Vasomotor rhinitis is a disease during which the nasal cavity begins to narrow quite strongly. Because of this, a person’s breathing worsens and the tone of the vessels of the nasal mucosa is disrupted. When the first symptoms appear, it is necessary to immediately begin treatment for this disease. However, not everyone knows how to treat vasomotor rhinitis. To understand the treatment of this disease, you need to understand what vasomotor rhinitis is and what ways you can get rid of it.
Reasons for development
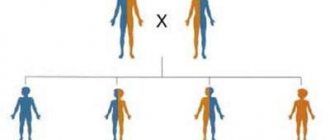
Depending on the cause of the disease, vasomotor rhinitis is distinguished between neurovegetative and allergic.
Also, special mention should be made of this type of rhinitis in pregnant women. Most often, vasomotor rhinitis is caused by impaired excitability of parts of the autonomic nervous system, as a result of which the membranes of the nasal cavity cannot respond normally to various stimuli. As a result, a reaction of hyperactivity of the neurovegetative system and vessels of the nasal cavity develops, which is clinically manifested by an increase in secretory functions and tissue swelling in response to exposure to irritants.
Predisposing factors for the development of vasomotor rhinitis include the following conditions:
- chronic diseases of the ENT organs;
- anomalies in the structure of the nasal cavity;
- curvature of the nasal septum due to previous nasal injuries, fractures, blows;
- prolonged and uncontrolled use of certain intranasal medications - drops such as Farmazolin, Naphthyzin, Oxymetazoline, when used for more than 5 days, are addictive and contribute to severe drying of the mucous membranes of the nasal cavity;
- smoking, including passive smoking;
- constant inhalation of dust or small particles - often found among workers in industrial enterprises;
- disturbance of the psycho-emotional background - people in a state of chronic stress often suffer from vasomotor rhinitis;
- staying in a room with dry air, especially during heating periods.
The main reason for the development of vasomotor rhinitis in pregnant women is hormonal changes in the body. In this case, there is no need to treat rhinitis; from about the 2nd-3rd trimester, the uncomfortable symptoms will go away on their own. In some women, vasomotor rhinitis goes away only after childbirth.
Cautions in treatment
It should be noted that vasomotor rhinitis can lead to serious complications. As a result of constant nasal congestion, the development of concomitant diseases is possible: otitis media, acute rhinitis, sinusitis, including purulent one. Disturbances in the functioning of the respiratory system can lead to the development of hypoxia - oxygen starvation of the brain.
Self-treatment often provokes the disease to become chronic. At the same time, you should not indiscriminately use hormonal drugs or vasoconstrictors - this will only lead to a worsening of the condition. If you have a persistent runny nose, you should consult a doctor for a thorough examination. A correctly established diagnosis and timely prescribed course of therapy is the key to a quick recovery.
Main stages of the disease
The disease has 4 main stages:
- Periodic attacks.
- Constant signs.
- Polyp formation.
- Changes in the structure of the nasal mucosa.
At the initial stage, the disease looks like a runny nose caused by a cold. Symptoms occur intermittently, it is not always possible to establish the causes, and treatment for this reason is sometimes ineffective.
As the disease progresses, attacks in the form of congestion and mucus secretion become more frequent. Due to poor circulation in the vascular tangles of the nasal mucosa, persistent swelling occurs and the risk of polyps increases.
At an advanced stage, the mechanism of pathological changes in the tissues of the nasal mucosa is triggered, they become denser and grow. Headaches occur, the sense of smell disappears, immunity decreases, and the body becomes more susceptible to infectious diseases of the respiratory tract.
Complications may occur in the form of otitis media, pharyngitis, heart failure, and bronchitis. If you experience hoarse breathing, a cough, and you feel discomfort in your heart due to oxygen deprivation, then a visit to the doctor should be made immediately.
What are the vasomotor symptoms of menopause?
Menopause symptoms can significantly impact a woman's quality of life, with the vast majority of women experiencing vasomotor symptoms of some sort as they go through menopause.
