Schlatter's disease is the pathological process of aseptic destruction of the core and tuberosity of the tibia, which occurs against the background of their frequent injury. As a rule, the disease develops during intensive skeletal growth. Its main manifestations are pain localized in the knee joint (its lower part).
Schlatter's disease is diagnosed based on examination, a comprehensive assessment of medical history, X-ray and computed tomography of the knee joint, as well as laboratory tests and local densitometry. For the treatment of Schlatter's disease, painkillers and anti-inflammatory drugs, exercise therapy, massage, physiotherapeutic procedures are usually prescribed, and it is also recommended to maintain a gentle motor regimen for the affected knee joint.
general information
The tibia is a bone of the lower leg, the upper edge of which connects with the femur, forming the knee joint, and the lower edge with the talus, passing into the medial malleolus. At the top of the tibia is the tuberosity, the area to which the quadriceps femoris tendon is attached.
In children, all tubular bones have growth points - places where bones connect with cartilage. Thanks to these zones, bones can grow in length. The tibial tuberosity is one of the points of ossification. In children, it is loosely fused with the rest of the bone and is easily injured, which leads to osteochondropathy - a disruption in the delivery of nutrients to the bone tissue and aseptic necrosis (death) of the tuberosity.
This condition was described in 1906 by physician Osgood-Schlatter. It develops in adolescents aged 10-18 years. May affect one or both legs. As the patient grows, the junction of the tuberosity and the main part of the tibia becomes strong, so Schlatter's disease does not occur in adults.
Prevention
To avoid Schlatter's disease in adolescents, you must follow these recommendations:
- when playing sports, you need to alternate exercise with rest; during this period, proper nutrition is very important;
- in case of injuries or any damage to the knee joint, you must seek medical help and be sure to undergo a full course of treatment;
- Do not overload your limbs.
Only timely access to the hospital is the key to a teenager’s health. You need to be attentive to your health, then you will be able to avoid more serious complications.
There are no similar articles.
After eliminating all irritating factors, resting the injured knee and conducting a complex of moderate therapy, the patient must continue to take precautions.
To prevent Osgood-Schlatter disease in adolescents in the future, you need to relieve the joint and avoid provocateurs of the disease (jumping, running, kneeling). You can replace your usual sports with more loyal ones (swimming, cycling), although, as a rule, after treatment, restrictions on playing sports are lifted.
Preventive measures are not always a guarantee that the disease will not manifest itself again. Any microtrauma can develop into Osgood-Schlatter disease if it is not noticed in time and treatment is not started. Children and adolescents are always at risk, whose constant activities (dancing, sports) carry the risk of injury to the lower extremities.
Causes
The cause of Osgood-Schlatter disease is injury to the tuberosity and nucleus of the tibia during the period of active skeletal growth. Pathology can be caused by direct damage to the knee joint - sprains and ruptures of ligaments, fractures, dislocations. But more often it occurs due to chronic microtrauma during intense sports.
The sports that most often provoke Schlatter's disease in adolescents include hockey, football, fencing, cycling, volleyball, basketball, weightlifting, artistic gymnastics, wrestling, acrobatics, alpine skiing, figure skating, and so on.
Schlatter's disease is diagnosed in 15-20% of children involved in sports. The incidence rate among adolescents who do not experience significant physical activity is 3-5%. The likelihood of developing the disease does not depend on gender. But boys encounter it more often due to the fact that they actively participate in sports sections.
Causes of development of Schlatter's disease
Schlatter's disease was first described by Osgood Schlatter at the beginning of the 20th century. It has a non-inflammatory genesis and is accompanied by necrosis of bone tissue. The disease is observed in children 10-18 years old during the most intensive bone growth, most often in boys. In some cases, the pathology occurs on one limb, but often the disease affects both legs.
Factors contributing to its development may be:
- Injuries, including dislocations, damage to knee ligaments, various fractures;
- Persistent minor knee injuries that occur during sports activities.
According to statistics, Schlatter's disease occurs in every fifth teenager who is actively involved in sports. Among the most dangerous sports that contribute to the development of the disease, doctors note hockey, basketball, volleyball, gymnastics, football, and figure skating. Ballet classes can also provoke the development of the disease. Much less often (in 5% of cases) pathology develops in less active children.
Pathogenesis
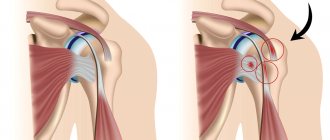
Schlatter's disease in children develops as follows. Stress loads on the triceps tendon caused by jumping, compression, or injury are transferred to the immature tibial tuberosity. As a result, its blood supply and nutrition are disrupted, resulting in areas of necrosis that lead to rupture.
