From school life safety lessons, everyone knows that according to the nature of severity, there are 4 degrees of burns.
A burn is damage to a person’s soft tissue as a result of exposure to high temperatures or chemical exposure. Each degree is characterized by its depth of affected tissue, from which specific measures are taken to restore health.
Doctors also pay great attention to the causes of injury. But in any case, if a burn occurs, first aid should be provided to the victim without waiting for the ambulance team to arrive.
What is a second degree burn and how long does it take to heal?
Second degree burns are superficial injuries , but nevertheless require close attention.
Unlike the first degree, which affects only the epidermis, in this case there is deeper damage to the skin, where in addition to the epidermal layer, the upper layer of the dermis is injured and microcirculation is disrupted.
Typically, 2nd degree burns heal relatively quickly - up to two weeks, and their treatment for a small area of damage is possible at home.
If the affected area is more than 1% (“palm of the hand”), you should immediately seek help from a doctor.
This is explained by the body’s possible reaction to the injury in the form of a burn or shock, which are grounds for mandatory hospitalization. Infection in the wound and dehydration may occur. Particular attention is paid to children and elderly patients.
Classification of burn herbs in Russia
On the territory of the Russian Federation, its own classification of gradation of burn injuries is used. The severity of the pathology is determined by the nature of the damage to the skin surface, as well as the blood flow system. When the circulatory system is damaged, regeneration processes are completely inhibited. In such a case, even a surgical operation does not guarantee the absence of burn marks.
The most common cases of injury are burns of the upper and lower extremities
Let's find out what degrees of burns there are and how they are expressed. Let's describe all the steps in more detail:
- The first degree is a shallow lesion of the skin, accompanied by erythema, swelling and attacks of aching pain.
- Second degree - small blisters containing clear or yellow liquid form on reddened areas of the skin. If individual elements of the vascular system are damaged, this liquid may be colored burgundy. Since this type of injury does not affect the germ layer, regenerative processes in cells completely restore damaged tissue.
- Third degree - with this degree of injury severity, the lesion affects the germinal layer of the epidermis. Tissue destruction leads to the formation of necrosis.
- Fourth degree is one of the most difficult types of burns. These injuries destroy tissue, muscle and even bone. In addition, this type of burn injury most often affects large areas of the human body.
A similar classification is used not only in Russia, but also in many other countries. It is this gradation that is considered the most convenient for selecting treatment methods.
Many people are interested in how to determine the degree of burn at home. The nature, severity, and possible consequences of the injury can only be determined after twenty-four hours. It is during this time that a kind of border appears, separating the dead areas from healthy tissue. Despite this nuance, first aid measures should be taken in the very first minutes after exposure of the skin to various aggressive factors.
First degree burn injuries to the skin
This category of injuries affects only the upper layer of the epidermis. The correct approach to therapy can reduce the risk of scar formation and complications of the recovery process to a minimum. Factors leading to such damage include contact with hot metal, faulty wiring, and short-term exposure to ultraviolet rays on exposed skin.
The main danger of this type of pathology is the risk of poisoning from toxins resulting from tissue destruction and dehydration. The main symptoms characteristic of such injuries are itching, erythema and peeling.
Regeneration processes in damaged tissues take several days. During the last stage of tissue repair, small scales and hyperpigmentation form on the affected area of the body.
If the depth of tissue damage is great and the burn is very extensive, then this can pose a great danger to the life of the victim
Second degree burn injuries to the skin
These types of damage to the integrity of the skin lead to the formation of small blisters filled with serous secretions on the affected areas of the body. The formation of blisters begins approximately on the second day after injury, which significantly complicates the early diagnosis of the nature of the pathology. Among the various factors leading to such injuries, the following should be highlighted:
- exposure to chemical components on the skin;
- exposure to high electrical voltage;
- prolonged stay in rooms with temperatures exceeding seventy degrees Celsius;
- interaction with open fire or steam.
The second degree of thermal burn is much more difficult to treat compared to the others. The duration of tissue restoration for this type of burn is about three weeks.
