislocated shoulder joint in order to determine the location of the head of the humerus.
The head has a rounded spherical shape, so it is clearly visible and palpable under the skin. With any dislocation, the head of the humerus may be shifted to the back under the shoulder blade, to the chest under the collarbone, or down.
Then the doctor takes the hand with the damaged joint and tries to make some small movement with it. When dislocated, spring resistance will be felt.
When you try to make a counterclockwise circular movement with your arm straight down along the body, a simultaneous rotation of the protruding, dislocated head of the humerus occurs. Movements in the fingers and in the elbow joint do not suffer when the shoulder is dislocated and are preserved in full.
When diagnosing a shoulder dislocation, be sure to check its response to movement and skin sensitivity, since such an injury is often complicated by nerve damage. In addition, it is necessary to feel the pulse on the artery of the forearm in the immediate vicinity of the palm and determine its strength.
If the pulse is weaker than in the healthy arm, this indicates damage to the blood vessels, which also often occurs with shoulder dislocations.
Thus, the signs that allow you to recognize a dislocated shoulder are the following:
- Deformed shoulder joint;
- Characteristic spring resistance when trying to make a movement in a dislocated joint;
- Rotation of the head of the humerus simultaneously with rotation of the outstretched and straight arm around its axis;
- Preservation of movements in the fingers and elbow joint.
However, to clarify the diagnosis of a shoulder dislocation established on the basis of the above signs, it is necessary to take an x-ray, which, in addition to confirming the diagnostic assumption, will allow you to accurately see the location of the bones relative to each other.
This, in turn, will allow the doctor to determine the most effective and least traumatic tactics for subsequent reduction of the dislocation. With habitual shoulder dislocation, as a rule, the configuration of the joint is not deformed, but movements in it are significantly limited.
Signs of habitual dislocation are various restrictions of movement in the shoulder joint, called Weinstein, Babich and Stepanov symptoms. The Weinstein symptom is that a person is asked to raise both arms to the sides 90o, and then bend them at a right angle at the elbows. The person is then asked to try to raise the forearm as high as possible.
With a habitual shoulder dislocation, the range of motion is less than on the uninjured side. Babich's symptom is that when a doctor tries to make movements with a person's hand, he resists and tries to control them on his own. Stepanov's sign is checked with the person lying on his back.
The patient is asked to extend his arms along the body and place them with his palms on the surface of the couch. Then they ask the person to turn their hands so that the backs of their hands touch the surface of the couch. If there is a habitual dislocation of the shoulder, the person cannot reach the couch with the back of his hand.
In addition, with a habitual shoulder dislocation, a doctor or other person will easily be able to lower the arm raised to the side, despite active attempts to resist. An arm with a healthy shoulder joint cannot be lowered to the body if a person actively resists this.
To confirm a shoulder dislocation suspected based on the listed signs, it is necessary to take an x-ray.
First aid
Providing first aid to the victim is as follows:
- Fixing the shoulder to the body with any available materials, or hanging the forearm on a scarf. Immobilizing the joint will reduce pain.
- Application of cold locally. Helps reduce swelling and pain.
- Administration of any painkillers and anti-inflammatory drugs (analgin, ketalgin, paracetamol, dexalgin).
First aid for a dislocated shoulder
First aid for such an injury is to apply a bandage to the injured arm, this is necessary to prevent movement of the injured arm. The patient is advised to apply cold to the affected area. It is necessary to seek help from a medical facility as soon as possible. If a shoulder is dislocated, its reduction should be done as quickly as possible, but it should also be taken into account that this should be done by a specialist.
Attention
You should not try to straighten the victim’s shoulder yourself; this may complicate the existing injury!
Bessonova Elina Sergeevna, doctor, medical observer
8, total, today
( 204 votes, average: 4.74 out of 5)
Sternum fracture: why it occurs, how to treat
Hallux valgus in a child: causes, diagnosis, treatment
Related Posts
Treatment of shoulder dislocation
At the first stage, it is necessary to perform pain relief using local anesthesia. To do this, an anesthetic solution (novocaine, icecaine, and in case of severe pain - promedol) is injected into the shoulder area.