Due to the tension of the tendon, the tuberosity fragments cannot align with the main part of the bone. As a result, pathological bone growths, swelling and inflammation occur in this area - the main manifestations of Schlatter's disease.
Treatment at home
Therapy with folk remedies can be an addition to the main course, but not the basis of treatment.
You can cure Schlatter at home by wearing a bandage, warming it with mud and paraffin, as well as oil compresses. They need to be done at night. You can use sunflower or olive oil, heat it and apply it to a cloth. Then apply the compress to the sore spot, wrap it in cellophane and wrap it with a warm towel.
Herbal compresses will help relieve pain and swelling. To prepare, pour 5 tbsp of boiling water. l. comfrey and black root roots, leave for 12 hours. Apply the compress overnight.
Treatment with folk remedies can last from one to several months, depending on the degree of the disease.
Symptoms
Symptoms of Osgood-Schlatter disease appear gradually. At first, mild pain occurs in the knee when bending, squatting, or walking up stairs. As the pathology develops or after intense exercise, the unpleasant sensations intensify and other signs are added to them.
Symptoms of Schlatter's disease at the stage of manifestation:
- cutting pain in the front of the knee, increasing during movement and weakening at rest;
- swelling (edema) of the knee joint without redness and hyperthermia of the skin;
- thigh muscle tension;
- limitation of joint mobility;
- the formation of a lump of bone tissue on the front of the tibia under the kneecap, which does not interfere with the function of the knee.
A man with Osgood-Schlatter disease.
The severity of pain can vary from minor to very severe.
Osgood-Schlatter disease is characterized by a chronic course: over 2 years, exacerbations lasting from 2 weeks to 2-3 months are replaced by periods of remission.
How to treat Schlatter's disease of the knee in adolescents?
Schlatter's disease of the knee joint in a teenager
This is an aseptic (non-inflammatory) injury to the upper third of the tibia, usually occurring in childhood and adolescence in the range from nine to eighteen years, characterized by damage to the tissues of the bone and cartilage of the leg.
The disease manifests itself by the formation of a growth just under the kneecap, which is easy to notice visually. The Swiss surgeon Dr. Schlatter, in collaboration with his US colleague Dr. Osgood, described and systematized data on the disease in December 1905. Therefore, in medical reference books the name of this disease is often referred to as Osgood-Schlatter disease.
Also, when making a diagnosis, doctors often write down the disease as osteochondropathy of the tibial tuberosity.
The clinical picture of the disease is the destruction of bone and cartilage tissue of the tibia. For no good reason, a swelling forms in the lower part of the kneecap, which is hard to the touch. In the International Classification of Diseases, the syndrome belongs to the ICD-10 class.
In children and adolescents, the skeleton is not yet fully formed. It is at this age that bones are most susceptible to injury. The disease is non-infectious. Inflammation does not occur with it. In children, unilateral bone lesions are most often observed. Less commonly, both limbs are affected.
And although Osgood-Schlatter disease is more common in boys, the gender gap narrows as girls become more involved in sports. Osgood-Schlatter disease affects more adolescents who play sports (by a ratio of one to five).
A feature of this type of osteochondropathy is the benign and often completely asymptomatic course of the disease. After some time, the pathology begins to regress on its own, and the patient never learns about his condition. In other cases, Schlatter's disease is an incidental finding during radiography of the knee joints for another reason.
Schlatter's disease manifests itself in different ways in children. The main symptoms are:
- Swelling of the knee joint
- Painful sensations in the area of the tibia
- The pain gets worse when you move your knee
- Tension of ligaments and muscles in the affected knee joint
- Limitation of joint movement, which can significantly harm the athlete in achieving high results
- Muscle wasting. In this case, the knee joint may become too mobile
At the very beginning, Osgut-Schlatter disease has minor symptoms. Typically, patients do not think that the pain that appears in the knee is associated with its injury. Gradually, the pain increases, especially when bending the leg at the knee, during squats, going up and down stairs.
The lower part of the knee begins to hurt very much, especially when bending when walking or running, subsiding when at rest.
Sometimes knee pain can be sharp and cutting, localized in the front of the joint, where the patellar tendon attaches to the tibial tuberosity. This area also swells.
