Varieties
Treatment of dry pleurisy is almost always prescribed strictly individually.
In pulmonology, a similar general term is used to designate a group of inflammatory lesions of the pleura of various origins. In some cases, pleurisy can be independent or primary in nature, but usually develops as a secondary disease against the background of chronic or acute processes occurring in the lungs.
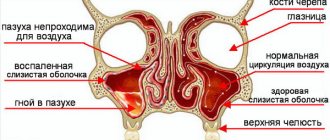
Depending on the presence or absence of effusion, several types of pleurisy are distinguished: they can be dry (or fibrinous), as well as exudative (serous-fibrinous, serous, purulent or hemorrhagic).
According to their origin, there are bacterial pleurisy (they can be specific or nonspecific), as well as tumor, viral, and traumatic.
Why the disease may occur
Most often, the causes of dry pleurisy come down to one of the following:
- Pneumonia.
- Tuberculosis of the lungs.
- Viral infection - enteroviruses of group B Coxsackievirus are most often associated with the dry form of the disease.
- Purulent processes affecting the tissue of the lungs or the spaces and organs located near the lungs.
In this case, pathogenic microorganisms are transferred to the pleura through the lymphatic system, that is, by the lymphogenous route, or through the bloodstream, that is, by the hematogenous route. And if the root cause is pneumonia, then there is also contact spread through inflammation of the lung tissue, spreading to the pleura itself.
Symptoms
Dry pleurisy has no independent meaning. Most cases of fibrinous pleurisy are etiologically associated with pulmonary tuberculosis or tuberculosis of the intrathoracic lymph nodes. Dry pleurisy of tuberculous etiology occurs when the lesions are located subpleurally, break through into the pleural cavity with contamination of the latter, or as a result of hematogenous introduction of pathogens.
Among extrapulmonary processes, dry pleurisy can be complicated by diseases of the digestive system (cholecystitis, pancreatitis, subphrenic abscess), collagenosis (SLE, rheumatism, systemic vasculitis), infections (brucellosis, typhoid and typhus, whooping cough, measles, influenza). In some cases, dry pleurisy is accompanied by eating disorders (cachexia, scurvy), uremia.
The pathogenetic basis of dry pleurisy is the inflammatory reaction of the parietal and visceral pleura, which occurs with hyperemia, edema, and thickening of the pleural layers. The amount of exudate is so insignificant that it is reabsorbed by the pleura with sedimentation of fibrin threads on the surface of the pleura in the form of pleural overlays, making it difficult for the sheets to slide. In the future, this can lead to the formation of massive moorings and limitation of lung mobility.
In most cases, dry pleurisy turns into exudative, but it can resolve without the formation of pleural effusion.
The main symptom of dry pleurisy should be considered acute painful sensations that have become stabbing in nature. They are localized in the side and are forced in the following cases:
- when trying to take deep breaths;
- short cough;
- sneezing.
When the pleural layers become inflamed, symptoms such as:
- chills;
- increased sweating at night;
- severe weakness;
- painful sensations.
- rarely - increased body temperature;
- swelling of the neck veins;
- sometimes - swelling of the skin in the lower parts of the chest may be swollen, its fold is thicker than on the healthy half of the chest.
In addition to pain, there are other manifestations of the disease. These include a dry cough, which occurs due to fibrin irritation of the cough pleural nerve endings, as well as an increase in body temperature.
In 80% of cases, patients with dry pleurisy indicate pain and discomfort in the lower and lateral sternum. Depending on which location is affected, other processes may be involved in the algorithm for the irradiation of symptoms. We are talking about the brachial plexus, the nerve trunks of the upper limbs and the diaphragm.
Typically, dry pleurisy lasts 1-3 weeks and ends with recovery. The transition of dry pleurisy to exudative pleurisy is possible; then the pain decreases and the pleural friction noise disappears. A prolonged or recurrent course indicates active pulmonary tuberculosis.
Left-sided diaphragmatic pleurisy should be differentiated from myocardial infarction. Indeed, in this situation the following symptom complex arises.
- pain in the chest, sometimes behind the sternum;
- dyspepsia;
- pain in the epigastric region;
- rhythm disturbance such as extrasystole or tachyarrhythmia;
- feeling of anxiety and fear.