Third degree burn injuries to the skin
This type of burn is divided into two categories “3A” and “3B”. There are several ways of developing pathology. Among them, wet and coagulation forms of necrosis should be highlighted, as well as fixation of changes under the influence of dry type heat.
Coagulation necrosis develops upon contact with an open flame or heated objects, as well as with prolonged exposure to steam. The victim's skin changes color, becoming red and dark. The lesion itself is painted black, and the tissues bordering the damaged area are painted red. Inflammatory processes that create a boundary between damaged and healthy tissues form towards the end of the first month.
In the third category of injury severity, only those burns whose diameter does not exceed two centimeters heal on their own. When carrying out first aid measures, it is very important to stop the process of damage to deep tissues, thereby preventing toxin poisoning and dehydration. Removal of serous contents and normalization of blood circulation is carried out only surgically.
During independent regeneration processes, the boundaries of the damaged layers grow inside the wound, which contributes to the formation of scars.
Depending on how deeply the tissues are affected, four degrees of burns are distinguished.
The wet form of necrosis is formed when clothing burns. The affected tissues initially swell, turning a soft pink color. The surface of the skin resembles torn shreds. This situation is often complicated by the addition of an infection.
“Fixation” of the skin is formed under the influence of infrared radiation. During the first three days, local body temperature and color change, swelling and redness appear. A dry scab forms approximately on the fourth day after injury. Further, the clinical picture is similar to coagulation-type necrosis.
Often, burn injuries lead to partial loss of skin sensitivity at the affected area. In the case where the muscle-binding tissues are affected, the mobility of the damaged limb is limited. The formation of rough scars and cicatrices disrupts the elasticity of tissues. When an injury affects a large area of skin, poisoning from toxins produced during combustion occurs. Such injuries can lead to death due to severe irritation of receptors by toxic products.
How long does it take for a third degree burn to heal? In most cases, the formation of new tissue is influenced by factors such as first aid, correctness of therapy, nature and area of injury.
Fourth degree
With a fourth degree injury, the damage extends to the entire depth of the affected area. In many cases, tissue breakdown products poison internal organs, which leads to a state of shock. Therapy of this type of pathology is considered the most labor-intensive, since the lesion occurs on more than sixty percent of the skin area. Severe dehydration and intoxication also complicate therapy. The treatment of this form of burn injuries itself is carried out in an intensive care unit.
Often, in order to save a patient’s life, specialists have to resort to complex surgical operations, including transplantation of donor organs. Since the burn affects large areas of skin, in many cases patients require skin grafts. Necrosis is accompanied by the appearance of purulent exudate, which increases the risk associated with the occurrence of sepsis.
Having considered how many degrees of burns there are, we need to say the following. Many burn injuries of the third and fourth degree of severity cause internal changes that are incompatible with life. Only preventing dehydration, intoxication and other pathological processes will save the victim’s life. Unfortunately, the current level of the pharmaceutical industry does not allow the creation of fast-acting medications that affect the body at the molecular level. That is why the main method of treating burns is surgery.
Below are photos of the extent of the burns.
Each degree has its own characteristics that determine the depth of damage to the skin and underlying tissues
Causes
Depending on how the burn was received, the following types are distinguished:
Thermal
A consequence of injury from fire, boiling water, steam or touching hot objects.
Chemical
The result of exposure of soft tissue to acidic and alkaline solutions.
Electric
Formed at the entry/exit points of electrical charge.
Ray
When exposed to ultraviolet or ionizing radiation.
Classification by type of damage
Based on the type of damage, 4th degree burns are divided into three types:
- thermal;
- chemical;
- electric.
A thermal burn that occurs during prolonged exposure to any high-temperature agents can lead to complete necrosis of the affected segment. Necrosis extends not only to the skin, but also to deeper structures such as muscles, tendons, and bones. In some cases, a thermal burn results in charring.
4th degree chemical burns are extremely rare. Their number does not exceed 1% of the total number of such injuries. A chemical burn with a significant area leads to the appearance of long-term, non-healing, ulcerative wounds. In this case, the skin always requires prompt restoration.