During examination of the knee, swelling is noticeable, due to which the outlines of the tibial tuberosity are smoothed out. On palpation, the knee is painful, and the swelling has a dense elastic consistency and a hard protrusion is palpated through it. Pain in the knee that occurs during active movements varies in intensity.
Osgood Schlatter's disease usually occurs in a chronic form, but sometimes it can be wavy and have pronounced periods of exacerbation. The disease, as a rule, lasts no longer than two years and leads to complete recovery of the patient by the time his bones stop growing (by the age of seventeen to nineteen).
Risk factors
The main risk factors for developing Osgood-Schlatter disease are age, gender and participation in sports.
Age
Osgood-Schlatter disease occurs during puberty and growth of the body. The age range is different for boys and girls because maturation begins earlier in girls. Osgood-Schlatter disease usually develops in boys aged 13-14 years and in girls aged 11-12 years.
Age ranges differ by sex because girls experience puberty earlier than boys.
Sports activities
Treatment of Schlatter's disease should be started only after visiting your doctor. Self-medication is unacceptable. The treatment course can be prescribed by a traumatologist, orthopedist or surgeon.
Diagnostics
Diagnosis of Osgood-Schlatter disease is based on:
- taking anamnesis;
- inspection and palpation;
- instrumental methods;
- laboratory research.
While collecting anamnesis, the doctor finds out what worries the patient, when the first symptoms appeared, whether there were injuries to the limbs, and so on. When examining the knee, its swelling is detected, and when palpating the area of the tuberosity, pain and elastic swelling are detected, through which a protrusion can be felt.
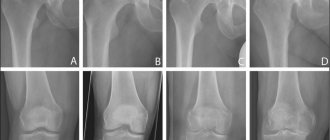
The main instrumental method is radiography. It is carried out in direct and lateral projections. It is advisable to monitor the X-ray picture over time.
Lateral radiograph of the knee joint of an adolescent with Schlatter's disease
X-rays for Schlatter's disease in children show:
- at the initial stage - flattening of the covering of the tibial tuberosity and raising of the lower border of the adipose tissue, while there are no changes in the nuclei;
- at the stage of progression - displacement of the ossification nuclei upward and forward, unclearness of their structure and contours, bone agglomerate - a spiky protrusion from pathologically overgrown tissue.
Another method for diagnosing Schlatter's disease is radioisotope scanning. Its essence is the introduction of a radioactive drug into the patient’s body - isotopes that are safe for health and emit weak rays. After the substance is distributed in the tissues, the radiation level is assessed and pathological areas are identified.
Additionally, instrumental diagnostic methods such as ultrasound, MRI or CT of the knee joint, as well as densitometry - an x-ray method for determining bone density, can be used.
Laboratory tests for Schlatter's disease are carried out to exclude the infectious nature of the inflammatory process. These include:
- general blood analysis;
- tests for rheumatoid factor.
The disease is differentiated from arthritis, fracture, syphilis, osteomyelitis, cancer, tuberculosis.
Possible complications
If the disease is diagnosed in time and treatment is started, complications usually do not arise. But no doctor can confidently predict the outcome of events, so prevention is necessary and important.
If prolonged stress is placed on the tibia tuberosity, the patella will begin to dislodge. This will disrupt the functioning of the knee joint, which will lead to complete immobility of the lower leg. Any movement will be accompanied by pain.
There have been cases in medicine when the joint developed incorrectly, which led to its deformation and degenerative processes. Subsequently, arthrosis may develop, and with this disease, pain will always be present, even with minimal physical exertion. In addition, there is stiffness and inflexibility in the knee joint.
Treatment
How to treat Schlatter's disease is determined by an orthopedic surgeon. The choice of tactics depends on the patient’s condition and the dynamics of the pathological process. A mandatory therapeutic measure is to limit physical activity. Sometimes complete exemption from physical education during the acute period is required.
In severe cases, it is recommended to immobilize the limb by applying a plaster cuff. If the pain is mild, it is necessary to secure the joint with a bandage or elastic bandage.
Bandage for fixing the knee joint of a person with Schlatter's disease
The traditional course of treatment for Osgood-Schlatter disease includes:
- medicines;
- physiotherapeutic procedures;
- Exercise therapy and massage.
Pharmacological therapy is based on the use of non-steroidal anti-inflammatory drugs that have an analgesic effect. Among them are ibuprofen, nimesulide and others. They are prescribed to children in short courses. You can also apply cold to the knee to reduce pain.
