Home » Our health » How to treat bursitis of the shoulder joint - symptoms and causes
Our health
Robert Prokofiev 12/05/2016
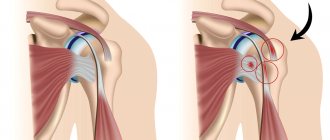
Shoulder bursitis is an inflammation of one of the periarticular bursae.
In its normal state, the bursa is a small cavity lined with a synovial membrane that produces a special fluid to withstand frictional forces. During inflammation, the volume of fluid produced increases sharply.
In the area of the shoulder joint there are about ten bursae: the subcoracoid, subacromial, subdeltoid (double), bursa of the subscapularis muscle, two bursa of the latissimus dorsi muscle, bursa of the pectoral muscle, as well as the bursa at the top of the acromial process and between the two legs of the scapular ligament. The process is often localized in the subdeltoid and subacromial bursae (subdeltoid and subacromial bursitis of the shoulder joint).
In some cases, the bursa - the bursa - communicates with the articular cavity. For example, if the subacromial, subdeltoid and subcoracoid bursae are affected, infection may penetrate into the cavity of the shoulder joint.
The risk group is males aged 35 to 45 years, whose occupation is associated with intense loads on the shoulder joint (athletes, loaders, miners, etc.).
Etiology
Bursitis of the shoulder joint is a fairly common disease that can begin to progress due to many reasons, including:
- excessive physical stress on the shoulders;
- injuries, bruises, sprains, cuts or abrasions;
- allergic reactions;
- metabolic disease;
- prolonged tension in a certain joint in the shoulder;
- autoimmune lesion;
- intoxication of the body;
- the effect of alcoholic beverages or tobacco smoke on the body;
- arthritis.
Violation of the structure of the shoulder joint can be caused by either one reason or a combination of them.
Causes
The shoulder joint includes about a dozen periarticular bursae in the form of the subcoracoid, subacromial, double subdeltoid, bursa of the subscapularis muscle, two bursa located at the dorsal muscle, bursa of the pectoral muscles, etc.
Inflammation most often affects the subdeltoid and subacromial bursae. The reasons for the development of the inflammatory process are the following situations:
- Intense physical activity caused by professional sports or the nature of work.
- Injury to the shoulder joint or sprain.
- Arthritis caused by infection, injury, or various autoimmune disorders. The causative agent of infection can penetrate through minor injuries in the form of an abrasion or small wound and spread through the blood or lymph flow. Often the infection joins the existing antiseptic inflammation in the bursa.
- Metabolic disorders resulting from diseases such as diabetes and gout.
- Allergy.
- Decreased immunity from intoxication due to abuse of alcoholic beverages and tobacco.
Varieties
Depending on how the disease progresses, bursitis can be:
- sharp;
- subacute;
- chronic;
- infectious.
Based on the composition of the fluid, the disease is:
- purulent;
- fibrous;
- serous;
- with blood impurities.
In addition, in the medical field, there are other types of shoulder bursitis, which have similar causes, but differ in course:
- calcareous bursitis of the shoulder joint, which is also called stone bursitis - accumulations of calcium salts are transformed into lime;
- calculous - calcium deposits are localized so deeply that surgical intervention is used to restore the functionality of the shoulder;
- subacrominal - which is characterized by acute pain when the joints are tense, and when the arm is lowered down, hanging freely, all unpleasant sensations go away;
- tendobursitis – combines the inflammatory process with thinning of the tendon structure.
What is arthrosis of the shoulder joint
Arthrosis, osteoarthrosis, deforming osteoarthritis (DOA) – these are all names for one disease. In Latin, “arthritis” is a derivative of the name of the joint, “osteo” is bone, the suffix “oz” indicates a pathological change in tissue. With arthrosis, degenerative changes affect cartilage, bone, and other joint tissues.
