Focal pneumonia is an inflammatory-infectious disease that does not affect all of the lung tissue, but only a certain area of it. In this case, the formation of small-focal or large-focal inflammation occurs in the lobules of the lung. Pathology can be either independent or secondary. In the first case, the source is pathogenic bacteria, and in the second - the occurrence of other ailments that negatively affect the tissues of this organ.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Complications
- Prevention and prognosis
The symptoms of the disease are nonspecific, i.e., characteristic of quite a large number of other diseases, which greatly complicates the establishment of a correct diagnosis. The main symptoms are often chest pain, cough, dry or with sputum, as well as fever and chills.
Diagnosis of focal pneumonia requires an integrated approach and is based on data from laboratory and instrumental measures. Treatment tactics are often conservative and include medication, physiotherapy and massage.
Etiology
Acute focal pneumonia most often acts as a complication that develops against the background of a severe course or complete lack of treatment for another pathology. In such situations, the formation of an inflammatory process may be caused by the following ailments:
- myocardial infarction;
- acquired, less often congenital heart defects;
- bronchitis and ARVI;
- malignant or benign tumors;
- measles and whooping cough;
- meningitis and scarlet fever;
- acute catarrh of the respiratory tract;
- furunculosis and typhoid fever;
- influenza and sepsis;
- chlamydia and osteomyelitis;
- purulent otitis and peritonitis;
- any pathologies of a purulent nature;
- diseases of the lungs and respiratory organs that have a chronic course.
It is noteworthy that in addition to the above factors, focal pneumonia in children can be caused by a severe stressful situation or nervous overstrain, as well as the influence of such factors:
- hypothermia of the body;
- penetration of a foreign object into the bronchi;
- inhalation of toxic or poisonous substances.
In cases where inflammation of the lung lobule acts as an independent disease, the pathology is caused by the influence of pathogenic agents, which are:
- pneumococci and staphylococci;
- streptococci and Escherichia coli;
- proteus and Friendlander's wand;
- influenza A and B viruses;
- microscopic fungi;
- mycoplasma and adenovirus;
- parainfluenza virus and rhinovirus.
It must be taken into account that most often the above microorganisms influence the development of community-acquired pneumonia.
Also among the predisposing factors, clinicians identify:
- lack of physical activity;
- decreased immune system resistance;
- excessive addiction to bad habits, in particular smoking cigarettes;
- poor nutrition;
- hypovitaminosis;
- previous operations, no matter what area the surgery was performed on;
- prolonged overheating of the body.
The pathogenesis of focal pneumonia has some features:
- localization of inflammation in one or several lobules of the lung;
- slow development of the pathological process, which is explained by the small area of the affected area;
- acquisition of intense permeability by the walls of the lung;
- a smooth transition from one degree of severity to another, while the symptoms do not change dramatically.
Classification
By type, focal pneumonia in adults and children can also occur:
- aspiration pneumonia - develops due to the penetration of foreign objects into the lungs, the influence of toxic substances and severe alcohol intoxication;
- congestive pneumonia - occurs in seriously ill patients who are bedridden and require nursing care. Most often this occurs against the background of heart defects, advanced diabetes mellitus, coronary artery disease and stroke, injuries of the spinal column or skull.
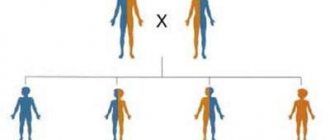
Classification of focal pneumonia
There are several ways pathological agents enter the human body:
- bronchogenic - this mechanism operates during bronchoscopy or other instrumental diagnostic procedures;
- hematogenous - becomes important in cases of the presence of distant septic foci or with bacteremia;
- lymphogenous;
- airborne;
- contagious – associated with the direct spread of the pathogen from organs adjacent to the lungs.
