Synovitis is a common cause of joint pain not only among athletes and those involved in physical labor.
Inflammation of the synovial membrane can occur in anyone, even in response to any other disease. Most often the disease affects the knee and elbow joints.
Without proper treatment, synovitis tends to become chronic, and quality of life can be seriously affected.
Synovitis of joints
Synovitis is an inflammation of the synovial membranes that line the inside of one or more large joints.
During illness, fluid accumulates in the synovial membranes. It is expressed by malaise, increased joint volume, pain and weakness. When infected, signs of intoxication appear. To be exempt from military service, synovitis must indicate dysfunction of a large joint. Our task is to explain to you what kind of disease this is, what are the reasons for the development of synovitis and what to do to quickly restore the body.
Reasons for the development of the disease
The main etiological factor provoking the development of acute synovitis is mechanical damage , which most often occurs with bruises, a fracture of the patella, rupture of the ligamentous-articular apparatus or meniscus. In this case, the formation of effusion is a protective reaction of the body.
In second place is rheumatic fever . The increase in synovial fluid occurs due to inflammatory swelling of the cartilage and its destruction by rheumatoid factors.
Chronic inflammation of the synovial membrane develops as a result of degenerative processes in the knee cartilage. With age, cartilage tissue loses its qualities, becomes thinner, leading to osteoarthritis, and with constant mechanical irritation, the amount of effusion increases to protect the bone tissue.
The cause of the development of the reactive type is infectious agents - streptococci, staphylococci, mycobacterium tuberculosis.
What is synovitis?
Synovitis is an inflammatory disease of the synovium (cavity) of the joint, characterized by excessive accumulation of effusion in it. The boundary of the inflammatory process during synovitis is limited to the synovial membrane.
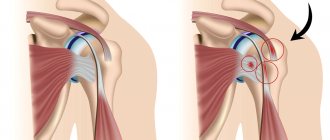
The synovial membrane-lined cavities involved in this inflammatory process can include the synovial bursa (a small flattened cavity lined with the synovial membrane, delimited from the surrounding tissues by a capsule and filled with synovial fluid), the synovial tendon sheath, and articular cavities.
With synovitis, in 65–70% of cases the knee joint is affected; the shoulder, elbow, ankle, and hip joints are much less often affected. The disease is widespread, has many variants of its course, and occurs equally often in children and adults of all age groups.
Surgery for synovitis
Knee arthroscopy
Reviews from patients who have suffered synovitis of the knee joint indicate that in most cases the disease is treated successfully with therapeutic methods and without the threat of relapse. The main thing is not to waste time and not to delay your visit to the doctor.
Advanced chronic cases, which lead to fossilization of areas of the synovial membrane, the formation of hypertrophied villi, and sclerosis of the membrane, require surgical intervention. The operation consists of removing the synovial membrane completely or partially, removing cartilage growths, foreign bodies, parts of damaged menisci, and pumping out the accumulated fluid. Knee arthroscopy is a gentle modern method of cleaning joints; however, the cost of the procedure is significantly higher than therapeutic measures and, in addition, requires a significant period of rehabilitation.
Orthopedic surgeons advise starting treatment measures immediately in the first stages of illness, and even better - remembering prevention.
Classification
Taking into account the current, the following are distinguished:
- Acute synovitis - accompanied by thickening, plethora and swelling of the synovial membrane. The effusion is a translucent liquid, sometimes with fibrin flakes visible to the naked eye.
- Chronic synovitis is manifested by the development of fibrous changes in the joint capsule. In some cases, the villi of the synovial membrane grow, and fibrinous deposits appear on the membrane, hanging from the joint cavity (villous synovitis). When separated, the deposits are transformed into so-called “rice bodies”, which move freely in the joint fluid and additionally injure the synovial membrane.
Synovitis is classified according to its location:
- shoulder joint (shoulder);
- ulnar (elbow);
- coxofemoral (hip);
- knee joint (knee);
- ankle (ankle);
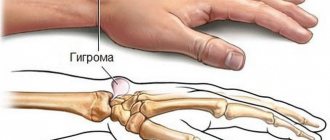
- wrist joint (wrist).
By the nature of the exudate:
- Serous;
- Serous-fibrous;
- Purulent;
- Hemorrhagic.
In addition, depending on the nature of the causative factor, all synovitis is divided into infectious and aseptic. Accordingly, infectious synovitis is caused by the entry of pathogenic microbes into the joint, and aseptic synovitis can be caused by all other causative factors, with the exception of infectious ones.
Classification of synovitis
Synovitis is classified according to:
- Form of the disease: Acute synovitis - clinical manifestations are pronounced.
- Chronic synovitis – develops over a long period. This form of the disease includes: Villous synovitis (villous) - synovial villi, responsible for expanding the useful surface during the synthesis of synovial fluid, increase and strongly protrude into the articular cavity.
- Crystalline synovitis - crystalline deposits form in the joint cavity, the cause of which is gout.
- Hyperplastic synovitis is characterized by thickening and degeneration of the synovial membrane.
- Infectious synovitis - it is caused by pathogenic microorganisms that have penetrated into the joint cavity. Specific – synovitis is caused by pathogens of specific diseases, such as tuberculosis or syphilis.
- Serous - the exudate is almost transparent, it contains low molecular weight proteins.
Reasons for appearance
Synovitis most often occurs in men, mainly under 35-45 years of age, which is due to active physical activity and age for professional sports, as well as heavy physical work. Also, the disease synovitis can plague people with reduced immunity, who often suffer from infectious diseases.
The following reasons for the development of joint synovitis are identified:
- injuries;
- infection entering the joint cavity;
- accompanying illnesses;
- allergic reactions;
- joint instability;
- increased body weight.
Non-infectious or aseptic synovitis develops differently depending on the causes. In case of traumatic injuries in athletes and people involved in physical labor, the mechanical factor comes to the fore.
Immunological disorders in rheumatism and rheumatoid arthritis lead to the fact that the antibodies produced by the body attack its own synovial membrane.
And with some metabolic disorders, synovitis is caused by the accumulation of waste products or uric acid salts (with gout) in the joint cavity.
The essence of pathology
What is synovitis? This is the name given to the inflammatory process that affects the synovial membrane of the joint. This membrane is represented by connective tissue and lines the articular cavity from the inside. The function of the synovial membrane is to protect intra-articular structures and produce fluid that serves as a shock absorber for movements.
Under the influence of a number of reasons, inflammation can occur in the synovial membrane. In this case, its function is impaired, and increased fluid formation is observed. Connective tissue loses its elasticity and smoothness. All this leads to dysfunction of the joint. In 70% of cases, synovitis of the knee joint is observed; small joints are practically not affected.
Synovitis can occur in anyone, regardless of gender and age. The classification of the disease is very extensive and includes many symptoms.
According to the nature of the flow, they are distinguished:
- Acute synovitis – no more than 3 weeks;
- Chronic – a month or more.
According to the nature of the effusion:
- Serous – clear liquid in small quantities;
- Serous-fibrinous – transparent with white flakes;
- Hemorrhagic - mixed with blood;
- Purulent – cloudy greenish;
- Villous - in this case, tissue growths appear on the synovial membrane.
Due to the occurrence:
- Infectious – caused by bacteria, viruses, fungi;
- Post-traumatic synovitis – develops against the background of injury;
- Autoimmune – caused by autoimmune processes in the body;
- Allergic;
- Metabolic for metabolic disorders in the body.
For synovitis, the ICD10 code is M65.
Tenosynovitis of the joints is similar in cause and clinical picture. The difference is that with this disease, not only the joint capsule becomes inflamed, but also the tendons. The disease is more severe, and the risk of developing joint contracture is higher.
The disease develops under the influence of external and internal causes:
- Acute and chronic injuries - ligament ruptures, joint capsules, sprains, intra-articular fractures and severe bruises;
- Infection of the joint capsule - from the outside or from chronic foci of infection inside the body;
- Allergic reaction;
- Autoimmune process;
- Metabolic disorders, endocrine diseases.