4th degree electrical burns occur from high voltage injuries and are fatal in most cases. Such injuries most often occur at work and they are usually combined with thermal burns resulting from contact with burning clothing and hot objects. Electric current instantly affects all internal organs of the human body and causes shock, cardiac arrest, paralysis of the respiratory tract, resulting in clinical death. A favorable outcome is possible only with proper and timely provision of resuscitation actions.
Symptoms
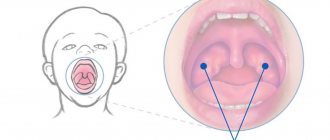
The clinical picture of a 2nd degree burn is as follows:
- inflammation and redness of the affected area;
- soreness to touch;
- swelling;
- blistering.
Blisters form immediately or after a short time. As a result of the detachment of the upper layer of the epidermis, a cavity is formed filled with a yellowish transparent liquid - blood plasma from broken capillaries. After a few days, the contents of the blister become cloudy.
Natural tearing may occur, followed by leakage of fluid and exposure of bright red wet erosion. Gradually, the resulting wound heals, and after two weeks it acquires the natural color of the skin.
When you get a sunburn, the skin turns red and becomes painful to the touch.
Somewhat later, many small blisters . To this picture you can add the symptoms of sunstroke - nausea and increased body temperature.
When an infection occurs, the affected area becomes purple and hot, and pus is discharged.
Diagnostics
2nd degree burns are diagnosed by visual inspection . The combustiologist determines the area of skin damage, the degree of swelling and the level of pain. The presence of infection is checked.
If there is a burn to the mucous membranes of the respiratory tract, an x-ray is taken . For large areas, a detailed blood and urine test .
After assessing the patient’s condition, a conclusion is made and appropriate treatment and prevention of complications are prescribed.
First aid
It turns out before the arrival of the medical team.
First of all, it is necessary to eliminate contact with the cause of the burn and call an ambulance, after which the following actions are performed:
- It is necessary to quickly cool the burned surface with running cold water (15-17°C). The fact is that after receiving a burn, the skin continues to heat up and break down for some time, thereby causing severe pain. Cold water will stop this process, thereby reducing the depth of skin damage. Constriction of blood vessels and decreased sensitivity of nerve endings produce an anesthetic effect. It is recommended to treat the resulting wound with cold for 20 to 60 minutes until the skin becomes numb. The water pressure should be low to avoid causing additional pain.
- In case of a chemical burn, the chemical substance is first removed using a sterile dry cloth, after which the remaining substance is also washed off with running cold water for 20-30 minutes.
- After washing the inflamed surface, apply a sterile gauze bandage.
- To relieve pain, you can take any painkillers. Effective pain relief with injections.
- If there is no vomiting, the victim is given lightly salted water to prevent dehydration.
What not to do when providing first aid:
- remove tissue stuck to burns;
- apply ice and cotton wool to the burn;
- use an adhesive bandage or bandage the wound tightly;
- treat damaged skin with coloring antiseptics - iodine, brilliant green, as well as sour cream and butter;
- pop blisters yourself.
If the area of the skin affected is small, and the resulting blisters are also small, it is permissible to treat the burn at home.
Mandatory hospitalization is required for adult victims with a lesion area of 5%, as well as children under one year old and children with burns of more than 2%. This also includes people with injuries to the face, neck, perineum, respiratory tract, as well as the elderly.
First aid and treatment
- First aid for a 4th degree burn is to eliminate the source of the injury. We must not forget about our own safety and come into contact with dangerous objects.
- Call emergency medical assistance. Describe in detail the condition of the victim, his injuries, age.
- Apply a bandage soaked in clean water and immerse the damaged organ in water. Keep for up to half an hour.
- After cooling, change the dressing if necessary. Make sure it is moistened with cold water.
- Provide rest to the victim, numb the wound with injections (do not use external agents - ointments).
- After first aid, carefully remove clothing, jewelry, and cut off any adhering material along the edge of the burn. Do not tear off burnt fabric.
It is prohibited to use other pre-medical measures to avoid worsening the victim’s condition.
After being admitted to a hospital, before treatment, the victim is prescribed painkillers, including anesthesia. If burn shock occurs, appropriate measures are taken.