The disease goes through three stages:
- hot flash - lasts the first three days from the moment of influence of the provoking factor;
- hepatization - in this case, the tissues of the affected area of the lung change their shade. This stage continues from the fourth to the seventh day of the inflammation;
- resolution or recovery - begins on the seventh day and lasts until the patient’s normal condition is completely restored.
Classification depending on severity:
- mild – symptoms are mild, sometimes completely absent;
- moderate – clinical signs become more intense;
- severe or acute - in adults and children, symptoms lead to a significant deterioration in general condition.
Inflammation can develop under various conditions, which is why they include:
- community-acquired or home focal pneumonia;
- nosocomial, hospital-acquired or nosocomial pneumonia;
- focal pneumonia associated with the provision of medical care.
According to the location of the inflammatory focus, the disease is divided into:
- right-sided pneumonia - diagnosed most often, which is explained by the peculiarity of the structure of the right lung - it is larger and wider than the left half;
- left-sided pneumonia;
- bilateral damage - in this case, inflammation of the lobules of both the left and right lungs is observed;
- upper lobe;
- middle lobe;
- lower lobe pneumonia – most common.
Focal confluent pneumonia is distinguished separately - in this case, inflammation affects several segments or lobules of the lung. During diagnosis, it is expressed by the presence of multiple separate areas susceptible to the inflammatory process. It is characterized by a severe course and a high probability of developing consequences.
Forms of focal pneumonia
There are several types of focal pneumonia:
- Finely focal;
- Large focal;
- Focal-confluent.
In small focal pneumonia, the lesions are small in size, which is reflected in the name of this form of the disease.
Accordingly, macrofocal pneumonia suggests the presence of more extensive foci of damage to the lung tissue. They manifest themselves as clearly visible changes on an x-ray, while small-focal changes in the lungs usually cause only a slight change in the pattern of the respiratory organs.
With focal confluent pneumonia, individual foci of inflammation merge. The inflammatory process spreads to several segments of the lung; in particularly severe cases, the entire lobe is affected.
During the examination, the lag of one lung from the other during breathing is clearly diagnosed, the patient develops shortness of breath and cyanosis (blue discoloration of some areas of the skin and mucous membranes).
Based on the location of the disease, two forms of focal pneumonia are distinguished - left-sided - if the inflammation is localized only in the left lung, and right-sided.
Symptoms
Clinical manifestations will differ somewhat depending on the location of the pathological focus.
For example, for bilateral focal pneumonia the following will be characteristic:
- a sharp increase in temperature, which is very difficult to get rid of, even with the help of antipyretics;
- severe headaches;
- intense pain and burning in the chest. Such unpleasant symptoms tend to worsen when inhaling;
- increased sweating;
- shortness of breath and dry cough, which is accompanied by sputum as the disease progresses. In such cases, they talk about the development of purulent pneumonia;
- pale or bluish skin;
- appearance of rashes.
Right lower lobe pneumonia has the following symptoms:
- discomfort and pain localized on the right side of the chest;
- cough with sputum, which may contain streaks of pus or blood;
- chills and fever;
- sweating at night.
Changes in pneumonia
Symptoms of left-sided focal pneumonia are presented:
- low-grade fever;
- heaviness and pain in the right side;
- severe cough - may be dry or with sputum production;
- chills and general weakness;
- shortness of breath and sweating.
Any type of pneumonia can be accompanied by the following clinical manifestations:
- decreased performance;
- weakness and weakness;
- the appearance of wheezing when breathing;
- muscle and joint pain;
- decreased or complete lack of appetite;
- heart rate disturbance;
- confusion;
- pathological blush of the facial skin;
- unhealthy shine in the eyes;
- abdominal pain;
- disruption of the bowel movement process, which often results in diarrhea;
- attacks of nausea and vomiting.
The last category of symptoms is most typical for community-acquired focal pneumonia.
All of the above signs can be applied to both adults and children, but it is worth considering that in the latter the disease develops faster and is more severe.