Additional definitions of vasomotor symptoms include:
- Hot flashes: a sudden feeling of warmth that affects the chest, neck and face.
- Night sweats: A woman may wake up and experience extreme sweating episodes where her clothes and sometimes bedding are soaked in sweat.
Vasomotor symptoms may cause a woman to experience anxiety and heart palpitations.
Forms
Depending on the predominant etiological factor, two forms of vasomotor rhinitis are distinguished - neurovegetative and allergic. The neurovegetative form usually occurs against the background of neurocirculatory dysfunction. With allergic vasomotor rhinitis, in turn, year-round and seasonal varieties are differentiated.
According to the severity of symptoms:
- mild – only local symptoms are present, and the patient’s general health remains satisfactory;
- moderate severity – moderate asthenic manifestations and limitation of the patient’s activity during the daytime;
- severe – characterized by frequent long-term exacerbations and a decrease in the patient’s ability to work.
The frequency of attacks is also important when selecting a therapeutic strategy, therefore, in clinical practice, intermittent vasomotor rhinitis is differentiated from persistent. In the first case, exacerbations occur no more than 3-4 times a week, in the second, paroxysmal attacks are repeated almost every day.
A common cause of vasomotor rhinitis is long-term uncontrolled use of nasal vasoconstrictors and other medications that affect the processes of regulation of vascular tone.
Fleming's ointment
Ointment based on calendula, game hazel, aesculus. Effectively reduces the symptoms of inflammation and has a bactericidal effect.
The ointment heals the mucous membrane, improves blood supply and improves immunity.
The drug should be placed into the nasal passages with turunda and kept for up to ten minutes. Repeat three times a day for two weeks.
Complete disappearance of all symptoms of vasomotor rhinitis most often occurs after ten days of use.
No adverse reactions were observed.
The drug is approved for use by pregnant women.
Anna Sadovaya, 37 years old. “For some time I used Fleming’s ointment for hemorrhoids, and recently I learned about its effectiveness for the treatment of vasomotor rhinitis.
I tried it and it surprisingly worked.”
Definition of disease
Vasomotor rhinitis is a pathology in which, due to impaired tone of local vessels, swelling develops and breathing through the nose is impaired.
The appearance of the disease is not associated with infection of the mucous membrane by bacterial microflora.
The following factors can provoke swelling of tissues in the nasal cavities:
- allergic reactions to food, medications;
- exposure to cold;
- strong odors, sunlight;
- endocrine disorders.
In some cases, it is not possible to determine the cause of vasomotor rhinitis. Often this disease develops against the background of dysfunction of the autonomic nervous system, which increases the volume of blood in the vessels.
The following symptoms indicate vasomotor rhinitis:
- nasal congestion (mostly temporary and occurs on one or both sides);
- copious mucous or watery discharge from the nose;
- penetration of mucus into the pharynx along the back wall;
- change in voice timbre (nasality);
- impairment of olfactory function;
- frequent sneezing.
Vasomotor rhinitis is typical for people over 20 years of age. Women of this age are at increased risk.
Read the link to see how to treat hypertrophic rhinitis.
Symptoms of the disease are difficult to distinguish from signs of infectious sinusitis or sinusitis, which makes it difficult to make a correct diagnosis. These include:
- Periodically occurring nasal congestion.
- Sneezing and itching.
- Fatigue.
- Watery mucus discharge from the nose.
- Headache.
Vasomotor rhinitis occurs when the proper functioning of the blood vessels of the nasal cavity is disrupted. As a result of disturbances in vascular tone and their increased blood supply, swelling of the mucous membrane occurs.
Main symptoms in adults:
- constant or periodic alternating nasal congestion (the symptom is more pronounced during rest, when a person takes a horizontal position);
- general malaise, weakness;
- a person is tormented by copious, moderate or scanty mucous discharge from the nose;
- There may be a burning and itching sensation in the sinuses;
- feeling of fullness in the nasal cavity;
- constant or periodic sneezing (sometimes it occurs suddenly and also suddenly stops).