Next, the patient’s internal systems are stabilized, breathing is restored, a blood transfusion is given, and the mineral balance is restored.
Once the risk to life has been eliminated, the wound is cleared of dead tissue. To prevent the spread of necrosis, the edges of the wound are excised. A course of drugs that promote regeneration is prescribed. A prognosis for further treatment is made.
For stage 4 lesions, surgical therapy is used exclusively. It requires sophisticated equipment to contain the patient. It involves applying dry skin bandages to damaged areas, which accelerates regeneration.
At the end of treatment, the patient is prescribed skin grafting. It is required to eliminate significant damage. Previously, plastic surgeons used the patient’s own skin or donor skin. The new key to solving problems in skin grafting is artificial skin and xenografts.
Post-burn recovery process
For second degree burns, the recovery process takes 12-15 days .
It is important during this period to properly care for the wound, avoiding exposure to traumatic events, as well as infection. Local drugs must be selected correctly to accelerate cell regeneration.
If the wound becomes infected, recovery time may be significantly longer.
There are three stages of healing of wounds resulting from a 2nd degree burn:
Purulent-necrotic
Under the wall of the blister, the contents gradually become cloudy and pus forms.
The adjacent skin becomes inflamed. The blister begins to swell and, if large, requires opening it. It is advisable that this procedure be performed by a doctor. If this is not possible, then the blister is opened independently, following the rules of disinfection. To do this, the burn surface is treated with an antiseptic, and a puncture is made with a sterile needle. The leaked pus is carefully removed with a clean napkin, and the wound is treated with anti-burn or antibacterial ointment.
After this, a sterile bandage is applied.
Granulation
At this stage, gradual restoration of the affected cells occurs.
Inflammation and blisters disappear. A bandage is no longer required; moreover, contact of the wound with clothing and other surfaces that can rub it is limited.
The surface of the burn is regularly treated with wound-healing ointments to prevent it from drying out and, as a result, the formation of cracks. It is important to eliminate the risk of re-infection of the wound.
Epithelialization
The last phase of wound healing is observed - it is covered with new skin.
Regenerating ointments are still used to speed up this process.
When caring for a burn wound, the key is to protect against infection by following antiseptic rules.
It is not recommended to wet the wound with water. The dressings are changed as they get wet and the procedure for treating the injured surface is performed. At each dressing change, the condition of the skin is assessed and a conclusion is made for further therapy.
Forecast and prevention of complications
Fourth degree burns have three main complications:
- Tissue necrosis. Medical intervention will reduce the risk of complications and the appearance of gangrene. Infectious wounds can cause inflammation and ulcers. Timely replacement of dressings, wound care, and compliance with sterile conditions will ensure proper protection.
- Damage to internal organs. With thermal burns, the temperature by inertia penetrates deeper into the body, affecting important organs. Electric arc pulses hit them directly. Emergency cooling will help prevent this.
- Intoxication of the body with decay products of dead tissue. Immunomodulators, blood transfusions, restoration of mineral balance will have a beneficial effect, cleanse the body, and restore its processes.
The article has been verified by the editors
Drug treatment
Correctly selected treatment will speed up the healing process of a burn wound. For this, a number of drugs or their analogues, both general and local, are used.
All medications must be prescribed by a doctor. It is necessary to strictly observe the dosage and rules for their administration.
Anti-inflammatory drugs
For the treatment of second-degree burns, the main emphasis is on anti-inflammatory drugs that have a local antibacterial effect: Levomekol, Syntomycin emulsion, Furacilin ointment, Gentamicin ointment and many others like them.
Antiseptics
Miramistin and Chlorhexidine, which have proven themselves well in first aid practice, as well as a 0.5% dioxidine solution are often used as antiseptics.
Ointments containing Panthenol
Today, moisturizing healing ointments containing Panthenol have become popular: Bepanten, D-panthenol, which help accelerate the restoration of the skin at the regeneration stage.
Spray
Effective is the use of Panthenol spray, which is applied to the surface of the skin by spraying without physical contact with the wound.
Homeopathic remedies
Among the homeopathic remedies, Traumeel C ointment, as well as sea buckthorn oil, have proven themselves well.