Excess weight, adherence to bad habits, physical inactivity, and poor nutrition increase the risk of developing synovitis. If inflammation develops as a result of direct damage to articular structures, it is called primary. Inflammation that is preceded by any disease is secondary synovitis.
Symptoms of synovitis + photos
Synovitis is characterized by damage to one joint or ligament; in rare cases, the disease is multiple.
General signs of synovitis:
- swelling and smoothing of joint contours
- pain on exertion, decreased range of motion in the affected area
- general increase in body temperature or local increase in skin temperature in the affected area
- general weakness, poor health.
Some of these symptoms may be more pronounced than others, but with infectious synovitis the symptoms will always be more pronounced than with non-infectious synovitis.
- With this form of the disease, the inflamed area becomes larger within the first 2–3 hours. This occurs due to the accumulation of a large volume of synovial fluid in it.
- As a rule, unpleasant sensations appear only when touching the affected area, and in a normal state a person does not experience any discomfort.
- Over time, the inflamed area becomes warm, and the patient begins to experience general malaise;
- The most characteristic symptom of this form of the disease is stiffness in the affected joint.
- Also, when performing movements in the affected joint, pain appears.
- Long-term movements in the affected joint are impossible due to rapid fatigue.
- Ultimately, this form of synovitis can lead to hydrarthrosis of the joint (hydrosis), which leads to subluxation and dislocation of the joint (due to sprained ligaments).
Symptoms of the disease
Synovitis most often affects the knee joint, followed by synovitis of the elbow, wrist and ankle joints. Symptoms depend on the cause of the disease and the nature of the inflammatory process.
With non-infectious acute synovitis, patients complain of:
- a feeling of fullness in the joint, an apparent increase in its volume;
- mild pain;
- poor general health;
- a slight increase in local temperature, sometimes the general body temperature rises;
- restriction of movements;
- pain on palpation of the joint.
In acute purulent synovitis, the following symptoms occur:
- pronounced pain syndrome;
- severe general weakness;
- increased body temperature;
- severe swelling of the joint;
- redness of the skin over the area of inflammation;
- persistent restriction of movement of the affected joint;
- enlargement of nearby lymph nodes.
Chronic synovitis is often mixed and combines various forms. Clinical symptoms are scanty, especially in the early stages of the disease. Patients note:
- slight aching pain in the joint;
- rapid fatigue of the joint when performing repetitive movements;
- slight limitation of movements.
Complications
Possible complications of synovitis:
- arthritis,
- decreased range of motion due to irreversible changes in the synovium or articular surfaces,
- spread of the process to neighboring areas of the ligamentous apparatus.
The most serious complication of infectious synovitis is sepsis, which is life-threatening. Sepsis (the appearance of a pathogen in the blood) with infectious synovitis can develop in people with a weakened immune system (for example, with HIV infection) or in case of prolonged absence of treatment.
Treatment options
There are several ways to treat synovitis. In most cases, a complex of puncture and further drug treatment is necessary. If medications do not provide sufficient effect, specialists may resort to surgery.
It must be remembered that when the first signs of synovitis occur, the knee must be secured with a tight bandage in a straightened form and contact a specialist as soon as possible to prescribe treatment.
Knee joint puncture
Puncture is both a diagnostic and therapeutic procedure.
The puncture involves suctioning out excess accumulated effusion, after which antibiotics are injected into the vacated joint cavity to prevent infection. The puncture is performed without anesthesia. The taken fluid is sent for analysis, and after establishing the type and form of the ongoing synovitis, the specialist prescribes additional treatment.
After the puncture, it is necessary to provide rest to the knee joint. A complete lack of mobility can harm the joint, so it is only recommended to reduce the load as much as possible.
Drug treatment
After determining the type and form of the disease, the specialist prescribes drug treatment for synovitis. He also prescribes the required dose and duration of medication. Drugs prescribed for the treatment of synovitis of the knee joint include:
- Analgesics and other anti-inflammatory drugs:
- Ibuprofen;
- Diclofenac
- Panoxen
- Antibiotics (to kill infection):
- Cefotaxime - injections into the muscle, one gram 3 times a day;
- Vancomycin – 0.5-1.0 g 4 times/day intramuscularly;
- Glucocorticosteroids:
- Betamethasone;
- Dexamethasone;
- Drugs to improve blood microcirculation:
- Amlodipine;
- Trental.
- Comfrey herb ointment;
- Rye broth;
- Herbal decoction;
- Bay oil;
- Black walnut tincture.
Surgery
As mentioned earlier, chronic synovitis is not always amenable to drug treatment. In such cases, surgical intervention is necessary. Also, indications for surgery may be when irreversible processes are detected in the knee joint: the formation of foreign compounds, sclerosis and atrophy of connective tissues.
During the operation, the articular cavity of the knee is opened, the surgeon removes everything unnecessary (deformed meniscus, foreign body), excises the synovial membrane, and examines all changes in the knee joint.
After surgery, anti-inflammatory and hemostatic therapy is necessary. The joint must be restored with the help of physiotherapy and exercise therapy. It must be remembered that after surgery, recurrence of synovitis of the knee joint is possible.
Treatment with folk remedies
Folk remedies in the treatment of synovitis are only an auxiliary step, and can only be used after consultation with a specialist.
Treatment with traditional methods without the use of medications often only leads to aggravation of the situation and the occurrence of chronic synovitis. Here are several folk remedies for the treatment of synovitis:
Diagnostics
Objective examination of a patient with joint synovitis:
- On examination, the following is observed: an increase in the size of the joint, swelling, smoothing of the surface, hyperemia, stiffness of joint movements.
- On palpation (palpation) one feels: a local increase in temperature, pain, swelling, fluctuation (the presence of fluid fluctuations in the joint during movement). In some cases, enlargement of regional lymph nodes can be felt.
To make an accurate diagnosis, the doctor examines the affected joint using the following methods:
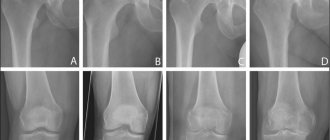
- X-ray examination;
- Ultrasound;
- puncture, during which intra-articular fluid is obtained and sent for extensive laboratory testing;
- CT or MRI.
Currently, this is done by arthroscopy, a type of endoscopy. Through a small hole in the skin in the area of the inflamed joint, a special optical device, an arthroscope, is inserted into the joint cavity.
Arthroscopy allows not only to visually assess the condition of the joint cavity, but also to carry out some therapeutic manipulations, in particular, to remove inflammatory fluid.
Laboratory research methods:
- In a general blood test, an increased erythrocyte sedimentation rate (ESR), an increased number of leukocytes, and C-reactive protein are detected.
- When examining punctate, the physicochemical properties are determined and microscopic, bacterioscopic and bacteriological analysis is carried out.
Diagnosis of synovitis
Making a diagnosis includes a certain algorithm of specialist behavior. Initially, a visual examination is performed, which determines the degree of swelling, deformation, pain and level of mobility limitation. The patient’s medical record records information about the causes of inflammation, the condition of the body and past illnesses and infections.
Next, the specialist prescribes a laboratory test, which includes a biochemical blood test from a vein, a general urine test, an immunological examination, and a collection of synovial fluid from the inflamed knee.
Important ! For a more accurate diagnosis, an ultrasound examination of the knee, X-ray, or arthroscopy may be prescribed.
Treatment of synovitis
As soon as a person notices any symptoms of the disease, he should immediately consult a doctor. The specialist will conduct an examination, study the results of examinations, establish an accurate diagnosis and prescribe competent treatment for synovitis.
Treatment of acute serous synovitis must be carried out with initial immobilization of the limb using a plaster splint. How to treat synovitis at the initial stage:
- UHF therapy,
- UV irradiation,
- electrophoresis with novocaine,
- warming compresses with dimexide solution.