A sign of vasomotor rhinitis is difficulty breathing through the nose when lying on your back. Difficulty breathing in a position on the side is also characteristic; the lower half of the nose does not breathe. The disease may be indicated by snoring, poor sense of smell, frequent pharyngitis, tracheitis, laryngitis.
| Allergic | Symptoms of allergic vasomotor rhinitis are formed when the mucous membrane of the nasal passages comes into contact with an allergen. The pathology is characterized by the sudden onset of symptoms:
|
| Neurovegetative | The clinical picture is characterized by:
Symptoms in this case increase during the next attack. Patients experience unbearable itching, headache and a feeling of pressure. Such attacks occur suddenly and disappear after 2-3 hours. |
With a long-term chronic course, vasomotor rhinitis also disrupts general well-being, causing irritability, increased fatigue, insomnia, headaches and other symptoms of trouble in the nervous system.
Triggering factors of the disease
It has been noticed that an exacerbation of the symptoms of the disease occurs after a cold or a common infectious runny nose. Almost all patients experience sneezing, runny nose and congestion when going out into cold air.
You can also identify a number of other factors that contribute to the exacerbation of new attacks of vasomotor rhinitis:
- passive and active smoking;
- alcohol consumption;
- strong aromas;
- dust;
- taking medications;
- stress;
- polluted air in cities with developed industry;
- dirty air at work;
- spicy or hot dishes;
- a sharp change in air temperature after leaving the bathhouse or sauna.
How to treat vasomotor rhinitis
Vasomotor rhinitis is not so easy to cure - therapy will be complex and quite long. First of all, you need to follow the following recommendations from experts:
- Eliminate/exclude all provoking factors that lead to the development of vasomotor rhinitis. It is understood that the patient must stop drinking alcoholic beverages, smoking, and avoid inhaling strong odors.
- Complete a full course of treatment for chronic stomach diseases - gastritis, gastroesophageal reflux and others.
- Elimination of abnormalities in the structure of the nose. Doctors will perform a series of surgical operations to help restore the normal structure of the nose. If it is precisely such anomalies that are the cause of the development of vasomotor rhinitis, then without eliminating them, the disease in question cannot be cured with any, even the most powerful, medications.
- It is worth doing physical exercise, but such loads should be moderate. Running, race walking, swimming in the pool and even basic morning exercises will help correct the functioning of the autonomic nervous system.
- Every day you need to take a contrast shower. Naturally, you first need to obtain permission to perform this procedure from your attending physician.
For a person diagnosed with vasomotor rhinitis, treatment with folk remedies is indicated if the disease is mild and there are no contraindications.
Methods of alternative therapy include taking herbal decoctions, rinsing the nasal cavity, special massage, etc. It is important to take an infusion of herbs and carry out all procedures systematically, over a long period of time, since traditional healing methods have a cumulative effect.
For vasomotor rhinitis, treatment at home should be aimed at eliminating the cause of the disease and its symptoms.
If you approach the matter wisely, then home remedies will only bring benefits and speed up recovery.
Antihistamines
If the cause of vasomotor rhinitis is an allergic reaction, medications with antihistamine action should be used in the treatment of the disease.
To completely get rid of the symptoms of the disease, you should stop the person’s contact with the provoking factor. The cause of the allergy may be:
- wool, dust, pollen, fluff;
- pungent odors;
- cosmetics, household chemicals;
- medications;
- Food.
Drops for vasomotor rhinitis are aimed at reducing the severity of allergy symptoms by blocking the release of biologically active components.
Levocabastine
The active ingredient Levocabastine is included in Tizin Alergy and many other drugs. It blocks receptors that are sensitive to histamine. As a result, swelling of the mucous membrane, rhinorrhea, nasal congestion are reduced, and nasal breathing is facilitated. Clinically, you can also notice a decrease in the severity of itching and the volume of discharge. The local effect after nasal instillation develops after 5 minutes and lasts up to 11 hours. Partial absorption of the drug into the general bloodstream does not cause systemic reactions.