The second stage - the reduction of the shoulder joint is performed exclusively by a doctor (in no case independently!) using one of several methods - Kocher, Hippocrates or Janelidze. Also, never try to straighten a dislocated arm or leg yourself.
In this case, certain movements are performed in the shoulder joint, which return the head of the humerus to its normal position. If it is not possible to realign the joint using these methods or a habitual dislocation occurs, then they resort to surgical treatment, when, under general anesthesia, the doctor realigns the joint and fixes it with knitting needles and sutures in the glenoid cavity.
A dislocated shoulder should be reduced as soon as possible after it develops. Reduction of a dislocation must be performed using anesthesia. Depending on the person's condition, general or local anesthesia may be used.
The simplest and most effective method of pain relief for the reduction of a dislocated shoulder is conduction anesthesia according to Meshkov. To produce it, a person is seated on a chair, asked to turn his head towards the healthy shoulder and find a point under the lower edge of the collarbone at the border of its middle and outer thirds.
Novocaine solution is injected into this point, wait 5-10 minutes until anesthesia sets in, after which they begin to reduce the dislocation by any available method.
There are more than ten ways to reduce a dislocated shoulder, among which the simplest, least traumatic and most effective are the following:
- Kocher's method.
- Dzhanelidze's method.
- The Mukhin-Mota method is applicable for any type of dislocation.
- Hippocrates' method.
First, the doctor grabs the injured arm by the lower third of the shoulder and wrist, bends it at the elbow at a right angle, and then simultaneously pulls it along the axis of the shoulder and presses it to the body. The assistant must hold the person’s shoulder while performing the movement so that it does not rise. Then the doctor turns the forearm bent at the elbow outward, so that the elbow is directed towards the abdomen. After this, turn the arm again so that the elbow is directed forward (in front of the stomach). Finally, the arm is turned again so that the elbow is near the stomach.
The person is asked to lie on the edge of a couch, table or bed, or sit on a chair so that the injured arm hangs freely over the edge. In this position, a person must lie down for 10–15 minutes to relax the muscles, after which the doctor bends the arm at the elbow at a right angle and pulls it down, while simultaneously pressing on the forearm and turning it alternately inward and outward.
The person is seated on a chair or laid on a couch, after which the shoulder blade on the side of the damaged joint is tied with a towel to the back, thrown over the armpit. Then the doctor bends the arm at the elbow and raises it to the side to shoulder level. In this position, the doctor gently pulls the hand along the axis of the shoulder, while lightly shaking and rotating it from side to side.
The person is placed on his back, the doctor grabs the hand on the side of the damaged joint by the hand and rests the leg against the armpit.
The third stage involves immobilization of the injured limb, which is necessary for speedy healing and prevention of relapses. To do this, a splint or Deso bandage is applied to the affected area for a period of one month, which will ensure complete rest.
At the fourth stage of treatment, rehabilitation is carried out aimed at strengthening the muscles and ligaments of the shoulder, which will avoid repeated dislocations. At this time, massages, physiotherapeutic procedures and special gymnastics will be useful. In general, it is worth reading the article about general symptoms and treatment of dislocations.
If the shoulder joint is weak and stress on the limb often leads to dislocation, the doctor may recommend surgery. The Bankart operation is prescribed when repeated dislocations are caused by improper functioning of the labrum.
If the doctor has diagnosed a violation of the anatomy of the shoulder joint, surgery can correct the situation. It can be performed using bone grafting, and in some cases it requires fixation of the bone with special anchors.
Surgery is often an effective means of correcting the problem. When the operation is completed, the patient is prescribed to wear a special fixing bandage, which can be removed after three weeks. After this, the patient is indicated for further rehabilitation.
Habitual dislocations of the shoulder joint occur if, after the initial dislocation, significant damage to the ligamentous apparatus and joint capsule was observed. They are caused by repeated attempts at traumatic reduction and reduction without pain relief.