Antihistamines
It is acceptable to use antihistamines that help relieve swelling and itching of damaged tissues: Suprastin, Zodak, Claritin.
It should be noted that some antihistamines cause drowsiness.
Analgesics
Any analgesic is most often taken as a pain reliever.
In case of severe pain, you can take Ketorol or its analogues. Injections with painkillers are effective.
Vitamins
As an additional treatment, the doctor may prescribe vitamins A (retinol), E (tocopherol) and ascorbic acid, which are responsible for the production of collagen and enhance the regenerative function of the body.
During the treatment process, it is important for the victim to maintain a water-drinking balance to more quickly remove toxins from the body. It is recommended to include foods rich in proteins and carbohydrates in your diet to replenish the loss of energy that accompanies burn injuries.
Medical information portal "Vivmed"
CONSEQUENCES OF THERMAL, CHEMICAL BURNS AND FROSTBITE.
Burns. like frostbite, they are dangerous due to the development of shock, damage to the skin, central nervous, cardiovascular systems, respiratory organs, if acid or alkali gets ingested - damage to the digestive tract (oral mucosa, esophagus, stomach), changes in kidney function, impaired water intake -salt metabolism, development of coma. With IV degree burns or frostbite, necrosis (death of tissue) occurs down to the bones. The percentage of deaths is high with IV degree burns and frostbite. With burns, the development of burn disease is possible. During its course, 4 periods are distinguished: burn shock, acute burn toxemia, septicotoxemia, convalescence. Burn shock develops 1-2 hours after the burn and lasts 2 days: blood pressure decreases, anuria develops, and the general condition is severe. Shock occurs with 1st degree burns of more than 30% of the body surface and with 2nd-4th degree burns - more than 10%. Acute burn toxemia develops after shock and is characterized by high fever, loss of appetite, weak rapid pulse, and slow healing of burn wounds. Lasts 4-12 days. Fever can last for months (40° and above). Complications develop: pneumonia, arthritis, sepsis, anemia, intestinal atony, bedsores. Septicopyemia develops with suppuration of burn wounds, which leads to burn exhaustion. A remitting fever is noted. Appetite disappears, anemia increases, disturbances in water-salt, electrolyte balance, and metabolism intensify. Bacteremia and dysproteinemia develop. Antibodies accumulate in the blood of a burned person, phagocytosis increases, and granulations form. Patients continue to lose weight. Wounds do not heal for a long time; a large amount of Pseudomonas aeruginosa, putrefactive integument, and Proteus are observed in the wound. Large loss of protein, prolonged intoxication, burn exhaustion, bedsores lead to muscle atrophy and stiffness in the joints. Death occurs as a result of the development of sepsis against the background of anemia, severe disorders of all types of metabolism, especially protein. The period of convalescence begins gradually in the case of healing of burn wounds and lasts for many years. Often accompanied by amyloidosis of internal organs, chronic nephritis, which requires systematic ongoing treatment. Chemical burns can occur when taking alkalis and acids. Deep damage to the tissues of the digestive tract and respiratory tract develops. Burns of the oral cavity always occur, manifested by drooling. In 30-40% of people who take alkali, burns of the esophagus occur, followed by the development of esophageal stricture, stomach damage, complicated by perforation (if liquid alkaline bleaches get inside). When the upper respiratory tract is affected, obstruction and stridor develop, requiring emergency assistance. In acid poisoning, tissue damage is not as deep as in alkali poisoning. Characterized by more frequent damage to the stomach than the esophagus, since the epithelium of the esophagus is resistant to acids. Consequences of thermal and chemical frostbite. With frostbite of the third degree, death of the skin, subcutaneous tissues and muscles occurs, with the fourth degree - tendons and bones. With severe hypothermia, coma develops. At 18 °C and below, electrical activity on the electroencephalogram disappears. If such patients survive, then central pectin myelinolysis sometimes develops. When the cardiovascular system is damaged, bradycardia and a decrease in blood pressure progress if the temperature drops below 29 °C or lower. At 22 °C, ventricular fibrillation develops, and at 18 °C and below, asystole occurs. Damage to the respiratory organs with a decrease in body temperature is characterized by a progressive decrease in tidal volume and respiratory rate. Changes in kidney function occur: cold diuresis and impaired concentration function of the tubules develop. In the long term, consequences such as severe cicatricial deformities of the trunk and limbs, joint contractures, defective stumps, trophic ulcers, and terminal osteomyelitis, requiring surgical and orthopedic treatment, may develop.
