Lung abscess - causes (etiology)
There is no specific causative agent of pulmonary suppuration. The etiological factor for lung abscess and the development of a suppurative process in the lungs is a mixed, predominantly coccal flora (streptococci, staphylococci, pneumococci). In some cases, lung abscess is associated with autoinfection with microbes that are saprophytes of the upper respiratory tract. These microbes, once in the lungs, can become pathogenic and cause suppuration of varying nature and prevalence. The development of the suppurative process in the lungs and its intensity depend, in turn, on the reactivity of the lung tissue and the reaction of the whole organism.
Information about the disease
So, a pulmonary abscess can really be called a disease, but in fact it is nothing more than inflammation in the lung tissues, which subsequently leads to their disintegration and the formation of a cavity in the lung filled with rotting products or purulent contents.
An abscess is a strictly limited area of arbitrary size, the volume of which depends on a number of factors, but is often a consequence of the severity of the problem. The walls of this formation are the so-called pyogenic membrane, which is formed from fibrous compounds and granulation tissues.
The most common cause of abscess formation in the lung is advanced or incompletely cured pneumonia. From here comes a reasonable conclusion that abscesses in the lung are formed as a result of certain microorganisms, that is, bacteria are the culprit in the death and suppuration of lung tissue. If we talk about less frequent, but also possible causes of the formation of a pulmonary abscess, then among them are:
- Clogged or persistent mucus;
- Vomit;
- Entry of foreign bodies into the lung;
- Physical damage.
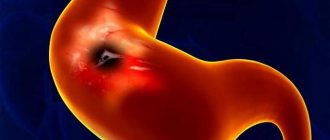
To put it in more understandable language and discard medical terms, a pulmonary abscess is formed due to the melting of lung tissue. At the site of such a lesion, the melting tissue turns into pus, which is isolated in the organ as a kind of capsule. In addition to the problems associated with this process, the greatest risk is the spontaneous opening of an abscess, in which case purulent masses are released, which also promises many problems.
However, under normal conditions, the released pus is sent to the bronchi, and the person begins to have a strong wet cough, which promotes expectoration of products of necrotic origin. Then, scarring and tissue hardening form in the affected area, but all this occurs only in favorable situations.
You must be clearly aware that the formation of an abscess should in no case be left unattended; with such a problem, it is important to be under the supervision of a doctor, in addition, such formations can have a different nature.
Lung abscess - mechanism of occurrence and development (pathogenesis)
The ways in which infection enters the lungs are different. Professor S.I. Spasokukotsky divided pulmonary suppuration into 6 groups:
- embolic;
- obstructive;
- aspiration;
- matapneumonic, arising as an outcome of pneumonia;
- parasitic (echinococcus, actinomycosis);
- traumatic.
Most often, a purulent process in the lungs develops as a result of pneumonia or a complication of bronchiectasis, which accounts for 68% of all pulmonary suppurations. This group of so-called secondary lung abscesses, when the bronchogenic route of infection predominates.
Primary lung abscess usually occurs acutely with injuries to the chest, aspiration of foreign bodies, after surgery on the upper respiratory tract (removal of tonsils, etc.). It is also possible for an abscess to develop by hematogenous or lymphogenous route, when the infection is introduced into the lungs from a distant purulent focus in the body.
Melting of lung tissue (lung abscess) can occur without the participation of microbes. For example, with disintegrating tumors or lung infarctions, a cavity may form as a result of circulatory problems in a certain area. In such cases, necrosis of the lung tissue precedes suppuration.
Diagnostic methods
It is important to take diagnostic measures seriously, the speed of recovery depends on this
For correct diagnosis, it is necessary to use all research methods in combination.
- Blood tests, both general and biochemical, in the event of an abscess will show a higher number of leukocytes than normal.
- Sputum is also taken for analysis to determine the type of pathogen.
- An X-ray method is used to show the condition of the chest, preferably in 2 projections - straight and lateral.
- CT scan
The doctor takes into account all the nuances by examining the x-ray of the lung abscess, and then makes a decision on prescribing the necessary medications.
Lung abscess - symptoms (clinical picture)
In the clinical picture of a lung abscess, two periods are distinguished:
- before opening the abscess;
- after opening the abscess.