If synovitis is severe, the doctor prescribes:
- electrophoresis with lidase,
- electrophoresis with potassium iodide,
- phonophoresis with glucocorticosteroids.
If the symptoms of synovitis are only a large amount of effusion in the synovial cavity and general weakness, then puncture of the joint with the possible addition of antibiotics is necessary.
It should be noted that therapeutic puncture is performed only when the infectious nature of synovitis is excluded.
The following contraindications for performing therapeutic puncture of the joint are identified:
- blood clotting disorder;
- infection of the skin in the area where the needle was inserted;
- presence of a wound at the site where the needle was inserted.
Read also: Why knees swell
Treatment of chronic serous or serous-fibrinous synovitis involves ensuring rest of the affected limb, performing joint punctures, prescribing physiotherapeutic procedures (electrification, paraffin applications, mud therapy and others). It is necessary to identify and treat the underlying disease that caused chronic synovitis.
In some advanced cases, it is necessary to resort to surgical treatment - synovectomy, which amounts to complete or partial excision of the synovial membrane of the joint capsule and is performed under endotracheal anesthesia.
For any type of disease, immobilization is indicated, that is, immobilization of the joint using a knee pad or bandage; they must be worn for at least a week. Elevation of the limb is also sometimes recommended.
Medicines for synovitis
Drug therapy is prescribed in several directions:
- After joint puncture, intra-articular administration of broad-spectrum antibiotics is prescribed. This is necessary to prevent infection or to eliminate it if the bacterial nature of the disease is established.
- Doctors prescribe NSAIDs (diclofenac, voltaren, ibuprofen, indomethacin) in the form of ointments, injections or oral medications to almost all patients with this diagnosis.
- It is also possible to administer intra-articular corticosteroids in combination with physiotherapy (magnetic therapy, ultraviolet irradiation, ozokerite, UHF, paraffin, phonophoresis).
- To restore microcirculation, the use of Thiotriazolin, Trental, and Nicotinic acid is indicated.
If there is no positive effect after a course of drug treatment, or if the symptoms of synovitis intensify, surgical treatment is prescribed. Under local or general anesthesia, the patient is subjected to opening the joint, cleaning its internal cavity, and rinsing it with antibacterial and drying solutions.
In the presence of “foreign” structures - bone and/or cartilage formations, as well as bone fragments after a joint injury - the surgeon performs a kind of plastic surgery, restoring the uniformity and uniformity of its internal surface.
Complete restoration of the affected joint due to synovitis is possible no earlier than after 2–3 months. Even if the patient’s condition allows him to resume his usual lifestyle at an earlier date, it is better to maintain a gentle regimen during this period of time. This will completely eliminate the inflammatory process, prevent its reoccurrence and transition to a chronic form.
Timely diagnosis of the disease and medical or surgical treatment can significantly increase the patient’s chances of full or partial recovery and restoration of joint mobility.
Treatment tactics
Therapy for synovitis is carried out simultaneously with the treatment of the pathology that caused its development. Therefore, consultation with a traumatologist, venereologist, infectious disease specialist, neurologist, gastroenterologist, and endocrinologist may be required. In case of acute aseptic or infectious synovitis, the patient is hospitalized. The doctor uses a puncture to remove the accumulated exudate, and then washes the joint cavity with solutions of antiseptics, glucocorticosteroids or antibiotics.
After applying a tight bandage, treatment is carried out in the department under the supervision of medical personnel.
Therapy for chronic sluggish synovitis consists of eliminating the factors that provoked it. The patient is advised to take medications at home. Recurrent chronic synovitis, accompanied by degeneration of the tissues of the joint capsule, practically does not respond to conservative therapy. During surgery, the doctor completely or partially excises the inflamed synovium.
Non-drug therapy
To reduce the severity of pain and prevent excessive stress on the injured knee, patients are recommended to wear orthopedic devices. For severe inflammation, semi-rigid orthoses, bandages and knee pads with metal or plastic inserts are used.
To reduce the symptoms of synovitis at the initial stage, it is enough to wear a soft elastic bandage that only slightly restricts movement. Physiotherapeutic measures must be included in treatment regimens:
- magnetic therapy;
- electrophoresis, phonophoresis using solutions of anesthetics, analgesics, chondroprotectors;
- laser therapy;
- UHF therapy;
- sinusoidally modulated currents;
- applications with ozokerite, paraffin, medicinal mud.
Immediately after the inflammatory process has stopped, the patient is recommended to perform special exercises to improve the functioning of the joint. The complex is compiled by a physical therapy doctor, and the first classes are held under his supervision.
Pharmacological drugs
Severe pain that occurs during the acute form of synovitis is eliminated by parenteral administration of glucocorticosteroids - Diprospan, Triamcinolone, Flosterone, Dexamethasone. These hormonal agents not only have an analgesic effect, but also exhibit pronounced anti-exudative and anti-inflammatory activity.
Often they cannot be used due to the toxic effect on the human body, therefore, after the pain has subsided, glucocorticosteroids are replaced with non-steroidal anti-inflammatory drugs:
- tablets - Ibuprofen, Nise, Ketorol, Nurofen, Ketoprofen, Meloxicam;
Approximately on the 3-4th day of treatment, after relief of inflammation, patients are recommended to use ointments with a warming effect (Finalgon, Capsicam, Apizartron) to improve blood circulation in the knee.
If destructive changes have occurred in the articular structures, then chondroprotectors (Structum, Artra, Teraflex) are included in the therapeutic regimens, stimulating the regeneration of damaged tissues.
Compliance with all medical recommendations allows you to quickly get rid of all the symptoms of synovitis. The prognosis for full recovery is favorable. Complications in the form of contractures occur only with severe purulent synovitis. Timely seeking medical help will help you avoid such negative developments.
How to treat synovitis of the knee joint?
Content:
Synovitis of joints is inflammation of the synovial (inner) membrane that covers the joint cavity. During the inflammatory process, effusion is formed, fluid accumulates in the joint capsule. When infection penetrates, the effusion turns into purulent contents - at this point purulent synovitis develops. More often, inflammation affects the knee joint, since it experiences significant stress.
Based on the reasons that caused the disease, infectious or non-infectious synovitis is distinguished, based on the nature of its course - chronic or acute.
Diagnosis of inflammation of the synovial bursa of the knee joint
The traumatologist will primarily prescribe extensive three-way radiography to his patients. The resulting images should reflect the main cause of the disease, that is, injury, bruise or rupture of the joint. As well as the exact localization of the inflammatory process and fracture. This method is the most popular and accessible. The second step of the diagnostic study is puncture of the synovial bursa. Color, concentration, the presence of blood or pus, as well as tissue debris during visual inspection of the serous contents tell about the stage of the disease. Biochemical analysis of exudate and blood shows the amount of protein and salts. Culture of the serous contents determines the type of infectious agent. In addition to radiography and puncture, intra-articular endoscopy, computed tomography, ultrasound examination of the knee joint and MRI are performed. These diagnostic studies are performed for all types of synovitis.
In the case of non-infectious synovitis, consultation with specialists such as a gynecologist, urologist, endocrinologist, allergist or rheumatologist is required.
Directions for treating synovitis
As a rule, the symptoms of synovitis of the knee joint are clearly expressed: there is pain, there is a change in the shape and limitation of joint mobility, and the temperature rises. A person should consult a doctor as soon as possible. Treatment of patients usually involves complex therapy, taking into account the causes of the disease, as well as the course of the pathological process.
To eliminate joint functions impaired by inflammation, doctors recommend general strengthening therapy, physiotherapy and physical therapy. The actions of doctors are, of course, aimed at identifying the causes and eliminating them, as well as at removing, first of all, such obvious symptoms of the disease as pain and dysfunction. Surgery, as one of the treatment methods, is rarely prescribed if there is no positive effect from conservative treatment methods or if there is a threat to the patient’s health (the development of sepsis).