Physiotherapy is aimed at improving blood circulation and nutrition of the tissues of the affected joint, restoring bone, reducing inflammation and discomfort. Schlatter's disease in adolescents involves the use of techniques such as:
- electrophoresis with calcium, procaine, lidocaine, aminophylline;
- shock wave therapy;
- mud baths;
- paraffin applications;
- UHF;
- ozokerite.
Physical therapy includes exercises to stretch the thigh muscles and work the hamstrings. Thanks to this, the load on the area of the articulation of the tuberosity and the tendon of the thigh muscle is reduced.
Treatment of Schlatter's disease, the symptoms of which are significant, can be surgical. The essence of the operation is to remove foci of tuberosity that have undergone necrosis and its subsequent fusion with the tibia using a graft.
Surgical treatment of Schlatter's disease is performed for children over 14 years of age if conservative therapy is ineffective. After the operation, a course of physiotherapy is prescribed to speed up the restoration of normal function of the limb.
Treatment of Schlatter's disease in adolescents at home with folk remedies, for example, oil compresses, is ineffective. But they can be used as an auxiliary therapy after consultation with the doctor.
Treatment of Osgood-Schlatter disease
Immediately after diagnosis, the patient will be asked to avoid exercise for at least 5-6 weeks. To prevent complications, physical rehabilitation is prescribed. In public hospitals, such classes are called exercise therapy. If there are no rehabilitation specialists in the city, then, in agreement with your doctor, you can independently perform exercises aimed at:
- strengthening the quadriceps muscle;
- hamstring stretching;
- stabilization of the knee joints.
It is recommended to relieve swelling and pain with ice compresses. If the disease was diagnosed after the popliteal bump appeared, you will have to wear a special elastic bandage or bandage on a daily basis.
If the pain is too acute (this often happens when juvenile osteochondrosis develops as a result of injury), then the doctor prescribes painkillers: Ibuprofen, Acetaminophen. Additionally, lidocaine injections are given, electrophoresis and magnetic therapy are performed. In rare cases, if a relapse has been diagnosed in older people, surgical excision of the tumor is performed. However, surgery is not prescribed without prior conservative treatment.
Forecast
Schlatter's disease in children has a favorable prognosis. Subject to the doctor's recommendations, in most cases it goes away by the end of skeletal development - 17-19 years.
Possible consequences of Osgood-Schlatter disease:
- painless lump on the front of the leg below the knee;
- discomfort in the knee joint when the weather changes.
In rare cases, with severe pathology, deformation of the knee joint occurs, and osteoarthritis occurs - a disease that is accompanied by damage to cartilage tissue. A person experiences pain when leaning on a limb.
To reduce the likelihood of negative consequences from Schlatter's disease, during and after the course of treatment the patient should avoid activities that involve jumping, squatting, running and any stress on the knees. The optimal sport is swimming.
Do people take into the army if they have Osgood-Schlatter disease? According to regulatory documents, this pathology is not a basis for declaring a conscript unfit for military service. An exception may be cases of severe dysfunction of the knee joint caused by osteochondropathy of the tibial tuberosity.
Causes
The disease is typical for young healthy people 10–18 years old, when active skeletal growth occurs. In adults and children under 10 years of age, Osgood-Schlatter disease is practically not diagnosed. The occurrence of osteochondropathy does not depend on gender, but boys are at risk, since they are exposed to more physical stress than girls. The main causes of pathology are:
- bruises and knee injuries;
- shin fractures;
- damage to the knee ligaments;
- excessive physical activity.
Teenagers involved in professional sports are especially susceptible to the disease. About a quarter of all professional athletes suffered osteochondropathy of the tibial tuberosity in adolescence. The most risky sports include:
- football;
- hockey;
- volleyball;
- Athletics;
- Weightlifting;
- gymnastics;
- acrobatics;
- ski race;
- cycling;
- kickboxing.
In addition, Schlatter syndrome is often detected in adolescents involved in mountaineering, professional tourism, dancing and ballet.
Recently, there has been a surge in incidence due to the growing popularity of sports sections and clubs in our country.
Schlatter's disease is characterized by an asymptomatic onset. But over time, slight pain appears when walking, bending and straightening the knee. At rest, no pain is felt.
If there was no injury, then the patient usually does not associate the pain that appears with a serious pathology and does not consult a doctor. However, the consequences of a negligent attitude towards one’s health are not long in coming.
https://www.youtube.com/watch?v=6p3xX4DyC5s
After a short time, the pain in the lower part of the knee joint intensifies after each workout or intense physical activity. Then attacks of acute cutting pain occur with any movement of the leg, the area of the knee joint swells. Sometimes the patient has difficulty sitting down and getting up.