CONSEQUENCES OF THERMAL AND CHEMICAL BURNS OF THE HEAD AND NECK.
With deep burns of the calvarium with bone damage, there is a risk of developing epi- and subdural abscesses, since they are often asymptomatic. Also, with such burns, meningitis may develop. As a result of deep burns of the skin and underlying tissues, there is often incomplete restoration of the lost skin, which leads to the development of burn deformities. Third degree burns of the auricles are often complicated by the development of chondrites. It is possible to develop a burn to the oral cavity, esophagus, and stomach. With deep burns of the head and neck, a rapid death is possible. With frostbite of the head and neck, infectious complications are often observed (in the II degree), and the development of a wound infection is possible (in the III and IV degrees). Abscesses and adenophlegmons form from suppurating lymph nodes. Local suppurative processes occur with purulent-resorptive fever, which, with a long process, leads to wound exhaustion. At the site of scars, the development of squamous cell carcinoma and fungal skin lesions is possible. Changes in nerves, blood and lymphatic vessels are also observed (for example, neuritis of the facial nerve, lymphangitis, thrombophlebitis, etc.).
CONSEQUENCES OF THERMAL AND CHEMICAL BURNS AND FROSTBOST OF THE UPPER LIMB
With burns of the upper limb, contractures often develop (this is a burn deformity as a result of deep burns of the skin and underlying tissues). The development of ankylosis, dislocations, subluxations, as well as long-term trophic ulcers may occur. In case of burns with acids, tissue death occurs as a type of dry necrosis, in case of burns with alkalis - wet necrosis. Local complications include purulent arthritis, furunculosis, and in case of circular burns - gangrene of the limb. With frostbite of the upper limb, ischemia of the limbs may develop as a result of damage to nerves, blood and lymphatic vessels. With the development of cold neurovasculitis, the pulsation of blood vessels in the limbs sharply weakens, the hands swell, sweating increases, and the hands become wet. Tactile sensitivity changes in the area of the hands; patients cannot confidently grasp objects or perform precise movements. In connection with neurovascular disorders, trophic changes in the tissues of the limb develop with the formation of skin ulcers, “sucked fingers,” and clubbed fingers. Squamous cell carcinoma may develop in place of scars after frostbite. When the demarcation line passes through the bone, inflammation can develop in the form of progressive osteomyelitis, and when passing through the joint, progressive purulent osteoarthritis can develop. With degrees III and IV frostbite, a wound infection (purulent, putrefactive, anaerobic) can develop, which can be accompanied by lymphangitis, lymphadenitis, thrombophlebitis, purulent phlebitis.
CONSEQUENCES OF THERMAL AND CHEMICAL BURNS OF THE LOWER LIMB.
Most often, contractures (burn deformities) occur after a burn due to deep damage to the skin and underlying tissues. Subluxations, dislocations and ankylosis, as well as long-term trophic ulcers, are less common. Locally in the area of the burn, purulent arthritis, phlegmon, furunculosis develop, and with circular burns - gangrene of the limb. Frostbite of the legs, complicated by cold neurovasculitis, is often the cause of obliterating endarteritis. With the development of cold neurovasculitis, the pulsation of blood vessels in the extremities sharply weakens, the legs swell, sweating increases and the extremities become wet. Patients experience a feeling of expansion, compression, and burning in the extremities. In the area of the feet, tactile sensitivity changes, patients cannot perform precise movements, lose the feeling of the foot when walking, and if increased tactile sensitivity develops after frostbite, then touching, squeezing, and wearing shoes are accompanied by pain. Due to changes in blood vessels and nerves, dermatoses and trophic changes in the tissues of the extremities develop with the formation of clubbed fingers, “sucked fingers,” and skin ulcers. Sometimes squamous cell carcinoma develops in place of scars after frostbite. With III and IV degrees of frostbite, any wound infection can develop: putrefactive, purulent, anaerobic, accompanied by purulent phlebitis, thrombophlebitis, lymphadenitis, lymphangitis; adenophlegmons and abscesses are formed from suppurating lymph nodes. If the demarcation line passes through the bone, then inflammation develops in the form of progressive osteomyelitis; when passing through the joint, purulent progressive osteoarthritis develops.