There are a number of diseases that can occur with symptoms similar to pleurisy:
- intercostal neuralgia;
- intercostal neuromyositis;
- rib fracture;
- epidemic myalgia;
- fibrinous pericarditis;
- angina pectoris;
- myocardial infarction;
- spontaneous pneumothorax;
- peptic ulcer of the stomach and duodenum;
- acute cholecystitis;
- acute appendicitis;
- osteochondrosis of the intervertebral discs of the thoracic region.
A deep knowledge of their symptoms, as well as additional research methods, will help the doctor distinguish dry pleurisy from these diseases.
Regardless of the origin of pleurisy, patients must adhere to medical prescriptions such as:
- bed or semi-bed rest;
- a balanced diet (it is especially important to consume enough proteins, but the consumption of carbohydrates, salts and liquids should be limited);
- anti-inflammatory drugs (in the acute period - intramuscular and intravenous, for residual effects - tablets);
- desensitizing agents;
- in case of severe pain, use painkillers;
- to increase the body's resistance - hyperimmune plasma, polyglobulin and their analogues.
Treatment for secondary pleurisy should be primarily aimed at eliminating the cause of inflammatory changes in the pleura - these are:
- cytostatics for cancer;
- anti-tuberculosis drugs for tuberculosis;
- antibiotics for pneumonia, taking into account the sensitivity of microorganisms;
and so on.
After consulting with your doctor, you can use old, but quite effective methods of traditional medicine:
- warm compress;
- tight bandaging of the lower chest;
- applying iodine strips to the skin of the chest
and so on.
In complex or advanced cases with a pronounced inflammatory process, as well as disturbances in protein and water-salt balance, the following is used:
- hormonal drugs;
- protein preparations;
- electrolyte solutions.
note
The introduction of antibacterial drugs into the pleural cavity is theoretically possible, but as a method for dry pleurisy it has not taken root.
Most often, fibrinous pleurisy in its origin is associated with tuberculosis of the lymph nodes inside the chest or pulmonary tuberculosis. Having a tuberculous origin, dry pleurisy is formed when the lesions are located subpleurally, as well as when they break into the pleural cavity, when it becomes contaminated. It can also develop due to hematogenous introduction of pathogens.
All sorts of nonspecific lung lesions are cited as causes of pleurisy in this situation. These may be bronchiectasis, pneumonia, abscesses, heart attacks or lung cancer.
The pathogenic basis of this disease lies in the inflammatory reactions of the visceral and parietal pleura, which occur with edema, hyperemia, and thickening of the pleural layers. In this case, the amount of exudate will be so insignificant that its reabsorption by the pleura may begin with the settling of fibrin threads on the surface of the pleura. It is formed in the form of characteristic pleural overlays, which significantly complicate the sliding of the leaves.
In the future, this may lead to limited mobility of the lung and the appearance of massive moorings.
Most often, dry pleurisy (especially if left untreated) develops into exudative pleurisy. But in some cases, everything can be resolved without pleural effusion.
When the costal pleura is affected by dry pleurisy, characteristic pain begins in the corresponding half of the chest. To effectively treat dry pleurisy, the symptoms must be familiar to everyone. Then the disease can be quickly identified in order to consult a doctor for appropriate help.
With this pathology, the pain will increase with exhalation, as well as with straining and coughing. All this forces the patient to lie only on the painful side, which significantly limits the mobility of the chest. Any doctor can easily determine the need to begin treatment for dry pleurisy based on the symptoms.
With this disease, during the subsidence of the inflammatory process, a significant decrease in the sensitivity of the nerve endings of the pleura occurs. All this is accompanied by the fact that the pain subsides.
Conservative treatment of dry pulmonary pleurisy is often sufficient. Drug treatment is possible if it is infectious in nature. In this case, antibacterial drugs are prescribed, the choice of which depends on the patient’s sensitivity to a specific antibiotic and the type of pathogen.
Depending on the nature of the pathogenic flora, medications can be in the form of:
- cephalosporins (“Ceftriaxone”, “Mefoxin”, “Latamoxef”, “Keyten”, “Cefepime”, “Cefpirom”, “Ceftolozane”, “Zeftera”);
- penicillins (“Oxamp”, “Sultasin”, “Amoxiclav”);
- glycopeptides (“Targotsid”, “Vancomycin”, “Vibativ”).
Also, drugs in the form of fluoroquinolones, carbapenems, macrolides, aminoglycosides, ansamycins, lincosamides, amphenicols, tetracyclines, and other synthetic antibacterial agents can be used as therapy.