Symptoms
Chronic focal pneumonia usually develops gradually; the onset of the disease is not acute or pronounced. The appearance of inflammation is preceded by an incubation period, during which the disease does not manifest itself in any way.
After focal pneumonia enters the active stage, characteristic symptoms appear:
- Chest pain appears, which intensifies with deep breaths and coughing;
- Wheezing in the lungs;
- Shortness of breath occurs;
- Breathing and heart rate increase;
- The patient is tormented by a cough - at the beginning of the development of the disease it is dry, then with sputum;
- The nasolabial triangle acquires a bluish tint;
- The sputum is white or yellow and contains an admixture of pus;
- There is pain in the head and back of the head;
- In most cases, body temperature rises - it can range from 37 to 39 ° C;
- Chills appear;
- The patient is concerned about general malaise and weakness.
This is a general picture of focal pneumonia, but this disease has many variants of its course, and its symptoms can be varied. In young patients, the disease can develop acutely, with high fever and chills from the first day.
Cough is the most characteristic sign of focal pneumonia - this symptom manifests itself more often than others. It can have a different character and different intensity.
In the early stages of development, focal pneumonia often resembles bronchitis. In such cases, it is usually diagnosed late, after it has spread to many lobes of lung tissue and cause great harm to health.
Inflammation spreads from top to bottom, gradually affecting the bronchi, bronchioles and alveoli. In some cases, peribronchial foci appear - this is the name given to horizontal areas affected by the disease during the transverse spread of pneumonia.
Diagnostics
Since right-sided or left-sided focal pneumonia has a wide variety of causes, a wide range of laboratory and instrumental studies will be required to establish a final diagnosis and determine the provoking etiological factor.
However, first of all, the pulmonologist should independently carry out a number of manipulations:
- get acquainted with the medical history - to identify a chronic disease that could serve as a source of development of community-acquired focal pneumonia;
- analysis of the patient’s life history - to determine the influence of one or another predisposing factor that does not have a pathological basis;
- a thorough physical examination - to assess the condition of the skin and listen to the patient using a phonendoscope. This also includes measuring temperature and heart rate;
- a detailed survey - to establish the severity of symptoms, which will indicate the severity of left-sided or right-sided focal pneumonia in a child and an adult.
Laboratory diagnostic measures are based on:
- PCR tests;
- general clinical analysis and blood biochemistry;
- bacterial culture of sputum - to determine the causative agent of the disease;
- blood test for blood culture;
- microscopic study of bronchial lavage.
In addition, the following instrumental procedures are carried out:
- X-ray of the sternum;
- fibrobronchoscopy;
- MRI and CT scan of the affected organ.
X-ray for focal pneumonia
It is necessary to differentiate pneumonia accompanied by lobar lesions of the lung with the following ailments:
- tuberculosis;
- alveolar lung cancer;
- abscess formation;
- pulmonary infarction.
Diagnosis of this lung disease
To determine the symptoms and treatment of pneumonia, you must seek medical help. A number of mandatory procedures are carried out for diagnosis. The role of symptoms of the disease is great, on the basis of which diagnostic methods for detecting bronchopneumonia are based.
Symptoms:
- Chills, fever, increased body temperature;
- Auscultatory modifications of the lung susceptible to disease;
- Specific cough with purulent sputum or small blood spots;
- Presence of infiltrate in the lungs;
- Decrease or increase in the number of leukocytes in the blood.
Great importance in diagnosis is given to the auscultatory method, which allows you to very quickly distinguish bronchopneumonia from other types of pneumonia. During auscultation over the affected organ, a decrease and reduction in the sound of the lung is noted; this process is caused by a failure in bronchial conduction.
X-ray diagnostics can detect the presence of infiltrates, pleurisy, enlargement of the lung and its significant deformation compared to a healthy organ.
A characteristic phenomenon for pneumonia, just like for tuberculosis, cancer and heart attack, is the formation of abnormal dark areas on an x-ray.