Main stages of the disease
There are several stages/forms of development of synovitis disease. Let's take a closer look at each of them.
Minimal synovitis of the knee joint
It may be painless. There is no pronounced inflammation, discomfort manifests itself in the form of a pulling sensation. The temperature is within normal limits. Painful sensations appear only upon palpation of the affected joint. It is quite difficult to determine the disease on your own, and this is one of the dangers - minimal synovitis can turn into chronic.
Acute synovitis of the knee joint
The acute form of the disease of the knee joint is accompanied by severe pain and difficulty in the normal functioning of the limb. In acute synovitis, a purulent infection often occurs, accompanied by severe inflammation of the joint and fever.
If you suspect an infection, you should immediately contact a specialist who will prescribe the necessary treatment.
Secondary synovitis of the knee joint
This type of synovitis is observed in people diagnosed with arthritis, arthrosis, osteoarthritis. With these diseases, a special load falls on the joint, which leads to its deformation and the accumulation of effusion.
A feature of secondary synovitis of the knee joint is its recurrence. Knee deformity, nagging pain, difficulty moving and swelling - all symptoms arise and disappear within 3-7 days. Then all signs of the disease disappear and return again after 2-3 months.
Moderate synovitis of the knee joint
Moderate synovitis is insidious due to its relatively painless form of the disease. The knee begins to bother you only a few days after receiving the injury. There is always pain, swelling of the knee joint, and difficulty moving.
In the acute form of moderate synovitis, the temperature may rise, chills may appear, and symptoms of fever may be observed. But since all these signs are of a moderate nature, the patient has a false confidence that the disease is in its final stages. Due to the lack of treatment, moderate synovitis very often turns into a chronic form of the disease.
Chronic synovitis of the knee joint
The form of chronic synovitis is quite rare and usually has signs of minimal synovitis. There is rapid fatigue and limited movement, crunching in the knee joint. The number of dislocations increases, and wear and tear of the joint is observed.
With chronic synovitis, there are completely no signs of fever or infection in the body. However, the disease can be in remission for a long time, followed by a sharp deterioration and exacerbation of all the above symptoms.
The result of chronic synovitis can be special forms of pathology of the knee joint, the treatment of which will require surgical intervention.
Stages of treatment
Usually, the attending physician decides how to treat synovitis of the knee joint, based on the reasons that caused it, the stage of the disease and the nature of the course. The doctor must prescribe a comprehensive examination of the entire body in order to find out what exactly triggered the development of knee synovitis, to monitor the development of inflammation, and to predict possible complications in the patient.
First, a puncture of the diseased joint is performed. The procedure is performed by experienced surgeons. Anesthesia is not required during this procedure, since the patient practically does not feel pain, only some discomfort. The specialist inserts a thin needle into the joint area and sucks out synovial fluid (effusion). The resulting exudate is sent to the laboratory for testing.
The next stage of treatment is joint immobilization. Its goal is to ensure complete peace. Doctors apply splints, plaster splints, and pressure bandages. The choice of the most appropriate method of temporary immobilization is determined by the nature of the disease. So, with minimal synovitis of the knee joint, it is enough to use a pressure bandage or a special patella. And if infectious synovitis is accompanied by severe damage to the joint, rigid immobilization with plaster splints or splints will be required. This stage of treatment usually does not exceed seven days.
Prevention measures ↑
Prevention involves avoiding joint damage.
If gonarthrosis of the knee joint or arthritis occurs, synovitis can be avoided by performing the prescribed therapy on time and correctly.
If synovitis occurs once, it is necessary to strictly monitor it in the future in order to give minimal chances of developing a relapse.
To do this you need:
- exercise regularly, but ensure proper knee flexion
- avoid increased physical activity
- don't overeat
- monitor the maintenance of body weight within individually acceptable values
- If you feel pain, crunching or loss of mobility in your knee, consult a doctor.
Thus, synovitis of the knee joint is a rather serious disease that can develop as a result of a huge number of reasons.
There is a whole arsenal of medication and complementary therapy for its treatment, however, the disease is very difficult to treat.
Treatment methods
Methods of drug treatment of the disease
Taking medications prescribed by a doctor leads to a speedy recovery. If you do not follow the doctor's instructions, various complications may occur, including joint destruction, sepsis and suppuration.
There are several groups of drugs prescribed for the treatment of synovitis:
- Anti-inflammatory non-steroidal drugs. They effectively eliminate pain and reduce inflammation. Moreover, drugs in this group are available in the form of tablets, injections, suppositories and ointments, which allows you to get good results. In some cases, the doctor prescribes the administration of drugs rectally - suppositories reduce the load on the gastrointestinal tract, but are as effective as tablet drugs, which are not always convenient to use. In the form of suppositories and tablets, Nise, Diklak, Ketonal, and Analgin are popular. Gels and ointments are applied externally to the joint: Ketonal, Indomethacin, Diclofenac, Voltaren.
- Proteolytic enzyme inhibitors. The drugs are quite effective in the treatment of chronic synovitis of the knee joint. The disease at this stage occurs with infiltration of the affected joint, with a large volume of effusion. Treatment is a course - drugs are injected into the joint after puncture. They use medications - Gordox, Trasylol.
- Corticosteroids. In malignant, very severe forms of the disease, intra-articular administration of steroid hormones is prescribed: Kenalog-40, Dexamethasone.
- Microcirculation regulators. To normalize microcirculation disturbed by the inflammatory process, doctors prescribe ATP, Nicotinic acid, Trental or Thiatriazolin.
- Antibiotics. After the puncture, the doctor introduces antibiotics into the cavity of the diseased joint (broad-spectrum drugs are used) in order to prevent the addition of a secondary infection or if the disease is confirmed to be bacterial;
- Dietary supplement You should take the prescribed vitamin and mineral complex.
Surgical method of treatment
There are cases when conservative treatment of synovitis of the knee joint does not produce results, but, on the contrary, contributes to the progression of the disease. This is evidenced by rare reviews from patients. In such cases, doctors use surgical treatment methods - they perform a total or subtotal synovectomy. During the operation, the surgeon opens the joint cavity, performs resection of the synovial membrane, and removes foreign bodies from the joint cavity.
Afterwards, anti-inflammatory, hemostatic and antibacterial therapy is carried out. During the recovery period, rest and reduction of stress are indicated to prevent the re-development of synovitis. As soon as the patient’s condition improves, the doctor prescribes physiotherapy and exercise therapy to “develop” the joint.
Read also: Articular fluid in the knee joint
Folk remedies in the fight against disease
There are many traditional methods of treating this disease. However, they are not able to completely cope with the disease on their own, even if the synovitis of the knee joint is moderate. They are allowed to be used in conjunction with other treatment methods, with the obligatory approval of a doctor.
Medicinal comfrey is useful. Compresses promote rapid tissue healing and prevent the development of necrosis.
You can prepare an infusion for drinking. To do this, mix crushed herbs of mistletoe, echinacea, eucalyptus, yarrow, tansy, thyme, oregano, and birch leaves. Take a spoonful of the mixture and pour a cup of boiling water, leave for about an hour. The solution is then filtered and drunk throughout the day between meals.
Some supporters of treatment with folk remedies are convinced that helminths (worms) further aggravate the course of the disease. To cleanse the body of parasites, it is recommended to take black walnut tincture. The tincture is also believed to effectively cleanse the blood. It should be taken every day before meals, 1 tsp. Many people use the tincture for preventive purposes.
Let us note once again that any self-treatment measures must be coordinated with a doctor. For example, the cause of reactive synovitis of the knee joint may be an allergy. Therefore, in order not to harm your health, you should undergo a medical examination, based on which the doctor will determine the exact causes and prescribe comprehensive effective treatment.