Before instilling the drug, it is necessary to clean the nasal passages with saline solution. Patients over six years of age are prescribed two doses twice a day. By agreement with your doctor, the frequency of use can be increased to four.
If after three days from the start of therapy the symptoms do not decrease, you should consult your doctor. The duration of the therapeutic course is 4 weeks.
Levocabastine should be prescribed with caution to people with renal dysfunction. If the color of the solution changes, you must stop using it. If the recommended doses are exceeded, drowsiness and other nervous system disorders may occur. In this regard, you should not engage in hazardous activities (driving vehicles). Contraindications include hypersensitivity and lactation period. Restrictions also apply to pregnancy.
During the period of gestation, treatment with Levocabastine is permitted only after balancing the risk for the embryo and the benefit for the woman. Breastfeeding should be stopped during therapy.
After using the drops, in rare cases, headache, dizziness, and changes in psycho-emotional state in the form of irritability are observed. Local adverse reactions include dryness, painful, burning sensations and soreness in the nasopharynx. Rashes may appear on the skin. Nausea, tachycardia, muscle pain and cough are also possible.
When Levocabastine and drugs based on oxymetazoline (Nazivin) are administered together, a slowdown in the absorption of the antihistamine is observed.
Other antihistamines
In addition to Tizin Alergy, other equally effective nasal drops can be prescribed:
- Cromohexal;
- Cromoghlin;
- Sanorin Analergin;
- Allergodil.
In addition to medications with local action, tablet forms of antihistamines are required.
Vasomotor rhinitis in children
In young children, vasomotor rhinitis often accompanies allergic conditions and ENT diseases. In particular, there is a direct connection between the incidence of vasomotor rhinitis and adenoiditis, inflammation of the paranasal sinuses, deviated nasal septums and other pathologies of the ENT organs. After eliminating the underlying disease, vasomotor rhinitis in children usually resolves on its own.
Vasomotor rhinitis is especially dangerous for infants. Nasal congestion leads to loss of energy, breast refusal and increases the risk of respiratory arrest. With partial nasal congestion, the possibility of breastfeeding remains, but sucking movements require serious effort from the baby. Fatigue and frequent regurgitation prevent children from getting enough nutrients, which can cause babies to lag in growth and development.
The neurovegetative form of vasomotor rhinitis in young children is less common than the allergic one, however, with a general tendency to autonomic neuroses, there is a risk of developing the disease due to chronic stress. In adolescents, the onset of vasomotor rhinitis may be associated with a sharp change in hormonal levels.
In pediatrics, the following drugs are used to treat rhinitis:
- Vasoconstrictor drops.
Vasoconstrictor drops for children - Herbal medicines with essential oils.
- Antihistamines.
- Glucocorticosteroid nasal drops.
- Drugs that improve blood flow to the brain.
The peculiarity of the course of the disease in children is that it progresses relatively quickly, symptoms increase, and the child’s condition worsens.
When carrying out therapy, much depends on the age of the patient, since some drugs have age restrictions:
- vasoconstrictor nasal drops are not used to treat children under 6 months of age;
- glucocorticosteroids and hormones are not used to treat children under 2 years of age, but the dosage is determined individually;
- nasal drops based on extracts of essential oils are prescribed to patients of different ages, but with caution, since there is a high risk of developing allergies (against which the unpleasant symptoms will only intensify).
You can rinse your child's nasal passages with saline solution or use drops of sea water on a regular basis; they will help normalize the condition of the nasal mucosa.
When vasomotor rhinitis in a child has developed against the background of neurological disorders, Pantocalcin and/or Glycine may be prescribed; Vinpocetine is less commonly prescribed.
But these medications are taken in a certain dosage; they are prescribed by a neurologist if there is a disturbance in blood flow to the brain and the main symptoms of VSD.
The drugs used to treat vasomotor rhinitis have different directions. For this reason, their selection should be done by a doctor. Otherwise, the effectiveness of treatment is called into question, various problems may arise, against the background of which the patient’s condition will worsen, and complications will appear.