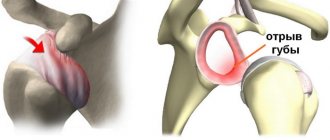
The structure of the shoulder joint includes the spherical end part of the humerus and the articular cavity of the scapula, covered with a thin layer of cartilaginous tissue, as well as the articular capsule covering them on all sides. The inner layer of the joint capsule is formed by a sealed synovial membrane filled with synovial fluid. This substance is similar in composition to hyaluronic acid. It serves to lubricate the joint and nourishes the cartilage with all the substances necessary for their regeneration.
Arthrosis of the shoulder joint begins with changes in the composition of the synovial fluid, which can be the result of various reasons. Due to lack of nutrition, degenerative changes begin in the cartilage tissue, it becomes softer, more susceptible to defects, and wears out and thins out faster. Over time, the bone tissue located under the layer of cartilage becomes exposed and deformed, and marginal growths form on it - osteophytes, which serve as limiters of joint movement and can completely block it.
Timely treatment can counteract the pathological process, improve tissue regeneration and maximize the service life of the joint.
Symptoms
Bursitis of the shoulder joint
In addition to the main symptom of shoulder bursitis - pain of varying intensity, the disease has the following symptoms:
- swelling and tingling sensation in the affected area;
- redness of the skin at the site of inflammation;
- slight increase in body temperature;
- weakening and rapid fatigue of the hand.
Such signs are characteristic of the acute form and stone type of the disease. With the chronic course of the pathological process, these symptoms intensify slightly and appear in waves - periods of increased pain alternate with periods of their subsidence.
Tendobursitis is characterized by symptoms such as dull pain with a specific location, which the patient can easily point to, and a decrease in motor functions. Externally, no changes in the shoulder are observed. This form of bursitis can only be detected on an x-ray.
Subacrominal bursitis is accompanied by symptoms such as:
- severe pain that appears not only when moving, but also at rest;
- weakness in the hand;
- touching the affected area causes discomfort;
- The fluid in the shoulder bursa contains pus and blood.
What is arthrosis of the shoulder joint
Dystrophic changes in the cartilage and adjacent bone tissue of the shoulder joint are defined in medicine as arthrosis of the shoulder joint by ICD 10-M19.91. Most often, arthrosis occurs in the acromioclavicular joint of the shoulder, which most often experiences constant stress and severe stress during the day.
- Under the influence of injuries and various inflammatory processes, cartilage tissue is damaged and gradually weakens, becoming fragile and thin.
- Cracks form in the cartilage, in which salts begin to be deposited, accelerating the destructive processes in the cartilage tissues.
- As a result of such salt deposits, the bone tissue becomes dense and begins to deform (see photo), and acromioclavicular arthrosis develops.
Arthrosis of the shoulder joint is degenerative changes in the cartilage and adjacent bone tissue of the shoulder joint
This process occurs slowly and is chronic; at the beginning it is asymptomatic, but gradually the manifestations of the disease increase and over time can lead to complete immobility in the joint area.
The following factors can trigger the onset of the pathological process:
- Shoulder injuries that have caused the joint to become deformed and cause inflammation.
- Insufficient blood supply to the shoulder joint, which lasts for a long time - this condition can be caused by vascular disorders.
- Constant high loads on the joints are observed among construction workers, athletes, and loaders.
- Congenital joint pathologies.
- Poor nutrition and, as a result, metabolic disorders.
Important! The most common form of the disease is post-traumatic arthrosis of the shoulder joint, ICD code 10-M19.91.
The shoulder joint is one of the most mobile in humans, which provokes quite frequent injuries to the joint. Even a small injury to a joint that is repeated regularly and over a long period of time leads to the development of arthrosis. Arthrosis of the right shoulder joint is most common, because the majority of the population are “right-handed” and the load on the right side is always higher.
Why does shoulder arthrosis develop?
The impetus for the development of shoulder arthrosis is inflammation in the joint. It can appear for various reasons:
- Injuries . Shoulder arthrosis can develop due to a previous shoulder injury, or constant, minor microtrauma to the shoulder, typical of athletes.