Timely access to a medical facility increases the chances of a speedy recovery and return to your previous life. The main thing is not to start the disease. Modern methods of treating synovitis are quite effective, and the number of relapses is minimal.
By the way, you may also be interested in the following FREE materials:
- Free books: “TOP 7 harmful morning exercises that you should avoid” | “6 Rules for Effective and Safe Stretching”
- Restoration of knee and hip joints with arthrosis - free video recording of the webinar conducted by physical therapy and sports medicine doctor - Alexandra Bonina
- Free lessons on the treatment of lower back pain from a certified physical therapy doctor. This doctor has developed a unique system for restoring all parts of the spine and has already helped more than 2000 clients with various back and neck problems!
- Want to know how to treat a pinched sciatic nerve? Then carefully watch the video at this link.
- 10 essential nutritional components for a healthy spine - in this report you will learn what your daily diet should be so that you and your spine always have a healthy body and spirit. Very useful information!
- Do you have osteochondrosis? Then we recommend studying effective methods of treating lumbar, cervical and thoracic osteochondrosis without drugs.
Synovitis
– inflammation of the synovium with the formation of effusion.
As a rule, the knee joint is affected. Usually the inflammation progresses in one joint. Damage to multiple joints is almost never seen. Synovitis
can form due to infection, injury, allergies, hormonal diseases and metabolic disorders.
It is expressed by malaise, increased joint volume, pain and weakness. When a joint becomes infected, signs of intoxication appear. To be exempt from military service, synovitis must indicate dysfunction of a large joint.
Symptoms
The development of symptoms of synovitis of the knee joint is not affected by the cause of the disease (with the exception of acute infectious synovitis). They are determined by the severity of the disease process and the duration of the course. Therefore, the signs of the disease are considered separately for acute and chronic forms.
Signs of acute synovitis
This form is characterized by the rapid onset and progression of symptoms. First of all, pain appears, which has the following features:
- is not limited to a single point, but extends to the entire joint;
- usually characterized by a fairly intense pain syndrome;
- there is an increase in pain in the morning and a decrease in pain in the evening;
- subsides slightly at rest.
After a short period of time after the onset of pain, swelling may form in the joint area due to increased production of intra-articular fluid. It is impossible to completely bend and straighten the joint, since this action increases the pain. Therefore, active movements of the joint are somewhat limited (by 10-15 degrees).
If a person suffers from acute infectious synovitis, local symptoms may be accompanied by signs of intoxication: loss of appetite, headache, weakness, fever (up to 38 degrees). If the disease is not treated, bacterial synovitis can cause phlegmon of the knee joint
Signs of chronic synovitis
Compared to the acute form, during chronic synovitis, periods of remissions and exacerbations can be distinguished.
The severity of the pain syndrome in the first few years of the disease is identical to the pain in the acute form. However, later the articular cartilage is gradually destroyed, and the walls of the joint capsule become thinner. Consequently:
- pain increases;
- movements of the knee joint are significantly limited;
- the joint is characterized by “instability” - in such patients the incidence of dislocations is much higher than in healthy people.
A febrile symptom is unusual for the chronic form. During exacerbations, the temperature can rise to 37 degrees. With proper treatment, the patient is left with only signs of moderate synovitis, which have almost no effect on his quality of life.
Diagnostics
The presence of synovitis can be suspected based on an analysis of the patient's complaints. To determine the form of the disease, you need to pay attention to its possible causes. To confirm the diagnosis, additional examination is carried out:
- Blood tests:
In a biochemical analysis, it is necessary to look at the level of C-reactive protein. If it exceeds 10 ng/ml, this indicates immune inflammation (rheumatic or psoriatic synovitis);
- In a general blood test, the presence of an inflammatory process is indicated by an increase in ESR and an increase in the number of leukocytes (more than 9.0 * 109).
- Serological analysis may reveal antibodies to streptococcus (antistreptohyaluronidase, ASLO, antistreptokinase) - this is a sign of migratory or rheumatoid synovitis.
After confirming the presence of synovitis and determining its form, you can proceed to the selection of treatment tactics.
Treatment
How should synovitis of the knee joint be treated? Therapy is based on clarifying two main points: the cause of the disease and the mechanism of its development. If the doctor can get rid of the effects of these factors, synovitis will be a thing of the past for the patient. Unfortunately, in the presence of a number of diseases, synovitis cannot be completely cured. These include:
- gout;
- psoriatic and rheumatoid arthritis;
- osteoarthritis and some others.
For each individual form of synovitis, its own treatment regimens have been developed to restore normal functioning of the joint or maintain the patient’s quality of life at an acceptable level.
Acute traumatic synovitis: treatment
The following points can be highlighted in the treatment regimen for this form of synovitis:
- Treatment of injury - in case of an open fracture, the surgeon restores the normal state of the bones located inside the joint; if there is damage, he stitches the damaged areas of the capsule and damaged ligaments, and also sutures the skin over the wound.
- For open and closed intra-articular fractures, the patient is subjected to “skeletal traction” - wires are pulled through the bones that form the joint and a weight is suspended to avoid their re-displacement. Typically, the patient should remain in this condition for up to 3 weeks, unless surgery has been previously scheduled.
- If signs of synovitis appear, the patient is prescribed:
Non-hormonal anti-inflammatory drugs in tablet form or intramuscularly. The most commonly prescribed medications are Nimesulide (Nise), Ibuprofen, Ketorolac (Ketoprofen, Ketorol), Diclofenac.
- To eliminate side effects in the form of stomach and duodenal ulcers, “proton pump inhibitors” are prescribed - Rabeprazole, Omerpazole, etc.
- During the period of “skeletal traction,” the patient is sent to undergo physiotherapeutic procedures (photo- or magnetic therapy), which promote tissue healing. They also produce an anti-inflammatory effect, which reduces the severity of synovitis.
- If there is severe swelling of the knee area, caused by a large accumulation of intra-articular fluid, an operation is performed to remove its excess.
After removing the pins, a cast is applied to the injured leg, which the patient must wear for 6-8 weeks. At this stage, synovitis occurs quite rarely, and it can only be detected when the plaster cast is removed. The disease is treated according to the scheme described above.
Is the use of NSAID ointments recommended? Today there is an opinion that the pharmacological action of ointments is better than intramuscular injections and tablets, since they are specifically applied to the damaged area. However, modern clinical studies have refuted this theory. All NSAIDs are inhibitors of an enzyme that promotes the development of the inflammatory process. They are equally effective regardless of where they are administered. Compared to other forms of medications, ointments are poorly absorbed, so they are not recommended for use at the present time.
With adequate treatment, the symptoms of synovitis disappear after 5-11 days.
Acute infectious synovitis: treatment
This form of the disease is characterized by the fact that, in addition to excess fluid, pus accumulates inside the joint and there are bacteria that gradually destroy the capsule, ligaments and cartilage. Therefore, it is important to puncture the knee joint in a timely manner with the introduction of disinfecting solutions.
How is a knee puncture performed? This operation does not require any preparation from the patient. First, the puncture area is treated with an alcohol solution (70%), and then with an iodine solution. Next, the skin is locally anesthetized with novocaine or lidocaine and a puncture is made. First of all, the internal contents of the joint are pumped out, then they are washed with an antiseptic and pumped out again until the purulent contents are completely removed. Antibacterial therapy measures are similar to those for the acute form of traumatic synovitis. Macrolides or penicillin antibiotics are prescribed. They have better effectiveness and minimal side effects.
The following medications are indicated:
- Macrolides:
Azithromycin.
- Erythromycin.
- Josamycin (recommended for pregnant women and children).
- Ampicillin.
- Amoxicillin.
- Amoxiclav (if the patient has recently finished taking antibiotics or the drugs described above did not have a positive effect).
Physiotherapeutic procedures are contraindicated in infectious processes, because they contribute to an increase in the number of bacteria. Therefore, this treatment method is not used for infectious synovitis.