Unnecessarily early resumption of exercise (for example, in athletes) contributes to joint laxity. Treatment of habitual shoulder dislocation is surgical; it is carried out in an inpatient setting. More than 150 methods of intervention have been described.
The most modern and low-traumatic method of treating habitual shoulder dislocation is arthroscopic surgery - plastic surgery of the articular labrum of the shoulder joint (Bankart operation). During arthroscopic surgery, the damaged labrum and joint capsule are fixed to the site of the avulsion from the glenoid cavity.
This makes it possible to restore the anatomy and function of the joint, significantly reduces rehabilitation time and improves the functional result.
Waiting for the doctor
If it is possible to entrust the reduction of a shoulder dislocation to specialists within 12 hours, then there is no need to attempt this complex procedure; it is better to provide first aid to the victim.
To do this you need:
- Secure the arm, bent motionlessly at a right angle, using a bandage. Any available means can serve as a bandage - scarves, belts, clothes, bedding. The forearm and elbow are conveniently located inside the bandage, the ends of which are secured to the neck so that the forearm is at chest level. This will avoid involuntary movements that can cause severe pain; and undesirable consequences in case of nerve rupture, vascular damage or bone fracture;
- Apply cold to the injured area - ice, frozen food or a damp cloth. By constricting blood vessels, cooling prevents inflammatory processes, reduces bleeding and relieves pain. Ice should be crushed for better adhesion to the surface, poured into a plastic bag and wrapped in a soft, dry cloth so as not to cause harm to the skin. Keep the compress on the sprain for 15-20 minutes per hour;
- Unbearable pain caused by injury and muscle spasm can lead to painful shock, so you should offer the victim a painkiller or muscle relaxant. When choosing a medicine, you should take into account the nature of the injury. In case of open or internal bleeding, determined by bruising and hematomas, Naproxen and Ibuprofen should be discontinued. These drugs provide good pain relief, but thin the blood, increasing bleeding. You should also not mix several medications without knowing their compatibility.
If the circumstances are such that “the rescue of drowning people is the work of the drowning people themselves” and there is nowhere to wait for help, it is not at all out of place to know how to set a shoulder yourself. But such knowledge should be used only in the most emergency situations.
Further therapy
Rehabilitation of the shoulder joint after a dislocation is no less important than the treatment process itself, so you should not neglect the recommendations of specialists. Rehabilitation involves restoring the function of the shoulder joint.
The main component of the recovery period after a dislocation should be therapeutic exercises aimed at a long period of strengthening the muscles and maintaining the normal functioning of the shoulder joint.
Main functions and purpose of exercise therapy:
- restoration of proper shoulder function;
- activation of muscle activity;
- final restoration of the joint and strengthening of muscles and ligaments to prevent future possible injury.
Gymnastics is especially important for patients who are faced with such a phenomenon as habitual dislocation. Rehabilitation and recovery after a shoulder dislocation usually takes place in four main stages. It is in the patient's best interest to go through them all.
Immediately after reduction or surgery at the initial stage:
- Immobilization of the shoulder for up to 7 days,
- Warm-up exercises with the wrist and hand for normal blood flow to the immobile part of the body,
- Cold compresses to reduce pain and swelling.
- Anti-inflammatory drugs.
At the next second stage:
- First light shoulder movements 2-4 weeks,
- If there is no pain, you can begin warm-up exercises for joint mobility,
- It is forbidden! Perform combined movements, such as abducting the arms to the sides or turning the shoulder outward - this can cause re-dislocation of the joint,
- The bandage can be removed
- After training, apply ice if there is swelling.
The third stage provides:
- Full mobility of the shoulder and shoulder joint 4-6 weeks,
- If there is no pain, you can begin to move your arm to the side,
- Continue exercises to develop mobility,
- Strive to achieve full range of motion.
At the final fourth stage of recovery after a shoulder dislocation, a return to normal activities occurs. It is already possible to lift light weights, and athletes can begin to work with strength equipment, gradually increasing the load.