The first period, when an abscess forms, has different durations in different cases, but on average lasts 10-12 days. At the onset of the disease, patients complain of general malaise, weakness, chills, cough with scanty sputum, and chest pain. When the lung tissue melts, a fever is observed, at first moderately high, then gradually becoming remitting and then hectic. Even with small abscesses, shortness of breath is noted.
When palpating the chest, in some cases pain is detected along the intercostal spaces on the sore side. This symptom is associated with the involvement of the costal pleura in the process. Perhaps there is a lag in the act of breathing of one half of the chest, corresponding to inflammation. Voice tremors depend on the location of the inflammation. With a peripheral location, vocal tremors are often enhanced, but with a deep location, they are not changed.
With percussion, you can determine the dullness of the percussion sound on the sore side, especially with metapneumonic abscesses. Listening in the initial stages and with deeply located abscesses does not reveal any deviations from the norm. With a more superficially located abscess, breathing over the affected area is vesicular, weakened, sometimes with a bronchial tint. In some cases, hard breathing and scattered dry wheezing are detected.
An important objective criterion in diagnosing a lung abscess is the blood picture. Neutrophilic leukocytosis (15,000-20,000 per 1 mm3) with a shift to the left, and sometimes even to myelocytes, and a significant acceleration of ROE is considered characteristic. A small amount of protein (up to 0.33%) may be detected in the urine.
When the lung tissue melts, examination of the sputum before opening the abscess does not give anything characteristic.
The X-ray picture of an abscess in the first period of the disease is almost no different from ordinary pneumonia or tuberculous infiltrate: a large-focal darkening with uneven edges and unclear contours is determined.
The clinical picture of the second period of lung abscess begins with a breakthrough of the abscess into the bronchus. Between the first and second there may be a transition period, characterized by an increase in the main clinical symptoms (higher fever with large daily fluctuations, severe cough, shortness of breath, chest pain, etc.). A breakthrough of an abscess into the bronchus, with a lung abscess, is accompanied by a sudden copious (mouthful) discharge of purulent and sometimes foul-smelling sputum, which is divided upon standing into 2-3 layers: mucous, serous and purulent. Subsequently, the daily amount of sputum is determined by the size of the cavity and ranges from 200 ml to 1-2 liters.
With a lung abscess, upon examination, the feverish appearance of the patient attracts attention. When the pleura is involved in the process, there is a lag in the diseased half of the chest during breathing. After emptying the cavity of pus, depending on its location and size, physical data may be different. On percussion, with large and superficially located abscesses, tympanitis is determined. Breathing can be harsh (as with an unopened abscess), bronchovesicular or bronchial, and in case of large air-containing cavities with the presence of an efferent bronchus, amphoric. Usually, ringing moist medium- and large-bubble rales are heard in a limited area. If diffuse bronchitis with a large number of wheezing is detected at the same time, this makes it difficult to definitely localize the abscess.
With a lung abscess, leukocytosis with neutrophilia and a shift to the left and acceleration of ROE are observed in the blood. In severe, long-term cases, iron deficiency anemia develops.
Sputum examination provides valuable information. When standing, it is divided into three layers: the upper one is foamy, mucous, the middle one is large, liquid, serous and the lower one is purulent. Microscopic examination of sputum, in addition to a large number of leukocytes and red blood cells, reveals elastic fibers, as well as crystals of cholesterol and fatty acids. The cessation of decay of lung tissue is judged by the absence of elastic fibers in the sputum. The bacterial flora is abundant, often coccal; when treated with antibiotics it becomes scarce.
X-ray examination after emptying the cavity gives a characteristic clearing with a fluid level that varies depending on the position of the patient. If the drainage bronchus is located at the bottom of the cavity, which happens with abscesses of the apex of the lungs, then the fluid level is not determined. This is due to the fact that the entire contents of the cavity drain and are eliminated through the efferent bronchus. When the lung tissue melts, the abscess cavity is surrounded on all sides by a border of inflammatory tissue with a blurred outer contour. With multiple abscesses, several levels are noted.