Treatment of rheumatoid, psoriatic synovitis
The presented forms of synovitis occur against the background of rheumatoid arthritis. To eliminate them, you should treat the underlying disease. For this purpose, complex therapy is prescribed, consisting of the following elements:
- Anti-inflammatory treatment - if there is a positive effect from NSAIDs, you can take only these drugs on a regular basis along with Omeprazole. If taking non-steroidal anti-inflammatory drugs is ineffective, the patient is prescribed hormones (Hydrocortisone, Prednisolone), the dosage of which is determined by the doctor individually.
- Chondroprotective agents are used to preserve the tissues of the knee joint. An effective and inexpensive drug in this group is Chondroitin.
- Reducing the load on the joint - reduces pain. To unload the knee joint, the patient is recommended to walk with a cane.
- Physiotherapy is pain-relieving procedures aimed at the affected area. The use of any techniques is allowed: UHF therapy, photo and magnetic therapy, galvanization.
Treatment should occur under the strict supervision of a rheumatologist. Self-therapy for this form of synovitis is unacceptable.
Tuberculous synovitis: treatment
Tuberculous synovitis is a special form that develops against the background of pulmonary tuberculosis. Its treatment is carried out in combination with therapy of the underlying disease in specialized dispensaries. If you suspect the development of tuberculous synovitis, you should consult a therapist or phthisiatrician.
This disease usually responds well to treatment. After 9 months of adequate therapy, the signs of tuberculous synovitis completely disappear.
Treatment of infectious synovitis developing against the background of osteoarthritis
Synovitis occurring against the background of osteoarthritis requires a special approach to the choice of therapy.
NSAIDs are used as the main treatment. However, to prevent the recurrence of synovitis, it is necessary to improve blood circulation in the affected joint. This goal is easiest to achieve with the help of physiotherapy, which is prescribed from the first days of the disease.
Therapy for migratory synovitis
To cure this form, it is necessary to carry out not only complex therapy for synovitis, but also for rheumatic fever. The following treatment regimen is recommended:
- Prescribed bed rest for 2-4 weeks.
- NSAIDs (Ibuprofen or Ketorolac) - to reduce the severity of inflammation and eliminate pain.
- Benzylpenicillin is an antibiotic that is intended to eliminate the streptococcus that caused the disease.
- Intravenous infusion of drugs with saline solution (droppers with sodium chloride) is intended to eliminate intoxication.
The doctor can expand therapy if necessary. Treatment of migratory synovitis requires hospitalization of the patient for a period of about one calendar month.
Treatment of villous nodular synovitis
This form of synovitis is, by its nature, a benign tumor. The most effective treatment option is removal of the formation. For this purpose, arthroscopic operations are currently performed:
- make two small incisions of 1-2 cm each;
- instruments are inserted into the joint, one of them is a camera with a flashlight, and the second is tweezers or an electric knife;
- they are used to remove the tumor;
- Having completed the removal procedure, the incisions are sutured.
Therapy for gouty synovitis
Synovitis in gout is a common phenomenon that develops due to the deposition of uric acid salts into the joint cavity, which causes inflammation of the synovial membrane and irritation of the capsule. The most effective method of treatment is to follow a diet that requires:
- exclude fish and meat products;
- limit coffee, tea;
- exclude alcohol;
- exclude beets, mushrooms, legumes and greens (lettuce, sorrel, parsley, onions, etc.);
- drink mineral waters (Essentuki, Narzan).
Drug treatment includes:
- NSAIDs during periods of exacerbations, if they are ineffective, take hormones (Hydrocortisone or Prednisolone).
- Colchicine is a drug intended to relieve seizures.
- Constant use of medications that remove uric acid from the body - Allopurinol or Benzbromanone.
If you do not adhere to a special diet in the treatment of gouty synovitis, taking medications will be useless.
Types and classification of the disease
Depending on the course of synovitis, it can be:
• Spicy
– manifested by swelling, pain, hyperthermia and thickening of the synovial membrane.
• Chronic
– fibrous changes form in the joint capsule. Sometimes the villi of the synovial membrane become enlarged, and villous synovitis develops. The resulting “rice bodies” float in the fluid and further injure the synovial membrane. This form of the disease occurs infrequently and is a consequence of incorrect and untimely treatment of acute forms of synovitis or the result of latent, low-grade inflammation in the body. Symptoms of the chronic form are less pronounced.
Taking into account the type of inflammation and the nature of the effusion, the disease is divided into serous, hemorrhagic, purulent
and
serous-fibrinous
.
Taking into account the cause of the development of synovitis, infectious, aseptic
and
allergic
form of the disease.
Types of synovitis
1. Pigmented villonodular
(PVS) - manifested by the proliferation of synovium, hemosiderin staining, the formation of villi, nodular masses and pannus. This is a fairly rare pathology and occurs at a young age. The disease develops over a long period, increasing swelling and pain, which are usually associated with injury. During an exacerbation, there is effusion, a local increase in temperature, limited mobility and a change in the shape of the joint. On an x-ray, the changes are almost invisible, sometimes disturbances in the form of surface erosions are noted.
2. Reactive
- restriction in the functioning of the joint is a consequence of the inflammatory process taking place in its cavity. In this case, fluid accumulates in the synovial membrane, a “dull” pain develops when walking, the joint is increased in volume, its shape is changed, and movements are limited. Usually the right or left knee joint is affected. This type of disease is secondary in nature against the background of the underlying pathology. Consequently, the main therapy is associated with the elimination of the underlying disease, and treatment of synovitis itself consists of joint puncture with the administration of antibiotics and corticosteroids, immobilization, NSAIDs and physiotherapy.
3. Post-traumatic
- this form of the disease occurs most often and is the body’s reaction to intra-articular damage. They develop as a result of injury (chondropathy, rupture of the cruciate ligaments or meniscus). Sometimes this type of disease is mistaken for infectious arthritis or hemarthrosis. In acute cases, deformation of the joint occurs, severe pain, and stiffness in the joint are noted. The chronic form is manifested by aching pain, protrusion of the patella, fatigue and dropsy of the joint. This provokes the formation of dislocations, sprains and complete immobilization.
4. Moderate
- any inflammatory diseases of the joint, for example, arthrosis, can develop into moderate synovitis with clear characteristic symptoms.
5. Minimum
- the reasons are the same as for moderate synovitis; the use of a pressure bandage is sufficient for treatment.
6. Suprapatellar
- Fluid accumulation and inflammation of the synovial membrane occur above the patella.
7. Exudative
- develops without visible injuries, that is, it is primary synovitis. It is usually caused by irritation of the inner surface of the joint capsule as a result of meniscus tear, cartilage injury, or joint instability.
8. Recurrent
— accompanied, as a rule, by a chronic form of hydrarthrosis with the formation of synovial membrane hypotrophy and fibrosis. Dropsy complicates the course of the disease and causes degenerative disorders.
9. Villous
- the villi of the inner lining of the joint grow, fibrinous formations appear, leading to severe disorders of lymphatic drainage and blood circulation in the joint area.
10. Secondary
- the appearance of this form is caused by the accumulation of products of destruction of cartilage tissue in the joint. The resulting antigens are perceived as foreign material, which leads to chronic inflammation. The course of the disease is similar to chronic arthritis.
11. Transitory
- usually the pathology affects children aged 1.5 - 15 years. The disease develops acutely. Pain appears in the morning, movements in the joint are limited, and its location is changed. X-rays show widening of the joint space. The duration of the illness is 14 days. Doctors suggest that a child may develop this form of synovitis after suffering from pharyngitis or tonsillitis, prolonged walking or injury. If the disease is not treated promptly, lameness may develop.
Read also: Diseases of the knee joints
12. Exudative-proliferative
– develops as a result of injury and is associated with the production of a large volume of exudate (turbid, protein-rich fluid containing joint and blood breakdown cells). This form of the disease usually affects the hip joint.