Drops for vasomotor rhinitis: review of the best
Swelling of the nasal mucosa, affecting almost all sinuses and manifested without pronounced symptoms of other ENT pathologies, is commonly called vasomotor rhinitis.
Such a disease has the character of a long and gradually developing illness, which can flow from the form of mild nasal congestion to an extremely severe and unpleasant runny nose, significantly worsening a person’s quality of life. As a rule, with timely and properly organized therapy, vasomotor rhinitis does not pose a particular danger and is completely controlled by medications, mainly nasal drops. In rare, particularly advanced cases, it is necessary to resort to surgical intervention. We will not cover the latter in today’s article, but we will pay close attention to conservative methods of treating rhinitis using drops. Interesting? Then be sure to read the material below to the end.
Drug treatment of vasomotor rhinitis
Sometimes folk remedies do not have the proper therapeutic effect. In this case, consultation with an otolaryngologist is necessary.
At the appointment, the doctor will carefully examine the nasal cavity, prescribe laboratory tests, study painful symptoms, and treatment will be carried out with correctly selected medications.
The most effective drugs for the treatment of this disease are nasal sprays with glucocorticosteroids (hormones), such as Nasonex, Avamis, etc. The big advantage of these hormonal sprays is that they are not absorbed into the blood, but have a local anti-inflammatory effect directly on the nasal mucosa .
Both drug treatment of vasomotor rhinitis and traditional therapy are carried out exclusively after consultation with a doctor. Only a specialist will competently select medications and advise on indications and contraindications for the use of traditional medicine.
Home remedies serve as an effective addition to taking medications, allow you to get by with a smaller dose of medications taken under the supervision of a doctor, and shorten the duration of the disease, which is why traditional recipes are so common among patients.
Diagnostics
Before treatment, it is necessary to diagnose vasomotor rhinitis. Making a correct and accurate diagnosis is quite simple. Sometimes it is enough to simply interview the patient and find out exactly when the first symptoms began to appear. However, in most cases, for a final diagnosis you need to take a referral from your doctor and undergo some diagnostic tests:
- a study of nasal flora carried out in a hospital to exclude an infectious form of the disease;
- rhinoscopy, during which the nasal cavity is completely examined to assess the condition of the mucous membrane and check the size of the nasal turbinates;
- general examination, which takes place under the supervision of the attending physician.
Complications
Dangerous complications of neurovegetative rhinitis are:
- Dyspnea;
- Hypoxia of body tissues as a result of insufficient oxygen supply to the blood;
- Inflammatory lung diseases;
- Asthma;
- Chronical bronchitis;
- Nasal polyps;
- Degenerative changes in the tissues of the nasal cavity.
Vasomotor rhinitis significantly worsens the patient’s quality of life, therefore, if a runny nose that does not go away for a long time, not associated with a viral infection, the patient is recommended to consult an otolaryngologist.
Clinical picture
The symptoms of the disease will be the same for both the neurovegetative and allergic forms.
So, the symptoms of chronic vasomotor rhinitis:
- Nasal congestion.
- Sudden attacks of itchy nose and sneezing.
- Copious mucous clear discharge from the nose.
- Headache, heaviness in the bridge of the nose.
- Insomnia.
- Fatigue, weakness, deterioration in performance.
Body temperature in the chronic form of vasomotor rhinitis is practically never elevated. Nasal congestion often goes away on its own if you change your body position, or at night without the use of any medications. Against this background, many people feel healthy.
Medicines
Sanitation of the nasal passages can bring the moment of recovery closer. Rinsing the nose with saline solutions helps relieve swelling and normalize vascular tone. After treatment, the amount of mucus is significantly reduced, and the cilia of the epithelium contribute to the rapid removal of residual secretions.
For rinsing, you can use regular pharmacy saline solution or Aqua Maris spray. At home, a healing liquid can be prepared by mixing sea salt with clean water. The salt concentration should be 0.9% (9 g of table salt per 1 liter of water). Sanitation should be performed several times a day. For this purpose, a syringe, pipette, or enema is used. Upon completion of cleaning the nasal cavities, it is recommended to instill the prescribed medications.