As we have already noted, dry pleurisy often develops into exudative one. In this case, the patient develops both objective and subjective complaints. The latter include a feeling of heaviness in the chest, dry cough, sweating, high fever, and headache.
When treating dry and exudative pleurisy, Traube's space, which had previously practically disappeared, begins to recover. It occurs in the lower chest on the left side.
It is worth noting that the treatment of exudative and dry pleurisy is somewhat similar, although it has some differences.
For example, in the latter case, pathogenetic therapy and evacuation of exudate are required. Etiological treatment consists of influencing the original source of the disease.
Also in the treatment of dry and exudative pleurisy along the wedge. Recommendations advise the use of diet therapy. You should include more proteins and vitamins in your diet, and limit your intake of water and salt. General strengthening gymnastics has a beneficial effect. When the acute manifestations of the disease pass, you can do breathing exercises and light chest massage. It is important to understand that any manipulations should be performed only after consultation with a treating specialist.
Dry pleurisy is usually a complication of painful processes in the lungs or other organs located near the pleural cavity, or serves as a symptom of general (systemic) diseases. Infectious pleurisy is divided according to the type of pathogen, aseptic (non-infectious) - according to the nature of the disease of which it is a manifestation.
Most often, the causes of serous and serous-fibrinous pleurisy are infectious inflammatory diseases of the lungs: tuberculosis, pneumonia (parapneumonic, metapneumonic pleurisy), a limited focus of suppuration of the lung (abscess).
Sometimes dry pleurisy develops as a complication of the active phase of rheumatism or other systemic connective tissue lesions (rheumatic, lupus pleurisy).
It can be very difficult to correctly and timely diagnose the onset of dry pleurisy: pain at the initial stage is either completely absent or insignificant, the temperature, as a rule, remains subfebrile or normal.
But the further development of the disease occurs acutely. Pain in the side appears, and pain intensifies when breathing: when sneezing, coughing, at the height of inspiration, when pressing on the affected area. The pain sometimes radiates to other parts of the body, for example to the abdomen, shoulder, or axillary region. A dry cough also appears with pain, body temperature sometimes shows 38 - 39°, tachycardia and fever are present.
When examining the patient, asymmetry of the chest is detected, on a particular half of the chest there is a bulging of the intercostal spaces, and there is a delay in breathing on the affected side. Above the exudate, the percussion sound is dull, vocal tremor and bronchophony are weakened, breathing is either weak or not audible at all. The upper limit of the effusion is established by percussion, during ultrasound of the pleural cavity or radiography of the lungs.
Dry pleurisy usually ends with complete recovery within 1 to 2 weeks. The temperature returns to normal and the pain disappears. But there is also a prolonged course of the disease, in which adhesions and pleural adhesions develop.
Quite often, dry pleurisy is mistaken for acute myositis, characterized by damage to the intercostal muscles, intercostal neuralgia, angina attack, rib fracture, myocardial infarction (according to ECG data).
With intercostal neuralgia, pain is felt along the nerves with the presence of painful points near the spine. By the way, with neuralgia, the pain, with a tilt of the body, intensifies in the painful side, the opposite happens with pleurisy - the pain intensifies in the healthy side. This is explained by the fact that in the first case the nerve is compressed, and in the second case the pleura is stretched.
How does the disease manifest itself?
Symptoms of pleurisy can be supplemented by manifestations of the underlying lung disease. They may also be the only signs of illness. As a rule, the patient’s condition is satisfactory, so the symptoms of the disease do not significantly affect the body. Temperature indicators are different, since everything depends on the activity of the main inflammatory process in the lung tissues. When the pleural layers become inflamed, symptoms such as:
- chills;
- increased sweating at night;
- severe weakness;
- painful sensations.
Dry pleurisy
Pain
The patient feels pain behind the sternum while breathing. He has a sharp character. Pain intensifies when coughing, inhaling or changing body position. Breathing is characterized by rapidity. In some cases, to alleviate the condition, the patient takes a lying position on the affected side. This is how he manages to reduce pain, since the respiratory movements of the chest are limited.
Incomplete chest mobility
Similar symptoms occur when breathing. If there is no massive inflammation of the lung tissue, then the percussion sound over the damaged area does not change. Decreased breathing is observed if the patient has taken a comfortable position. There is noise above the inflammatory focus, which occurs due to friction of the pleura. Its timbre is similar to the sound of frosty snow.