The clinical course of a lung abscess and its healing depend on the location of the cavity, the possibility of its emptying and associated complications. Most abscesses are cured with the formation of focal pneumosclerosis at the site of the former cavity, but in 30-40% of cases the cure does not occur and they become chronic. Chronic lung diseases (bronchiectasis, pneumosclerosis, lung cancer, etc.) contribute to a prolonged course of suppuration. The following complications of lung abscess are distinguished:
- breakthrough of the abscess into the pleural cavity with the development of pyopneumothorax;
- pulmonary hemorrhage;
- the occurrence of new lung abscesses;
- metastases of abscesses to the brain, liver, spleen and other organs.
- The resulting complications aggravate the clinical course of pulmonary suppuration and worsen the prognosis of the disease.
Complications of ring shadow syndrome on x-ray
Radiographs.
Abscesses of various locations in the pulmonary fields. This syndrome on an x-ray with the destructive destruction of the pulmonary parenchyma by pyogenic (pyogenic) bacteria leads to the following complications:
- Cavern formation.
- Fibrous-cavernous cavities.
- Purulent melting of the lung (empyema).
- Repeated recurrence.
Difficulties in X-ray diagnosis of pathology arise if an abscess is formed due to tuberculosis. The radiologist periodically, upon the direction of the TB specialist, reviews the images of such patients. Difficulties in interpreting the X-ray picture arise in the absence of inflammatory foci around the ring-shaped shadow. Bacteriological examination of sputum comes to the rescue, which allows you to determine the activity of Mycobacterium tuberculosis.
How to distinguish a purulent cavity from a cancerous one
Of great importance in X-ray diagnostics is the difference between inflammatory abscesses and cavities and cancerous analogues. This can be done according to the following criteria:
- with peripheral cancer there are no complete contours of the ring-shaped shadow;
- the cancer cavity has thick tuberous walls and radiant outer contours;
- inflammatory destruction of the lungs is accompanied by fluid levels and perifocal lesions.
Lung abscess - treatment
Treatment of a lung abscess should begin with bed rest in a hospital setting. Patients should receive high-calorie foods with sufficient amounts of proteins and vitamins. In addition, general strengthening measures are necessary: repeated blood transfusions in small portions, 200 ml each, intravenous infusions of glucose, prescription of calcium supplements, etc. Treatment with antibiotics and sulfonamides should be started as early as possible. Sulfonamide drugs must be prescribed in sufficient dosages and for a long time. Antibiotics, in addition to oral and intramuscular use, are administered intratracheally or in the form of an aerosol (1-2 times a day for 2-4 weeks).
Symptomatic treatment for a lung abscess consists of prescribing expectorants and sputum-thinning drugs, bronchodilators (ephedrine, no-spa), etc. In case of a lung abscess, the creation of drainage for better emptying of the cavity is of great importance: the patient must find a position in which sputum drains well , and take it 2-3 times a day for 30-60 minutes.
Physiotherapy for lung abscess has also worked well.
If there is no improvement under the influence of conservative therapy, after 1-2 months the question of surgical intervention should be raised. If the process progresses quickly, especially in the presence of large decay, then surgery is performed after 2-3 weeks. The operation consists of removing a lobe, and in case of multiple abscesses, sometimes the entire lung.
Predisposing factors
Equally important is the knowledge that there are a number of factors that increase the risk of developing a lung abscess.
First of all, the risk group includes people who have diseases that lead to the appearance of purulent formations, we are mainly talking about chronic ailments, for example, this includes diabetes mellitus.
People suffering from alcoholism are also at risk. However, we are not talking now about the deterioration of the body’s immune properties, although this point also cannot be eliminated. In fact, everything is simpler - with alcoholism, the likelihood of aspiration of vomit into the lungs increases, and we have already said that this factor may well contribute to infection and the occurrence of a purulent abscess.
In addition, you need to take pneumonia of any severity very seriously, since even a mild form of pneumonia, with inadequate treatment, increases the risk of complications in the form of abscess formation.
Classification
Depending on the duration of the disease, lung abscess can be acute or chronic. In the first case, ulcers appear within 3-6 weeks after the onset of the disease. In chronic abscess, foci of necrosis form slowly.
Based on its origin, the disease is classified into groups:
- along the route of infection - hematogenous, traumatic, bronchogenic;
- by pathogen - staphylococcal, pneumococcal and others.
According to the localization in the tissues, the pathological process can be single or multiple, unilateral (abscess of the right or left lung) or bilateral, central and peripheral.