There are 4 degrees of proliferative form of pathology:
1. Thickening of the synovium without significant proliferation of villous tissue; 2. Formation of focal accumulations of villi caused by thickening of the synovium; 3. The lateral sections of the joint are completely covered with villi; 4. Villi cover all parts of the joint.
According to localization, synovitis is classified:
• ankle joint; • temporomandibular joint; • knee and hip joint; • hand (wrist) and elbow joint; • shoulder joint; • big toe and foot.
Types and forms of the disease ↑
There are quite a large number of forms of the disease. Here are the most common ones.
Reactive
This is a subtype of allergic synovitis, which occurs as a result of:
- frequent mechanical irritation of the synovial membrane (for example, when the joint bones or articular surfaces are damaged by disease);
- as a response to general intoxication resulting from infectious or non-infectious pathology.
Chronic
In this case, the division of synovitis according to the duration of its course is taken into account.
The disease develops as a result of untreated or undertreated acute synovitis, especially if it was caused by a traumatic factor that was not subsequently eliminated. The general reactivity of the synovial membrane also plays a role in the development of the disease.
It is difficult to diagnose this disease at first due to the paucity of its clinical manifestations.
But its advanced course leads to disruption of blood and lymph circulation in the joint, which leads to a change in its function and a deterioration in the quality of life.
Moderate
This takes into account the classification according to the severity of inflammatory changes in the synovium.
Symptoms of the disease are not very pronounced:
- the joint does not increase in volume much;
- movements in it, although painful, are possible;
- the general condition suffers, but only slightly.
Photo: synovitis of the knee joint
This type of disease must be treated especially carefully, as it has a tendency to recur and become chronic.
Post-traumatic
This is synovitis that develops as a result of mechanical trauma to the synovial membrane.
Trauma can be either an external impact on the joint or (most often) irritation of the membrane by fragments of bones and cartilage located inside the joint, in case of damage to the meniscus.
Minimum
The diagnosis of “minimal synovitis” is made according to magnetic resonance imaging.
It is characterized by few clinical manifestations, which makes it difficult to diagnose.
May occur due to any of the reasons described above.
Vypotnoy
The synovial membrane, covering the joint cavity from the inside, is the place in which normal articular (called synovial) fluid is synthesized, feeding the articular cartilage.
When this membrane is inflamed or irritated, the cells react by synthesizing more fluid - an effusion appears in the joint (there can be a different amount of it).
Fig.: synovitis of the knee joint
Effusion synovitis is usually a variant of an acute disease, since during a chronically ongoing process, cells are depleted, resulting in less synovial fluid than necessary.
Secondary
It occurs in response to some other disease that can develop both inside the joint (osteomyelitis, arthritis) and in any other organ.
Treatment of such synovitis will not be effective until the primary source of inflammation is eliminated.
Purulent
It develops as a result of bacterial flora entering the synovial cavity.
This can occur either as a result of injury or due to another infectious disease (gonorrhea, tuberculosis, pneumonia, sepsis).
This is the most difficult process.
It requires the use of antibacterial therapy:
- initially - a wide spectrum, after diagnosis and taking pus for bacteriological examination;
- continues - based on the results tank. sowing and sensitivity of the microorganism to a certain type of antibiotic.
Spicy
This is one that developed for the first time, in response to any mechanical, infectious, inflammatory, allergic disease.
Photo: acute synovitis of the knee joint in the picture
Acute synovitis develops quite rapidly and requires research to determine its type.
Villous
One of the subtypes of chronic synovitis.
The diagnosis is made based on the results of arthroscopy (introduction of video equipment into the joint).
Photo: villous nodular synovitis
In this case, you can note:
- thickening of the outer shell of the joint capsule;
- cicatricial changes appear in it;
- The villi of the synovial membrane also grow;
- fibrin is deposited on the synovial membrane, which hangs, like cysts, into the joint cavity.
Recurrent
It develops mainly with untreated acute synovitis.
If such a disease recurs frequently, then:
- fluid accumulates in the joint (hydrarthrosis, dropsy);
- as a result, the pressure on the synovial membrane increases;
- as a result, the membrane becomes thinner, cicatricial changes appear in it, and its ability to absorb joint fluid sharply decreases.
A “vicious circle” arises.
Suprapatellar
This is the name for inflammation of the synovial membrane in the area above the patella bone.
In this case, different amounts of effusion accumulate in the so-called suprapatellar bursa - a special “volvulus” of the synovial membrane.
Double sided
It develops mainly during a chronic process in the synovial membrane, as well as during allergic (autoimmune) damage to the cells of this membrane by various antibodies.
Read also…. How to cure foot tendinitis?
Exudative
Most often occurs in response to mechanical trauma to the joint.
At the same time, the synovial membrane produces quite a lot of inflammatory fluid (exudate), rich in proteins and various cells.
Based on the nature of this liquid, they are distinguished:
- serous synovitis;
- serous-fibrinous (also called adhesive);
- purulent synovitis;
- hemorrhagic.
Expressed
This characterizes the severity of inflammatory changes in the joint according to additional studies: MRI, ultrasound, arthroscopy.
In this case, the symptoms are usually pronounced:
- the joint is swollen;
- the skin over it is stretched;
- the skin may be red;
- movements are significantly difficult.
Hypertrophic
This is a type of chronic synovitis.
This diagnosis is made according to the morphological study of the synovial membrane.>
In this case, as a result of prolonged irritation of the synovial membrane, a pronounced growth (hypertrophy) of its villi is noted.
Transitory
Most often occurs in children 1.5-15 years old.
It is characterized by rapid development of symptoms and resolves within two weeks.
If the disease is not treated on time, the child will limp.
Probable reasons:
- bacterial diseases of the respiratory tract and oral cavity (sore throats, pharyngitis);
- in case of joint injury;
- when walking for a long time.
Symptoms and signs
Synovitis typically affects one joint; very rarely, the pathology is multiple.
General symptoms:
• limitation of movement in the joint and pain during exercise; • swelling and change in the outline of the joint; • malaise, general weakness; • hyperthermia of the skin in the affected area, hot to the touch.
All signs of the disease can be more or less pronounced depending on the form of the pathology and the individual characteristics of the patient. Infectious synovitis is manifested by a rapid increase in symptoms, with hyperthermia over 38°, the formation of pain and a feeling of pressure in the joint. In just a few hours, manifestations of intoxication develop (restlessness, headache, pallor) and the joint swells.
With non-infectious synovitis, the symptoms increase slowly, first of all there is discomfort in the joint and aching pain during exercise. After a few days or weeks, the pain increases, swelling appears, and the joint becomes deformed. Sometimes the signs of the disease disappear on their own, usually in the absence of stress, and independent recovery is possible.
Clinical picture
The symptoms of the disease largely depend on the causative factors. But there are several signs of synovitis that will be observed in any of its forms:
- Pain in the area of the affected joint;
- Edema and swelling in the joint area;
- Impaired motor function.
Read also: Blood test for rheumatic factor
These symptoms can vary in intensity - minimal, moderate, intense.
Such symptoms are not the main ones for diagnosing synovitis, as they can be observed with other joint pathologies. Based on them, we can only assume the likelihood of inflammation of the synovial bursa.
Based on the nature of the course, two forms of the disease are distinguished:
- Acute synovitis. It is observed in most cases and has a pronounced clinical picture. Usually caused by exposure to external factors. The clinic clearly shows a change in the stages of inflammation. The disease resolves within 3 weeks;
- Chronic synovitis. This form is given if the inflammatory process lasts more than a month. Usually one joint is affected, and there are mild symptoms. The pathological process has a wave-like course.
Exudative synovitis is an inflammatory process in which intensive production of synovial fluid is observed. As a result, the joint increases significantly in size and takes on a spherical shape. Exudative synovitis is most often purulent.