Manifestations of diaphragmatic dry pleurisy
The presented pathology develops against the background of fibrinous inflammation of the pleura lining the diaphragm. It is impossible to listen to the friction noise of the affected pleura. The pain syndrome can affect the neck and abdomen. Symptoms of diaphragmatic pleurisy are characterized by abdominal tension. It stimulates acute disease of the abdominal organs. The result of this process is painful hiccups and pain when swallowing.
Patients complain of symptoms such as chest breathing and increased pain in the lower part of the sternum during deep inspiration. If you press on the area between the legs of the sternocleidomastoid muscle, painful sensations occur.
Complications
With the development of extrapulmonary dry pleurisy, they can be complicated by diseases of the digestive system. For example, pancreatitis, cholecystitis, subphrenic abscesses.
In some cases, the disease may be complicated by infections (typhoid or typhoid fever, brucellosis, measles, whooping cough, influenza) or collagenosis (rheumatism, systemic lupus erythematosus, systemic vasculitis).
Sometimes dry pleurisy is accompanied by uremia or an eating disorder.
Shortness of breath after treatment of pleurisy, which may indicate the presence of adhesions (shvart) between the layers of the pleura, which limit the mobility of the lungs during breathing.
As a rule, the outcome of the disease is always favorable, but if patients ignore medical prescriptions, it is possible:
- development of adhesive process in the pleural cavity,
- compaction of the pleura,
- education mooring,
- development of pneumosclerosis and subsequent respiratory failure.
A frequent complication of exudative pleurisy is suppuration of fluid in the pleural cavity.
Reasons for development
Dry pleurisy has no independent meaning. Most cases of fibrinous pleurisy are etiologically associated with pulmonary tuberculosis or tuberculosis of the intrathoracic lymph nodes. Dry pleurisy of tuberculous etiology occurs when the lesions are located subpleurally, break through into the pleural cavity with contamination of the latter, or as a result of hematogenous introduction of pathogens. The causes of the development of dry pleurisy are also often nonspecific lung lesions: pneumonia, bronchiectasis, pulmonary infarction, lung abscess, lung cancer.
Among extrapulmonary processes, dry pleurisy can be complicated by diseases of the digestive system (cholecystitis, pancreatitis, subphrenic abscess), collagenosis (SLE, rheumatism, systemic vasculitis), infections (brucellosis, typhoid and typhus, whooping cough, measles, influenza). In some cases, dry pleurisy is accompanied by eating disorders (cachexia, scurvy), uremia.
The pathogenetic basis of dry pleurisy is the inflammatory reaction of the parietal and visceral pleura, which occurs with hyperemia, edema, and thickening of the pleural layers. The amount of exudate is so insignificant that it is reabsorbed by the pleura with sedimentation of fibrin threads on the surface of the pleura in the form of pleural overlays, making it difficult for the sheets to slide. In the future, this can lead to the formation of massive moorings and limitation of lung mobility.
In most cases, dry pleurisy turns into exudative, but it can resolve without the formation of pleural effusion.
Signs of inflammation
You can also learn about the symptoms and treatment of dry pulmonary pleurisy by consulting a pulmonologist. It will not be superfluous to know the characteristic signs of this pathology.
With inflammation of the diaphragmatic pleura, pain is concentrated in the abdominal cavity. In this case, pancreatitis, acute cholecystitis, and appendicitis may appear. With dry apical pleurisy, pain is transferred to the projection of the trapezius muscle, and when the pericardium is involved in inflammation, pleuropericarditis is formed.
What signs of dry pulmonary pleurisy in adults do doctors note? In fibrous pleurisy, the patient can experience general symptoms of almost any inflammation - loss of appetite, malaise, night sweats, as well as a dry cough. At the same time, the body temperature of a patient with such an illness can be either normal or significantly high, reaching 38-39 degrees. The resulting fever is accompanied by tachycardia and chills.
The total duration of the disease is from one to three weeks, depending on the body's response to therapy, the severity and many other associated factors. In this case, the final outcome may be a complete cure or the transition of pleurisy to an exudative form. In some cases, the disease becomes chronic - then it is not possible to completely defeat it until the end of life. In the latter situation, pleurisy lasts several months with periodic exacerbations.
Forecast and prevention of pleurisy
The prognosis for dry pleurisy is generally favorable and depends on the course of the underlying disease.