- Vascular diseases. With vascular pathologies, blood circulation is usually impaired, which leads to insufficient blood supply to the joints. As a result, articular tissues undergo degenerative changes, i.e. arthrosis develops.
- Excessive load. This is often associated with the patients’ work activities (loaders, builders).
- Hormonal or autoimmune disruptions . Often they significantly affect joint tissues, having a destructive effect on them. These are diseases such as psoriasis, gout, etc.
- Heredity . It has been proven that children of parents with arthrosis of the shoulder joint are more prone to developing joint defects than others. This also includes people who were already born with any joint defects. Both of them perceive the usual load placed on their hands as excessive, and therefore the process of wear of the cartilage occurs much faster.
- Failures in metabolic processes and the endocrine system . Because of this, salts begin to accumulate in the joints, and cartilage tissues cease to receive proper nutrition (phosphorus, calcium, etc.) and begin to deteriorate.
- Joint diseases. A prerequisite for the development of arthrosis can be joint pathologies such as arthritis, bone necrosis, synovitis, etc.
- Age. Elderly people (50 and older) are especially at risk, since joint tissues wear out with age, which in itself leads to the development of pathology.
If the disease develops, you need to consult a doctor, undergo diagnostics, and only then proceed to conservative treatment for medical reasons. It is necessary to find out why the joint was able to deform, what preceded this pathological process. The main causes of arthrosis of the shoulder joint are detailed below:
- vascular diseases with impaired systemic circulation;
- prolonged physical stress on the shoulder joint;
- genetic predisposition;
- impaired metabolism;
- chronic diseases of the endocrine system;
- injuries;
- extensive joint diseases;
- age-related changes in cartilage and bone tissue;
- autoimmune diseases.
sovets.net
Signs
Arthrosis is characterized by a long development, sometimes not manifesting itself in any way in the initial stages. Therefore, you should be very wary of the slightest symptomatic manifestations. Shoulder arthrosis is usually indicated by:
- Pain is considered the main symptom of the disease. Aching pain often bothers patients in the morning. Pain syndromes are also more possible with sudden changes in weather. If you subject your sore shoulder to any load, for example, lifting something heavy, then the pain will also remind you of itself. The patient feels pain even when feeling the shoulder. With the development of shoulder arthrosis, pain begins to occur even in a quiet position. This fact should be taken into account - with arthrosis of the shoulder joint, pain can occur not only in the affected joint, it can be localized in the arm, elbow or back.
- Motor dysfunction. Because of the pain, it becomes difficult for the patient to cope with seemingly simple tasks on his own, for example, combing his hair. By the way, this action is one of the test movements for diagnosing arthrosis. Rotational movements and attempts to move the arm back are also difficult. If treatment is not started on time, then gradually the shoulder joint and, accordingly, the arm stop moving altogether, and contracture develops.
- Painful crunch, creaking in the joint. It usually occurs due to salts deposited in the diseased joint (osteophytes). Initially, a weak, creaking rustle appears in the diseased joint; as the disease progresses, it turns into distinct crunchy clicks, audible even at some distance from the patient.
- Swelling, increased general temperature and redness at the site of the affected joint. These signs confirm the presence of inflammation in the diseased joint.
- Hardening of the joint. This symptom appears when the disease is advanced due to bone growths that cover the joint.
Diagnostics
Diagnosing bursitis of the shoulder joint is not difficult for an experienced doctor. The diagnostic process consists of a whole range of activities:
- examining the affected area for redness and swelling;
- collecting information about the causes and timing of symptoms;
- Carrying out radiography - from the image you can determine the form of the inflammatory process;
- puncture of the affected joint capsule, thanks to which you can find out the composition of the fluid, the presence of purulent or blood impurities;
- use of ultrasound and MRI data of the affected shoulder joint.
Which doctor should I contact?