CONSEQUENCES OF THERMAL AND CHEMICAL BURNS OF THE TORSO. With extensive burns, the main complication is burn disease.
Thus, during periods of toxemia and septicotoxemia, lobar, focal or lobar pneumonia may develop due to damage to the respiratory organs by combustion products. Occasionally, myocardial infarction develops, and in the period of septicotoxemia - pericarditis. Acute ulcers of the gastrointestinal tract (peptic ulcer) often develop, accompanied by bleeding or perforation. Sometimes gangrenous or acalculous cholecystitis develops. Other complications may also develop, such as acute pancreatitis, acute intestinal obstruction, and thrombosis of abdominal vessels. With severe burn intoxication, bilirubinemia, increased bleeding of granulations, and sometimes acholia of feces can be observed, which indicates the development of liver failure, serum or toxic hepatitis with a predominance of anicteric forms. The most serious complication of burn disease is sepsis. In the later stages after a burn, pyelonephritis, pyelitis, and nephritis can develop. With burn exhaustion (a complication of the period of burn septicotoxemia), the development of mono- and polyneuritis and urinary stones is possible.
In the area of thermal damage, the development of furunculosis, phlegmon, and anaerobic infection is possible.
Burns caused by acids and alkalis cause damage to the oral mucosa, esophagus, and intestines. In case of burns with acids, the state of cell colloids changes, dehydration and coagulation of tissues are observed, and their death occurs as a type of dry necrosis. Alkalies, interacting with proteins, form alkaline albuminates, saponify fats, and wet necrosis develops. With frostbite, widespread local suppurative processes occur with purulent-resorptive fever, and therefore, with prolonged suppuration, wound exhaustion can develop.
In severe forms of frostbite, changes in internal organs are also observed: inflammatory diseases of the respiratory tract, gums (stomatitis, etc.), stomach, duodenum, colon; fungal infections of the skin and nails, arthrosis, may develop.
vivmed.ru
What to do with bubbles?
Blisters are the first sign of a second degree burn.
Manipulations with them must be extremely careful and depend, first of all, on their size.
- If the blisters are small, then with proper care of the burn they will gradually disappear on their own.
- When the bubbles swell, puncture is required to remove the contents, as well as its shell. In this case, it is advisable to seek the help of a doctor who will perform the necessary procedure in compliance with all the rules.
- In case of a natural tear, first of all, it is necessary to treat the surface of the burn from contamination with an antiseptic, for example, 3% hydrogen peroxide. Then, using sharp sterile scissors, cut off the membrane of the bladder and apply antibacterial ointment.
It is important to consult a doctor promptly after manipulating blisters if necessary. The formation of purulent plaque and an increase in temperature indicate infection of the wound, in which case general antibiotics are usually prescribed.
First aid for second degree injuries
A large burn area requires an emergency call to the doctors. First aid consists of mandatory cooling of the damaged area. The further algorithm for providing assistance depends on the type.
- In case of thermal damage, rinse immediately with cold water. The skin continues to heat up after exposure to high temperatures and it is urgent to cool it down to prevent further spread of inflammation. Ice water flowing in a small stream acts as an anesthetic. Pain sensations are reduced.
- In case of chemical exposure, the wound should be cleaned of corrosive substances with a sterile cloth. Then rinse with cold water to stop the heating and remove any remaining chemicals. Traditional medicine practices the use of soda, the properties of which reduce the reaction rate and prevent the spread of acid burns.
- The skin suffers from an electric shock and a person may lose consciousness. First of all, sources of electricity are eliminated. If there is no pulse and breathing, before the doctor arrives, you should independently perform resuscitation (artificial respiration and closed cardiac massage). After making sure that the victim is conscious, you can wash the burned area with cold water.