Prevention of pleural inflammation involves the prevention and effective treatment of diseases complicated by pleurisy.
For early diagnosis of pneumonia and lung abscesses, it is necessary to promptly seek medical help when the first symptoms of respiratory tract inflammation appear. A simple and accessible method for diagnosing these diseases is x-rays of the lungs. Patients should not refuse diagnostic radiography prescribed by a doctor to exclude severe complications.
An effective and affordable method for early diagnosis of tuberculosis is preventive annual fluorography.
The primary prevention of pleurisy is timely prevention and further treatment of major diseases: acute pneumonia, rheumatism, tuberculosis.
It is necessary to increase the body's resistance to various infections, avoid hypothermia and contact with harmful substances. Good nutrition also plays an important role in the prevention of dry pleurisy.
Patients diagnosed with dry pleurisy caused by tuberculosis are subject to mandatory dispensary observation.
Breathing exercises are also recommended for the prevention of adhesions in the pleural cavity.
Prevention of pleurisy includes:
- Timely contact with your doctor for various pathologies/diseases in order to prevent the disease from becoming chronic;
- Compliance with rehabilitation instructions after chest surgery;
- Avoid staying in crowded places during epidemics of influenza, ARVI, acute respiratory infections;
- Compliance with personal hygiene rules;
- Rest regularly, get enough sleep;
- Always ventilate the room you are in;
- Stop smoking and alcohol;
- Avoid hypothermia.
Of course, it is impossible to predict how the body will react to the action of a particular factor. However, anyone can follow simple recommendations for the prevention of pleurisy:
- First of all, complications should not be allowed during the development of acute respiratory infections. To prevent pathogenic microflora from penetrating the mucous membrane of the respiratory tract, and then into the pleural cavity, colds cannot be left to chance!
- If pneumonia is suspected, it is better to take a chest x-ray in a timely manner and begin adequate therapy. Improper treatment of the disease increases the risk of complications in the form of inflammation of the pleura.
- For frequent respiratory tract infections, it is good to change the climate for a while. Sea air is an excellent means of preventing respiratory tract infections, including pleurisy.
- Do breathing exercises. A couple of deep breaths after waking up will serve as an excellent prevention of the development of inflammatory diseases of the respiratory system.
- Try to strengthen your immune system. In the warm season, do hardening, spend more time in the fresh air.
- Stop smoking. Nicotine becomes the first cause of the development of pulmonary tuberculosis, which in turn can provoke inflammation of the pleura.
Classification
In clinical practice, it is customary to distinguish several types of pleurisy, which differ in the nature of the effusion formed in the pleural cavity and, accordingly, in the main clinical manifestations.
- Dry (fibrinous) pleurisy. Develops at the initial stage of inflammatory damage to the pleura. Often at this stage of pathology, there are still no infectious agents in the lung cavity, and the changes that occur are caused by the reactive involvement of blood and lymphatic vessels, as well as an allergic component. Due to an increase in vascular permeability under the influence of pro-inflammatory substances, the liquid component of plasma and some proteins begin to leak into the pleural cavity, among which fibrin is of greatest importance. Under the influence of the environment in the inflammatory focus, fibrin molecules begin to unite and form strong and adhesive threads that are deposited on the surface of the serous membrane.
- Purulent pleurisy. Purulent exudate accumulates between the layers of the serous membrane of the lung. This pathology is extremely severe and is associated with intoxication of the body. Without proper treatment, it poses a threat to the patient's life. Purulent pleurisy can form either due to direct damage to the pleura by infectious agents, or due to the spontaneous opening of an abscess (or other accumulation of pus) of the lung into the pleural cavity. Empyema usually develops in debilitated patients who have serious damage to other organs or systems, as well as in people with reduced immunity.
- Exudative (effusion) pleurisy. It represents the next phase of the development of the disease after dry pleurisy. At this stage, the inflammatory reaction progresses, and the area of the affected serous membrane increases. The activity of enzymes that break down fibrin threads decreases, and pleural pockets begin to form, in which pus can subsequently accumulate. the outflow of lymph collapses, which, against the background of increased fluid secretion (filtration from dilated blood vessels at the site of inflammation), leads to an increase in the volume of intrapleural effusion. This effusion compresses the lower segments of the lung on the affected side, which leads to a decrease in its vital volume. As a result, with massive exudative pleurisy, respiratory failure may develop - a condition that poses an immediate threat to the patient’s life. Since the fluid accumulated in the pleural cavity reduces to some extent the friction between the layers of the pleura, at this stage the irritation of the serous membranes and, accordingly, the intensity of the pain is somewhat reduced.