If disturbing symptoms appear in the form of shoulder pain or limited mobility of its joint, it is recommended to visit a rheumatologist or orthopedist, since these specialists will be able to help with the initial stage of the disease. When time has passed and the disease has advanced, only a surgeon can help. Upon contact, specialists prescribe the necessary tests in the form of x-rays, ultrasound, and laboratory tests. Based on the results obtained, the doctor makes the necessary prescriptions.
Treatment
Treatment of bursitis of the shoulder joint is carried out using many methods, from therapy with folk remedies to surgery.
Not all types of bursitis are treated with surgery, but only a few:
- stone, because deposits of calcium salts acquire the structure of lime or stone, which cannot be cured with medications;
- calculous - since calcium collects much deeper than in other forms, and the functioning of the shoulder can be normalized only by removing the salts surgically;
- tendobursitis - it is possible to cure and restore the functionality of the arm only through surgery, during which calcium deposits are removed and the joint is artificially strengthened;
- purulent - the operation is aimed at removing purulent fluid (sometimes mixed with blood) from the shoulder joint bursa.
In addition to this drastic remedy, bursitis can be treated by rubbing medicinal ointments and taking anti-inflammatory and antibacterial medications. Also, therapeutic massages and physical exercises are used to strengthen and restore motor functions. All the time, until complete recovery, the patient needs to wear a tight bandage or bandage on the damaged shoulder (grabbing the elbow), so that after the operation the tissue fusion takes place in the correct form.
Bandage for shoulder bursitis
Treatment of bursitis of the shoulder joint can be carried out at home using folk remedies, the effect of which will be noticeable only if they are used in conjunction with other methods.
So, folk remedies consist of medicinal compresses, which are made from:
- cabbage leaves;
- Kalanchoe;
- burdock leaves;
- salt - for this, salt is soaked in boiling water, a scarf or towel is dipped into the resulting solution, and the sore spot is tied.
Also, treatment with folk remedies consists of preparing decoctions, which include burdock root, propolis and butter.
You can use warming up using flax seeds, which are heated, then while still hot they are transferred to a towel, tied so as not to spill the seeds, and applied to the sore spot.
The latest folk remedy for treating bursitis is medicinal pine baths, which must be taken daily until the disease completely subsides. The duration of the bath is no more than twenty minutes.
Clinical picture
Doctors also call calcareous bursitis calculous or stone. This lesion of the musculoskeletal system is considered quite severe. Inflammation in the area of the synovial bursa is accompanied by calcareous deposits. They accumulate in the form of calcium balls.
Calculous bursitis causes the joint to cease to function normally. There is a complete disruption of the mobility of the joint. The pathology is dangerous due to the complete immobilization of the joint and its destruction.
Calculous bursitis can affect any joint. Most often, inflammation with calcification is localized in the shoulder area.
Also, this type of pathology can affect any joint:
- knee;
- shoulder;
- elbow;
- hip
In ICD-10, bursitis is coded M70. It includes a group of pathologies called “soft tissue diseases associated with pressure and load. overload."
Clinical picture of stone bursitis
Prevention
Preventive measures aimed at avoiding the occurrence of such inflammation consist of:
- reduction in physical activity (directed at the shoulder joints);
- maintaining a healthy lifestyle and giving up bad habits;
- good rest;
- performing gymnastic exercises in between hard work;
- a balanced diet, which should be enriched with vitamins and calcium;
- timely diagnosis and treatment of any infectious diseases.
Forecast
Calcium deposits may not cause any discomfort. If pain occurs, you will need the help of specialists. If inflammation can be relieved with this pathology, the prognosis for the patient will be favorable.
Physiotherapy in combination with drug treatment is considered especially effective. In some cases, surgery is required to remove calcium deposits. The pathology in question is treatable if you follow all the recommendations of the attending physician.
Self-medication is dangerous due to the development of complications. The leading complication of calculous bursitis in the absence of proper treatment is the absolute destruction of the bursa, cartilage, and bone elements. There are still chances for a full recovery even after surgery. Complex cases require longer treatment, so do not delay starting therapy.
What causes bursitis, watch in our video: