Symptoms
Common symptoms of lung cancer
- Fast weight loss,
- no appetite,
- decline in performance,
- sweating,
- unstable temperature.
Specific signs:
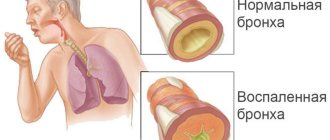
- a debilitating cough without an obvious reason is a companion to bronchial cancer. The color of the sputum changes to yellow-green. In a horizontal position, physical exercise, or in the cold, coughing attacks become more frequent: a tumor growing in the area of the bronchial tree irritates the mucous membrane.
- Blood when coughing is pinkish or scarlet, with clots, but hemoptysis is also a sign of tuberculosis.
- Shortness of breath due to inflammation of the lungs, collapse of part of the lung due to tumor blockage of the bronchial tube. With tumors in large bronchi, organ shutdown may occur.
- Chest pain due to the penetration of cancer into the serous tissue (pleura), growing into the bone. At the beginning of the disease there are no warning signs; the appearance of pain indicates an advanced stage. The pain can radiate to the arm, neck, back, shoulder, intensifying when coughing.
The degree of intensity of the symptoms of the clinical picture will directly depend on the volumes of the lung involved in the pathological process. For example, microatelectasis or damage to only one segment of the lung can be completely asymptomatic. In such cases, the pathology will be a diagnostic finding, which is often discovered during a radiograph for prophylactic purposes.
The disease manifests itself most acutely when an entire lobe of this organ is affected, in particular, atelectasis of the upper lobe of the right lung. Thus, the basis of the clinical picture will be the following signs:
- shortness of breath - it appears suddenly both during physical activity and at rest, even in a horizontal position;
- pain of varying degrees of intensity in the chest area from the affected lung;
- severe dry cough;
- violation of heart rate, namely its increase;
- decreased blood tone;
- cyanosis of the skin.
Similar symptoms are typical for both adults and children.
In case of incomplete blockage, air enters the bronchus during inhalation, but when exhaling it does not come out, but, remaining in the alveoli and accumulating there, gives a picture of partial emphysema corresponding to the affected bronchus. When the bronchus is completely blocked, air cannot enter or leave this area of the lung.
The remaining air is gradually absorbed, the alveoli collapse, and the lung becomes airless in this area. In one area or another of the lung there is a picture of atelectasis, which is the second most important symptom of primary lung cancer after cough, according to some authors.
Atelectasis of the lung creates favorable conditions for the development of infection. Distal to the tumor, abscesses easily arise with a corresponding rise in temperature, with a horizontal level, etc., which confuses the picture of the underlying disease. According to some data, 10% of all lung abscesses in patients undergoing examination developed due to lung cancer.
Almost the same as a cough, weakness is a constant symptom. About 50% of our patients turned out to be so weak that they had to be declared unable to undergo surgery even before a trial thoracotomy.
Another characteristic symptom of lung cancer is chest pain. According to N.N. Grinchar, this symptom occurred in 82% of cases. There is no exact data on the genesis of these pains. And if in peripheral cancers the origin and transmission routes of pain are more or less clear, since they are caused by irritation of the pleura and intercostal nerves, then in tumors of the lung root we have not found a sufficiently substantiated explanation.
With a peripheral tumor location, even significant intercostal pain does not always indicate tumor growth into the chest wall. In one of our patients, the nature and intensity of intercostal pain in the upper half of the chest wall did not raise any doubt that the tumor had grown into the intercostal spaces in the area of the 4th-6th ribs on the right, to which it was directly adjacent, and we could not differentiate it from the ribs during fluoroscopy.
The next important and fairly early symptom is shortness of breath. It is associated not only with atelectasis, but also with secondary inflammatory phenomena in the lungs. An early symptom is slight shortness of breath, which usually cannot be explained by objective findings of either the heart or lungs. Dyspnea to one degree or another was observed in 55% of our patients.
Severe, painful shortness of breath is a common symptom of large tumor spread and is often a sign of inoperability.
Causes
The mechanisms of cell degeneration are not fully understood. But thanks to numerous studies, chemicals have been identified that can accelerate cell transformation. We will group all risk factors according to two criteria.
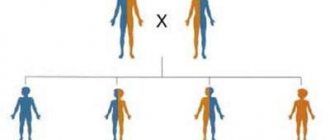
Reasons beyond a person's control:
- Genetic predisposition: at least three cases of a similar disease in the family or the presence of a similar diagnosis in a close relative, the presence of several different forms of cancer in one patient.