- Burns from prolonged exposure to the sun should be cooled with water, but make sure there is no significant temperature difference. It is necessary to cover the affected areas from direct exposure to ultraviolet radiation.
Before doctors arrive, it is not advisable to apply sterile dressings; specialists should perform an initial examination of the wound. Unnecessary manipulations can cause additional pain. In case of accidents, the extent of injury must be objectively assessed. You can help on your own with minor burns and ensure a person’s well-being is stable. In case of loss of consciousness and a large area of damaged tissue, medical assistance is required.
Actions for inflammation
The presence of an inflammatory process indicates that harmful bacteria and viruses have entered the body. Characterized by fever, chills, and weakness. As a result, the recovery process is delayed, and a scar may form . In such cases, you should not delay your visit to the doctor, otherwise death is possible.
systemic antibiotics first . Moisturizing ointments are replaced with antiseptics and ointments with antibacterial action .
In the absence of purulent plaque during the recovery stage, the wound is treated with aerosols , which form a protective film on the surface that prevents the penetration of harmful microbes.
In each individual case, the treatment regimen and selection of drugs are carried out taking into account the individual characteristics of the body.
Danger and consequences of serious injury
Deep burns can cause not only irreparable harm to health, but are life-threatening to the patient. Patients often suffer from burn shock and the consequences of burn disease. As a result of the entry of pathogenic bacteria into the body, sepsis develops and more extensive damage occurs, since with severe traumatic injuries the immunity and protective functions of the body decrease. In case of severe exhaustion of the body, surgical and medicinal treatment measures aimed at eliminating the causative agents of infectious diseases and excision of purulent areas should be provided as quickly as possible. Burns that affect more than 10% of the body surface or spread deep inside, affecting bone tissue, are highly dangerous.
Child's burn
If a child has suffered from a burn, it is necessary to provide him with first aid according to the same scheme as indicated above. Every parent should have these , since even the most obedient baby is not immune from an accident. When determining the second degree of burn , you should not hesitate to call a doctor , who will determine the severity and area of skin damage and decide on the need for hospitalization.
The principles of treating burns in children are the same as for adults, with the only difference being that the dosages of prescribed drugs are determined taking into account the age and weight of the patient, and treatment procedures are often carried out under the influence of painkillers. Additionally, physiotherapy may also be prescribed to speed up the recovery process.
Under no circumstances should you treat your child at home without the supervision of a doctor. The slightest carelessness can lead to worsening health conditions.
A burn is a type of wound that requires close attention and careful handling. Any initiative in this matter is unacceptable. A timely visit to a specialist will not only help you quickly restore your health, but will also help you avoid the risk of complications that can have negative consequences.
Consequences of burns
Burns are considered one of the most severe injuries, from which every fifteenth victim dies. The consequences of burns depend on how deeply the tissues were affected, which organs were damaged, and the area affected. The provided pre-medical and first emergency aid also plays an important role.
The main consequences of burns are scars. If a burn wound heals in less than two weeks, then the scar that forms is hardly noticeable and soon ceases to stand out at all. But if the burn was deep, the wounds take a long time to heal and always leave a rough scar. Until half a year, scars are considered immature; they often itch, have a bright color and grow. It is during the period of scar formation that it is worth using special creams and ointments that can reduce it.
The location of the scar is also very important, because if it is located somewhere on the arm, back or thigh, it does not cause much discomfort, but if the face or open areas of the body are injured, then this brings great inconvenience and causes complexes in the victims, because scars in most cases look unsightly and attract the attention of strangers. Scars can also be functional defects; affected eyes, ears, joints can lose their main function, and a person becomes disabled.
In addition to scars, there are other serious consequences - people who have suffered burns without scar formation become nervous, irritable and morally unstable, and people who have post-burn scars, especially deforming and disfiguring ones, often withdraw into themselves and try not to leave the house, which leads to social rejection.
As you can see, the consequences of burns are quite serious, so during the rehabilitation period every effort should be made to avoid the formation of scars.
improvehealth.ru