With Schlatter's syndrome, only the knees hurt; redness, fever, general weakness and other symptoms are not observed.
The disease is diagnosed when a teenager visits a doctor. The specialist examines the patient, identifies swelling, and determines the location of the pathology.
To determine the extent of the disease and make the most accurate diagnosis, the doctor prescribes an X-ray examination of the knee joint.
X-ray reveals the contours of the epiphyses of the tibial tuberosity, thickening of the patellar ligament, and areas of calcium deposits in the knee joint.
However, X-ray examination is best done several times to see pathological changes over time.
Additionally, MRI, ultrasound and CT scans of the knee joint can be performed, which allow a detailed study of a specific case of pathology, obtain information about changes in the structures of bone and cartilage tissue, and exclude an infectious disease.
An effective method for diagnosing the disease is radioisotope scanning. A special low-radioactive liquid is injected into the patient’s vein. After a few hours the examination can be carried out. Radioisotope scanning also helps to select an effective treatment method.
Treatment methods
If you experience pain symptoms in the knee area, it is better not to postpone a visit to the doctor. The sooner treatment begins, the faster the disease will recede. As a rule, it is possible to completely relieve inflammation and get rid of pain in 8–10 months. In advanced cases, patients struggle with the disease for years.
A conservative treatment method with timely consultation with a doctor gives good results. The course of therapy consists of procedures such as:
- taking anti-inflammatory drugs;
- use of pain-relieving ointments and compresses;
- Exercise therapy.
As a rule, after a year, all symptoms of the disease completely disappear in adolescents. Only in some cases the disease reminds itself of itself with minor pain, but this lasts until the skeleton is completely formed.
Surgery is necessary if complications arise that cause severe pain in the knee that interferes with movement.
However, treatment with folk remedies must be agreed with a doctor.
The disease cannot be left to chance. If the inflammation is not treated, then in the future you can get serious problems with the functionality of the knees.
Some symptoms of the disease persist for life, causing significant discomfort when moving the legs. Many young people who have suffered from the disease are interested in whether they are accepted into the army with Schlatter syndrome.
If the disease is not completely removed, then you will have to forget about both your sports career and military service.
If children are diagnosed with Schlatter syndrome, then they have to radically reconsider their lifestyle. The rehabilitation period takes about a year. During this time, the patient is advised to protect his knees as much as possible. To strengthen the immune system and improve the overall health of the body, it is worth visiting specialized sanatoriums.
During the recovery period, any risk of knee injury is eliminated. For the first months, the patient is not allowed to jump, run, or squat. In the future, the load on the knees can be increased, but knee pads should be used during any physical exercise. Often, the attending physician prescribes a whole set of exercises for the patient to strengthen and develop the knee joint.
Exercise helps relieve the discomfort associated with the disease and also prevent the risk of relapse. A special massage has a beneficial effect on the knee joint. Although you can learn self-massage from the photo, performing it at home.
In most cases, the disease is treated successfully, but the patient cannot return to professional sports. After the recovery period, teenagers often continue to lead an active lifestyle, but avoid excessive stress on their knees. Dangerous sports can be replaced with more gentle activities - swimming in the pool, rowing, etc.
Treatment methods
Schlatter's disease is treatable in most cases.
Medication:
- Taking painkillers with an effect on inflammation ( Tylenol , ibuprofen ). The course of admission is insignificant.
- Vitamin complexes (in particular vitamin B).
Physiotherapy:
- Ultrasound therapy options are used, which allows immediately after the first dose to significantly reduce the manifestation of symptoms.
- Magnetic therapy, in this case variants of a pulsed field are used, this effect provides relief from swelling and pain.
of physical education of a therapeutic plan is also used . This method is used to stretch the quadriceps muscle and develop the hamstring tendons. This allows you to reduce stress and prevent injuries.
It is recommended to reduce physical activity and keep the joint at rest. If swelling occurs, cold can be applied. Specialized knee pads are also used to ensure reduced load on the joint.
What are the symptoms of osteochondropathy?
The first signs that indicate the appearance of Schlatter's disease are pain in the knee that appears after physical activity. If the patient has suffered injuries to the knee joint, then the risk that a simple sprain has occurred increases significantly. At the initial stages of the disease, the pain is inconsistent, but as it progresses, it appears more often and becomes more powerful. In addition, people complain of the following symptoms:
- swelling in the knee area;
- swelling that occurs after sports or in the morning;
- severe pain during intense physical exertion.