Let's consider several clinical forms of the disease:
- Pigmented villonodular synovitis. This pathology is typical for young people. It is characterized by the formation of villi and growths on the inner surface of the capsule. The disease develops slowly, there is a gradual progression of pain, swelling, and dysfunction of the limb;
- Reactive. Develops against the background of activation of chronic foci of infection. Characterized by moderate swelling, low-intensity pain, limited range of motion;
- Post-traumatic. Accompanied by joint deformation and often becomes chronic. Develops several weeks after injury;
- Purulent. Characterized by a pronounced clinical picture, increased local and general temperature, malaise, severe bursting pain;
- Autoimmune. Usually it immediately becomes chronic. It manifests itself with moderate symptoms, pain comes first.
Most often, moderate synovitis with mild symptoms is observed.
Complications
With synovitis, complications may develop:
• Purulent arthritis - appears when the purulent process spreads to the fibrous membrane of the joint capsule. • Gonarthrosis or arthrosis deformans - the hyaline cartilage covering the bony condyles is affected. This type of arthrosis is the most common and develops over several years. • Panarthritis – is formed when the cartilage, bones and ligaments of the joint are involved in the purulent process. • Restriction of movement or complete immobility as a result of irreversible changes in the joint. • Soft tissue phlegmon and periarthritis – are formed when the purulent process spreads to the surrounding tissues of the joint. • Sepsis (infection in the blood) develops in the absence of treatment or weakened immunity. • Hydrarthrosis (dropsy) – accumulation of excess fluid in the joint. • Joint looseness and weakening of ligaments leading to subluxations or dislocations. • Baker's cyst - accompanied by circulatory disorders, thrombus formation, with tingling, tissue numbness and convulsions. This may ultimately contribute to limb loss.
Traumatic and post-traumatic synovitis
One of the most common causes of synovitis is trauma. Therefore, athletes are more likely to suffer from the disease.
- The injured joint swells and becomes painful.
- The patient feels weakness and loss of strength.
- He may feel dizzy and have a fever.
- The inflamed joint loses mobility.
If an infection is added to the inflammatory process, a purulent form of the disease may develop. Pyogenic bacteria cause more severe intoxication of the body. The skin in the joint area turns red and becomes hot. Body temperature may rise to 39°C or higher. If such signs appear, you should immediately consult a doctor.
As a result of infection, the patient's nearby lymph nodes sometimes increase in size and become painful. When the inflammatory process spreads to cartilage, ligaments and bones, purulent arthritis (panarthritis) develops. A dangerous infection can penetrate nearby organs and into the blood.
Post-traumatic synovitis develops as a result of destruction of joint tissue caused by injury. However, there may not be any signs of injury on the outside. Damage to the articular membrane occurs due to the mechanical pressure of the articular elements on it during a fall or impact. The disease appears some time after the injury. Its diagnosis is difficult because the patient does not always notice the injury. It is important for the doctor who treats the patient to distinguish the disease from rheumatoid arthritis.
The joint increases in size and loses its anatomical shape over several hours or days. During this period, the amplitude of his movements decreases and severe pain appears. It sharply intensifies when trying to move the affected joint. The patient's body temperature rises and there is a loss of strength.
Causes of the disease
1. Infectious synovitis
. Develops due to the penetration of pathogenic microbes into the joint. The causative agent of the disease enters the synovial membrane from neighboring tissues, distant foci of infection and from the outside. The nonspecific form of the pathology is provoked by streptococci, pneumococci, etc. And the specific form is caused by Koch’s bacillus, treponema pallidum, etc.
2. Allergic synovitis
. The reason for the formation of this type is the patient’s contact with the allergen, subject to increased sensitivity to it.
3. Aseptic synovitis
. There is no infectious pathogen, and the source of origin is:
• metabolic disorders; • mechanical trauma (bruises, intra-articular fractures, meniscus damage, ligament ruptures, etc.); • hormonal disorders; • irritation of the synovium due to meniscus tear or cartilage damage; • hemophilia.
Causes of synovitis
The causes of the disease are divided into two groups:
- Infectious - they are caused by pathogenic microorganisms that penetrate the synovial membrane as a result of injuries that violate the integrity of the skin, or through blood and lymph from foci of infection inside the body.
- Non-infectious (aseptic) - this group includes synovitis caused by injuries, endocrine disorders, and allergic diseases.
Synovitis often occurs against the background of bursitis - inflammation of the synovial bursa.
Diagnostics
The diagnosis is made based on symptoms, results of a diagnostic puncture and other studies. At the same time, it is necessary not only to confirm the existence of synovitis, but also to determine the cause of its development, which is often quite difficult. In the aseptic form of the disease, the doctor prescribes arthropneumography or arthroscopy. Sometimes cytological examination and biopsy of the synovium may be necessary. If there is a possibility of allergen penetration, allergy tests are performed. If hormonal, metabolic disorders or hemophilia are suspected, consultation with appropriate specialists is necessary.
A diagnosis of punctate, the fluid taken during joint puncture, is required. Acute aseptic synovitis is manifested by a large volume of protein and a decrease in the viscosity of the effusion, while chronic synovitis reveals excessive enzyme activity, leading to rapid destruction of cartilage.
In the puncture of infectious synovitis, pus is detected, which is diagnosed by bacterioscopic or bacteriological methods. This allows you not only to determine the type of pathogenic microorganisms that caused inflammation, but also to select effective antibacterial drugs. A general blood test reveals leukocytosis, increased ESR and the number of band neutrophils.
The main principles of treatment are puncture, immobilization, and, if necessary, surgery or drainage. Patients with a purulent form of the disease are hospitalized in the surgical department, with a traumatic form - in the traumatology department, and the rest - in departments corresponding to the profile of the primary pathology.
Treatment of any type of synovitis begins with joint puncture. Using a needle penetrating the joint cavity, fluid is collected for diagnostic studies, and then antibiotics are administered for prophylaxis. The manipulation is practically painless and is performed without anesthesia.
For any type of disease, immobilization is indicated, that is, immobilization of the joint using a knee brace or bandage; they must be worn for at least a week. Elevation of the limb is also sometimes recommended.
Doctors prescribe NSAIDs (diclofenac, voltaren, ibuprofen, indomethacin) in the form of ointments, injections or oral medications to almost all patients with this diagnosis. It is also possible to administer intra-articular corticosteroids in combination with physiotherapy (magnetic therapy, ultraviolet irradiation, ozokerite, UHF, paraffin, phonophoresis).
Surgical intervention consists of excision of the synovial membrane; it is performed for chronic synovitis with irreparable changes in the joint or for constantly recurrent forms of the disease. In the postoperative period, immobilization, antibacterial and anti-inflammatory drugs, and physical therapy are also indicated.
Diagnostic methods ↑
Synovitis of the knee joint is a diagnosis that is not made only on the basis of anamnesis, complaints and the results of examination of the joint, but requires instrumental confirmation.
This happens because many of the symptoms (pain and impaired movement), as well as objective data (swelling of the joint, redness and swelling of the skin over it) are nonspecific, that is, they can appear in various diseases.
Therefore, when making a diagnosis, the doctor is guided by the data of some instrumental diagnostic methods.
Ultrasound
This study is very informative in identifying effusion in the joint cavity.
So, if the amount of exudate exceeds 1 ml, it will already be visible.
Also, with this diagnosis, thickening of the joint capsule is visualized.
Video: signs on ultrasound
MRI
This type of diagnosis is widely used to visualize intra-articular structures.
It is based on his data that the diagnosis of “Synovitis” is made.
In the case of the development of this disease, a change in signal intensity in the joint cavity is noted due to the accumulation of exudate: it is hyperintense in T2WI mode, reduced - in T1WI.
With MRI with contrast, the signal from the inflamed synovial membrane is enhanced, its growths are visible, which hang into the lumen of the articular capsule.