The drug is prescribed only after the etiology of rhinitis has been clarified. Depending on what diagnosis is established, the following is prescribed:
- Glucocorticoid drugs of local and general action. The products have antiallergic and anti-inflammatory effects. This variety includes drops Nasobek, Nasonex, Budesonide, Desrinit, Flixonase. Diprospan injections are prescribed, the patient’s well-being improves quite quickly.
- Antihistamines. They block the body’s reaction to allergens, reduce swelling of the mucous membrane, and normalize airway patency. This is Allergodil, Reactin, Tizin spray.
- Homeopathy. Therapeutic agents have anti-inflammatory, protective and vasoconstrictor effects. Among the popular drugs are Delufen, Euphorbium Compositum, and Fleming's ointment.
- Combined formulations. They have a wide spectrum of action; they can be used to eliminate acute symptoms of allergic manifestations. The most effective drops are Sanorin, Vibrocil, Rinofluimucil, Avamis, Tafen Nasal, Sinupret, Polydexa with phenylephrine.
- Angioprotective drugs. Used to reduce permeability and swelling of capillaries. The product of this group is the biological additive Dihydroquercetin.
- Modern herbal preparations. They have anti-inflammatory and antimicrobial properties. Available as a spray, for example, Pinosol.
The above products are presented in various forms of release. Not only drops and sprays that have a targeted effect can help in the fight against the disease. In some situations, pills or injections help a lot.
In advanced cases, treatment with novocaine may be prescribed. The blockade helps the patient get rid of the annoying runny nose.
There are several classes of medications that are prescribed to patients for vasomotor rhinitis:
- These are antihistamines that have an antiallergic effect.
- Anti-inflammatory drugs, which include glucocorticosteroids.
- Vasoconstrictor drugs that can restore the condition of the nasal mucosa.
- Herbal medicines that have a homeopathic effect.
The treatment is complex, it is most effective, since it allows you to influence the root cause of the disease and the unpleasant symptoms that arise.
The doctor may prescribe:
- agents that dilate blood vessels and improve blood flow to the brain;
- medications for vegetative-vascular dystonia;
- nootropic drugs that improve brain activity.
Medicines can be in the form of tablets, drops, nasal sprays and even inhalation solutions.
Drops
There are several drugs that are prescribed to patients with vasomotor rhinitis:
- Naphthyzin.
A modern drug that is most often used first - Children's Nazivin.
- Xymelin.
These drops act directly on the mucous membrane. They help normalize its condition, narrow blood vessels and relieve nasal congestion. But the peculiarity of therapy is that vasoconstrictor drugs are not used on an ongoing basis to treat this disease.
The fact is that the drops will help stop an attack and relieve an acute runny nose, but they do not affect the root cause of the pathological condition.
For this reason, drops are used to a limited extent, that is, only on those days when pronounced signs of vasomotor rhinitis appear.
To normalize the respiratory process, you can use vasoconstrictor drops for 3 days. Further treatment with the use of such drugs will only worsen the patient’s condition and cause swelling of the mucous membrane.
Sprays
They also prescribe medications that have an anti-inflammatory effect; they include glucocorticosteroids; they help stop the inflammatory process.
Most often, doctors recommend using:
- Aldecin;
Modern spray for quick relief of congestion - Nasonex;
- Nasobek.
These products are available both in the form of sprays and drops; they contain hormones, for this reason they help cope with both allergies and inflammation.
The disadvantage of using such medications is their limited effectiveness. They can be part of combination therapy, but when treatment is carried out using only these drops or sprays, certain problems arise.
During therapy, the patient's condition improves and he feels normal. But as soon as the course is completed, the effect of glucocorticosteroids gradually fades away. Therefore, such therapy is relatively effective.
In addition, this class of medications has a number of contraindications, and in some cases their use is not recommended.
But if the patient did not experience any contraindications or side effects during treatment, then such drops or sprays can be used on a long-term basis. Several courses of treatment can be carried out per year with minor breaks. Derinat nasal drops are also an effective treatment for vasomotor rhinitis.