- Tuberculous pleurisy. It is often placed in a separate category due to the fact that this disease is quite common in medical practice. Tuberculous pleurisy is characterized by a slow, chronic course with the development of a syndrome of general intoxication and signs of damage to the lungs (in rare cases, other organs). The effusion from tuberculous pleurisy contains a large number of lymphocytes. In some cases, this disease is accompanied by the formation of fibrinous pleurisy. When the bronchi melt by an infectious focus in the lungs, specific curdled pus, characteristic of this pathology, can enter the pleural cavity.
This division in most cases is rather arbitrary, since one type of pleurisy can often transform into another. Moreover, dry and exudative (effusion) pleurisy are considered by most pulmonologists as different stages of one pathological process. It is believed that dry pleurisy initially forms, and effusion develops only with further progression of the inflammatory reaction.
Diagnostics
If dry pleurisy is suspected, consultation with specialists is required: phthisiatrician, pulmonologist, gastroenterologist, rheumatologist, infectious disease specialist.
To make a diagnosis, clinical and auscultatory data, ultrasound results of the pleural cavity, and X-ray studies are also necessary.
Auscultatory symptoms of dry pleurisy are weakening of breathing on the affected side, listening to extensive or localized pleural friction noise, which occurs due to the contact of rough pleural layers with each other. It can be subtle and sometimes pronounced. Muscle soreness and stiffness are detected by palpation.
Ultrasound of the pleural cavity is indicated to exclude the presence of exudate.
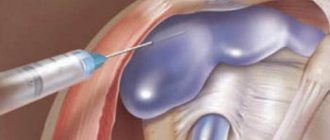
When performing pleural puncture, fluid is removed, the volume and nature of which completely depends on the cause of pleurisy. Bacteriological and cytological studies of pleural exudate make it possible to clarify the etiology of pleurisy. Pleural effusion is marked by a relative density above 1018-1020, again a positive Rivolt reaction, and a variety of cellular elements.
In the blood, an increase in fibrin, ESR, an increase in the values of sialic acids, seromucoids, and neutrophilic leukocytosis are detected.
Also, to determine the cause of pleurisy, thoracoscopy with pleural biopsy is prescribed.
It is worth noting that formal diagnostics to determine dry pleurisy are considered insufficient. The doctor always needs to establish the cause of the disease, and not just eliminate its symptoms. Therefore, if this disease is suspected, the patient should consult with a number of specialists. This is a rheumatologist, pulmonologist, gastroenterologist, phthisiatrician, and infectious disease specialist.
Auscultatory, that is, physical, signs of this disease include a significant weakening of breathing on the affected side, extensive or localized pleural friction noises during auscultation. It is worth noting that pleural friction noise occurs when the rough pleural layers come into direct contact with each other.
Interpretations of complaints, visible manifestations, as well as data from additional examination methods will help the general practitioner establish the correct diagnosis.
Differential diagnosis with pericarditis, coronary insufficiency, intercostal neuralgia, and neuromyositis is necessary. For this purpose, consultations are necessary: with a cardiologist, neurologist, pulmonologist, and sometimes a thoracic surgeon.
Diagnostic methods include:
- Clinical blood test (increased erythrocyte sedimentation rate, neutrophilic leukocytosis with a shift to the left).
- Biochemical blood test (increased amount of seromucoids, fibrin, sialic acids and other acute-phase indicators).
- X-ray examination of the thoracic organs (typical high location of the dome of the diaphragm on the affected side; decreased mobility of the lower edges of the organ during respiration and slight bulging of parts of the pulmonary field).
- Ultrasound (reveals the presence of deposited fibrin layers and thickening of the membrane walls).
A modern way to diagnose processes occurring in the pleural cavity is spiral computed tomography (SCT), as well as magnetic resonance imaging (MRI).
Diagnostic tests
To begin treatment of dry pulmonary pleurisy, various studies are carried out. For example, chest radiography and fluoroscopy show obliteration of the sinuses, limited excursion of the diaphragm on the affected side, as well as changes in its contour or high standing. In particular, the contour of the diaphragm may become atypical - for example, with compactions, irregularities, and bulges.