The purpose of laboratory diagnostics is to study the patient’s biomaterials - sputum or bronchial washings. For this, different methods are used, for example, microscopic, serological, bacteriological methods. When examining blood, attention is paid to the content of leukocytes and blood proteins, and an increase in the erythrocyte sedimentation rate.
Treatment
Regardless of the classification, the elimination of such a disease is carried out using conservative methods.
Treatment of focal pneumonia is based on taking medications, including:
- antibacterial substances - used for a course of at least two weeks;
- anti-inflammatory drugs;
- detoxification agents;
- corticosteroids;
- mucolytics and bronchodilators;
- drugs to thin mucus and facilitate its removal;
- immunomodulators;
- vitamin complexes.
This disease can also be treated with physiotherapeutic procedures, in particular:
- medicinal electrophoresis;
- UHF;
- DWI therapy.
In addition, the therapy includes a course of therapeutic massage and exercise therapy. In severe cases of the disease, they turn to plasmapheresis.
Other treatment of focal pneumonia in children and adults is unacceptable.
Features of therapy
The main forms of focal inflammatory changes in the lungs can be cured at home if an integrated approach is followed.
- Antibacterial therapy. Its timely and early appointment is a fundamental factor. It is advisable to use broad-spectrum chemotherapy drugs if there is no precise microbiological verification. Lack of improvement within 2-3 days is an indication to change the antibiotic.
- Symptomatic therapy: anti-inflammatory drugs, antihistamines, bronchodilators, mucolytics, expectorants.
- General rules: bed rest, high-calorie diet, vitamin therapy, drinking plenty of fluids.
- Physiotherapy: inhalations, massage, therapeutic exercises during the period of convalescence and additional restoratives are extremely important for a complete recovery.
If a severe course or complications are detected, hospitalization in a hospital is necessary for intensive infusion therapy.
Treatment with folk remedies
Treatment with folk remedies can only be used in combination with standard methods. Herbal medicine is especially relevant as a symptomatic treatment:
- Warm baths with herbal infusions;
- Infusions and teas;
- Inhalations.
Folk remedies for immunostimulation consist of a mixture of rose hips, lingonberries, raspberries, black currants, thyme and other herbs; they are useful for any inflammatory process. For the same purpose, propolis, garlic, onions, butter and olive oil are actively used.
To get rid of a dry cough, infusions of oregano, coltsfoot, marshmallow, and licorice root can help. To thin phlegm, simple folk recipes are used in the form of brewing teas with the addition of violets, pine buds, plantain, as well as onion and black radish juice with honey.
Honey can be used as an anti-inflammatory folk remedy in the form of warm compresses. Badger fat is very active and beneficial, promoting the rapid resolution of inflammation of the lung tissue and preventing the occurrence of fibrosis. Inhalations with eucalyptus and birch buds are also often used.
Russian culture, rich in traditions, has over the course of many centuries created many folk recipes for all diseases, including pneumonia. Active fight against pathogenic microorganisms using modern chemotherapy drugs in combination with non-traditional methods helps to speed up recovery and prevent complications.
Complications
Ignoring clinical signs and untimely therapy is fraught with the development of the following, quite dangerous complications of focal pneumonia:
- formation of abscesses or gangrene;
- toxic shock and sepsis;
- acute respiratory failure;
- anemia and pleurisy;
- pulmonary hemorrhage;
- glomerulonephritis and meningoencephalitis;
- myocarditis and amyloidosis;
- heart failure;
- empyema of the pleura.
Prevention and prognosis
Preventive measures that reduce the likelihood of such a disease may include:
- vaccination against inflammatory agents;
- rejection of bad habits;
- balanced diet;
- preventing hypothermia or overheating of the body;
- avoidance of stressful situations;
- timely treatment of viral infections and other diseases of the respiratory system;
- Regularly undergoing a full medical examination.
Rational and early treatment leads to the fact that focal pneumonia has a favorable prognosis. Complications develop quite rarely, which is why the disease almost never leads to death.