Galazolin
Particular attention should be paid to the nasal gel Galazolin - it has a vasoconstrictor effect and is widely used in pre-urban practice for the treatment of allergic and vasomotor rhinitis.
Modern spray for quick results
This medicine for the runny nose in adults reduces swelling of the mucous membrane, in a short period of time helps to normalize the amount of mucus secreted and relieve nasal congestion.
Otolaryngologists often prescribe this drug, the reason being that during an acute attack of the disease, the gel helps to quickly normalize the patient’s condition.
Physiotherapy
Physiotherapy is used as an additional treatment method in combination with other drugs. The use of this method has shown high efficiency.
Physiotherapeutic procedures for vasomotor rhinitis:
- phonophoresis with hormonal drugs - the use of ultrasound on the cells of the mucous membrane of the nasal cavity and nasal vessels, normalizes vascular tone, restores damaged mucous membrane and the functioning of mucous glands and cilia, the most effective method of physiotherapy.
- electrophoresis with calcium chloride – strengthens the wall of blood vessels, increases their tone and resistance, relieves swelling, and helps normalize the function of the venous plexuses.
- laser therapy - relieves swelling of the mucous membrane, normalizes local mechanisms for regulating vascular tone, most effective in relation to arterioles and venules.
Physical procedures are carried out daily for 10 – 12 days.
Corticosteroids
Steroid-based medications are widely used for runny nose in severe cases. They have a powerful anti-inflammatory, antihistamine and decongestant effect. In the treatment of chronic vasomotor rhinitis, hormonal agents are an essential component of therapy. Self-administration of glucocorticosteroids is not recommended.
Among the common drugs we highlight:
Long-term use of hormonal drugs in large doses is fraught with local immunosuppression, thinning of the mucous membrane and addiction.
The drug belongs to synthetic drugs with hormonal activity. Its action is aimed at suppressing the inflammatory process, blocking the allergic reaction and alleviating the general condition by restoring nasal breathing.
The effect is to reduce tissue edema and gland secretion. Aldecine is prescribed for hay fever and year-round rhinitis of allergic origin. A special therapeutic effect was noticed for vasomotor rhinitis.
Contraindications include:
- systemic infection of bacterial, fungal, viral type;
- frequent nasal bleeding;
- latent period of tuberculosis;
- hemorrhagic diathesis;
- surgical interventions or injuries of the nasopharynx over the past six months;
- hypersensitivity to the components of the drug;
- children up to six years of age.
The issue of using steroids for pregnant women is decided only by a doctor after assessing the severity of the disease and the woman’s condition. The dosage is 1-2 doses up to four times a day. After achieving a therapeutic effect, the drug is discontinued gradually.
Among the adverse reactions we highlight:
- individual intolerance;
- hives;
- bronchospasm;
- hoarseness;
- increased intraocular pressure;
- sneezing;
- burning sensation in the nasopharynx;
- bloody runny nose;
- ulcerative lesions of the nasopharyngeal mucosa;
- headache;
- decreased sense of smell;
- dry mouth.
A serious complication of hormonal therapy is perforation of the septum and activation of a fungal infection, which is quite difficult to cope with.
The therapeutic effect develops three days after the start of treatment with corticosteroids.
The effect of medications can be enhanced with the help of physiotherapeutic procedures, for example, ultraviolet irradiation, UHF, laser therapy. They stabilize the tone of blood vessels and improve metabolic processes. Usually 5-10 procedures are prescribed.
Do not forget about strengthening the immune system, the strength of which determines not only the success in the treatment of vasomotor rhinitis, but also the overall health of a person.
Lifestyle
To normalize vascular tone, it is necessary to lead a healthy lifestyle and diet:
- Hardening is the best way to tone and train blood vessels. It must be started in the summer with a gradual decrease in the temperature of the water for washing, bathing, and dousing.
- Physical activity stimulates blood vessels, prevents the development of hypertension, obesity, and vegetative-vascular disorders. It is best to do cardio exercises (running, cycling, race walking, dancing, jumping in place, etc.).