It is important to differentiate dry pleurisy from myositis, intercostal neuralgia, angina attack, rib fracture, and myocardial infarction. The latter options can be excluded using an electrocardiogram. All of these diseases may have similar symptoms and signs. It is important to establish exactly what problem the patient has and what he should be treated for.
Only a professional doctor can do this based on the results of a full diagnostic examination. So self-medication is strictly prohibited when the first such signs appear. Only a doctor can give you an accurate diagnosis and prescribe effective treatment for dry pleurisy.
It is impossible to determine dry pleurisy using formal diagnostics. Here it is necessary to find out the root cause of the pathology. Therefore, the patient must visit other specialists.
Auscultatory symptoms of the present disease can be recognized by weakened breathing on the damaged side and pleural friction noise. During palpation, it is possible to detect hardness and soreness of the muscles.
According to the results of fluoroscopy, there is a limitation in the excursion of the diaphragm on the damaged side. To exclude the presence of exudate, an ultrasound of the pleural cavity will be required.
An ECG will help to distinguish dry pleurisy from diseases such as intercostal neuralgia, angina pectoris, and myocardial infarction.
Treatment of pleurisy
How to treat pleurisy? Due to the development of pleurisy against the background of other diseases, its course, symptoms, and methods of therapy largely depend on the root cause of the pathological process in the pleura. So, initially the course of treatment is aimed at stopping the primary disease, and the treatment of pleurisy itself is already reduced to improving the course of the pathology - relieving pain, normalizing the outflow of exudate, stopping the infection, normalizing respiratory function, etc.
1. Drug treatment: 1.1. Anti-infective therapy;1.2. Anti-inflammatory therapy;1.3. Detoxification therapy;1.4. Strengthening the immune system; 1.5. Normalization of beneficial intestinal microflora.2. Surgical treatment.3. Diet for pleurisy.
Important! Before using medications, be sure to consult your doctor!
Important! Before using folk remedies for pleurisy, be sure to consult your doctor!
Horseradish. Mix 150 g of dry crushed horseradish root with the juice of 3 lemons. You need to take half a teaspoon 2 times a day, in the morning on an empty stomach and in the evening before bed.
Badger fat. Make a mixture of 250 g of badger fat, 300 g of thorn-free and crushed aloe leaves and a glass of honey. Place the resulting mixture in the oven for 15 minutes to heat, after which you need to strain the product and throw away the remaining raw materials. You need to take this folk remedy for pleurisy 1 tbsp. spoon 3 times a day, 30 minutes before meals.
Depending on the root cause of the disease, etiotropic treatment of the underlying pathological process is carried out.
Bed rest and drinking plenty of fluids are prescribed. Cupping, mustard plasters, and warming compresses are applied to the chest area.
Since the patient is bothered by severe pain and cough, non-narcotic painkillers and antitussives are used. Desensitization therapy is also recommended. If there is a high temperature, paracetamol analogues are prescribed.
The patient needs to undergo breathing exercises. Those who have had pleurisy of unknown etiology must be registered for observation at an anti-tuberculosis dispensary.
Therapeutic measures
Treatment of the presented pathology should take an integrated approach and actively influence the underlying disease. The patient is required to remain in bed. Treatment is carried out with anti-inflammatory medications and antibiotics. Antitussive medications are taken when there is a dry cough, which increases pain in the chest.
To reduce inflammation, treatment includes taking steroid hormones. These include Metypred, Prednisolone, Hydrocortisone.
Drug Metipred
Treatment, including the administration of painkillers intramuscularly, will help reduce severe pain. Traditional treatment is also actively used:
- compresses with a warming effect;
- installation of medical cups;
- applying an iodine mesh to the skin of the damaged area.
If there is no focus of the inflammatory process in the lung tissue, then treatment can be carried out at home. Symptomatic treatment involves using the method of immobilization of the affected half of the chest. For these purposes, use tight bandaging. Patients should drink more fluids, eat well, replenishing their body with vitamins and complete proteins. If the patient’s recovery is evident, then treatment can be supplemented with physiotherapy and therapeutic breathing exercises.
Breathing exercises
Treatment of an uncomplicated form of dry pleurisy lasts several days or 2–3 weeks. With a prolonged recurrent course or transition to exudative pleurisy, one can assert the presence of a tuberculosis process.