- Healthy sleep – an adult should sleep at least 8 hours at night.
- Walks in the open air.
- The normal emotional state is “nerve cells are not recovering”, it is better not to be nervous.
- Quitting smoking and alcohol will not only help strengthen blood vessels, but will also be beneficial for the heart, lungs, liver and the entire body as a whole.
- Body weight support. Sudden changes in body weight, plus or minus kilograms, can also disrupt vascular tone.
- Proper nutrition with the exception of foods containing high amounts of cholesterol. The diet should be balanced, containing a sufficient amount of calcium and other microelements, vitamins B, A, E, and C, polyunsaturated amino acids. Foods that contribute to the strengthening of blood vessels: Fish and other seafood - contain a large amount of polyunsaturated amino acids and microelements.
- Vegetables: beets, cabbage, eggplant, green vegetables, carrots, tomatoes and others.
- Fruits: citrus fruits, apples, banana, grapes and others.
- Berries: currants, raspberries, pumpkin and others.
- Legumes.
- Juices, fruit drinks.
- Gelatin, marshmallow.
- The temperature of food and drinks should be comfortable and warm. Cold and hot food provokes dilation of the vessels of the nasal cavity.
Causes
Doctors say the causes of vasomotor symptoms during menopause are unknown. But the absence of certain hormones can have an impact. They believe this makes the hypothalamus, or the part of the brain that regulates temperature, more sensitive to changes in a woman's body temperature.
Even a very slight increase in body temperature can cause a fever. Researchers are unclear why some women experience them and others don't, or why hot flashes vary in severity.
Over time, the fever begins to subside and may eventually disappear completely. Few women experience periodic hot flashes for the rest of their lives.
Surgery
In the absence of effect from conservative measures for vasomotor rhinitis, surgical treatment is successfully used. Depending on the specific clinical picture of the disease and the general condition of the patient, submucosal vasotomy of the inferior turbinates, ultrasound or microwave disintegration of the inferior turbinates, as well as their laser or radio wave destruction can be used.
In some cases, surgical interventions have to be repeated. The ineffectiveness of the above surgical intervention techniques is an indication for a gentle lower conchotomy. Often, surgical operations on the nasal turbinates are combined with septoplasty, adenotomy, and endoscopic correction of intranasal structures.
Prevention
Preventive measures help prevent the disease in an adult or its transition to a chronic course. If symptoms have just appeared, then prevention can suppress their development and avoid complex treatment in the future. To prevent vasomotor rhinitis you need:
- Avoid nasopharyngeal diseases and treat them promptly
- Get enough sleep
- Periodically breathe fresh air and be outside
- Temper yourself
If you do not monitor the health of your nose, the development of vasomotor rhinitis in adults will be inevitable, and since it is a chronic pathology, a complete cure after this is almost impossible.
Forecast
The prognosis is relatively favorable in young and middle age, worsening with age-related changes in the human vascular system. In most cases, lifestyle changes help alleviate the symptoms of vasomotor rhinitis or get rid of them completely. The disease can occur again with the next appearance of an irritating factor, a large stress load, or with a deterioration in the general condition of the cardiovascular system.
Without changes in lifestyle and treatment procedures, vasomotor rhinitis tends to progress.
Symptoms
There are quite a few different symptoms of vasomotor rhinitis. It is necessary to familiarize yourself with them in advance, since symptoms and treatment in adults and children are interrelated. If you do not know the main signs of vasomotor rhinitis, then it will be quite difficult to treat it. The main symptoms of vasomotor rhinitis include various psychosomatic problems:
- general weakness;
- poor appetite;
- high fatigue;
- sleep problems;
- memory impairment;
- severe dizziness.
Also, the course of vasomotor rhinitis may be accompanied by other dangerous symptoms:
- congestion in one of the nostrils;
- coughing;
- when patients lie on their side, there is a feeling of nasal congestion on the side on which they lie;
- mucous and clear nasal discharge, which can sometimes be purulent;
- accumulation of mucus in the throat.