- Age after 50 years.
- Tuberculosis, bronchitis, pneumonia, scars on the lungs.
- Problems of the endocrine system.
Modifiable factors (what can be influenced):
- Smoking is the main cause of lung cancer. When tobacco is burned, 4,000 carcinogens are released, covering the bronchial mucosa and burning living cells. Together with the blood, the poison enters the brain, kidneys, and liver. Carcinogens settle in the lungs until the end of life, covering them with soot. Smoking experience of 10 years or 2 packs of cigarettes per day increases the chance of getting sick by 25 times. Passive smokers are also at risk: 80% of exhaled smoke comes from them.
- Professional contacts: asbestos-related factories, metallurgical enterprises; cotton, linen and felt mills; contact with poisons (arsenic, nickel, cadmium, chromium) at work; mining (coal, radon); rubber production.
- Poor ecology, radioactive contamination. The systematic influence of air polluted by cars and factories on the lungs of the urban population changes the mucous membrane of the respiratory tract.
Atelectasis is a pathological condition that develops as a result of collapse of the lung or part of it, followed by compaction and a decrease in air content. Atelectasis usually develops against the background of an underlying disease; its occurrence has certain prerequisites. The causes of pulmonary atelectasis include:
- bronchial obstruction - blockage of the bronchus with subsequent resorption of air just below the blocked area;
- the formation of extensive pleural effusion, which compresses the lung tissue from the outside;
- the formation of a blood clot in the lungs due to internal bleeding, in which the patient cannot cough up blood;
- formation of viscous secretion in the bronchi due to pneumonia, chronic bronchitis, pulmonary infarction and similar diseases;
- compression of the lung tissue due to the impact of a tumor, an enlarged lymph node, or penetration of a foreign object into the mediastinum;
- impaired ventilation of the lungs and accumulation of thick mucus in the bronchi due to the use of general anesthesia during surgery;
- long-term adherence to bed rest, in which the patient does not change body position.
Atelectasis of the lung is accompanied by pronounced symptoms that cannot be ignored. These are chest pain, shortness of breath, cyanosis, hypotension and tachycardia, weakened voice and breathing, increased body temperature if atelectasis is complicated by a bacterial infection. During the physical examination, a dull percussion sound and retraction of the affected area of the chest during breathing are observed.
The results of radiography show a high position of the diaphragm, a decrease in the transparency of the affected area of the lung, and a displacement of the mediastinal organs to one side. In case of atelectasis, it is appropriate to conduct bronchography and computed tomography as part of a more in-depth study of the causes of the pathology.
How is pulmonary atelectasis treated?
Treatment of atelectasis is aimed at eliminating the factor that provokes it, restoring bronchial patency and preventing infection. When the bronchi are obstructed by foreign bodies or sputum, bronchoscopy is used. In uncomplicated cases, sputum can be removed by coughing, as well as by using a catheter inserted into the bronchus.
To prevent the collapse of the lung from being accompanied by an infectious process, the patient is prescribed antibacterial drugs. To stimulate weakened breathing, etimozol may be used. At the same time, courses of breathing exercises are prescribed, and for active coughing up of thick and viscous sputum, thinning and bronchodilator drugs are prescribed.
Prevention of atelectasis for patients with pneumonia and other potentially dangerous diseases of the respiratory system consists of improving pulmonary drainage, the same is recommended for postoperative patients.
Therapy for the pathological condition of the lung tissue is primarily aimed at neutralizing the provoking factor and restoring bronchial patency. Measures are also taken to prevent the occurrence and suppression of the inflammatory process.
If obstruction of the bronchi is caused by foreign objects or accumulated sputum, the plug is removed using bronchoscopy. For milder atelectasis, bronchodilators and expectorants are used to remove sputum.
- When atelectasis develops against the background of lung cancer, the cause of collapse of the lung tissue is compression of the bronchi by the resulting tumor; surgery, chemotherapy and radiation are used. In severe cases of atelectasis, intubation and artificial ventilation are used. Activities are carried out until the patient’s condition is completely stabilized and the underlying disease is completely controlled. To prevent the development of infection, the patient is prescribed antibacterial agents and antibiotics. The treatment also includes measures to improve the respiratory process. The patient is prescribed drugs that stimulate breathing. Simultaneously with the treatment, the patient is prescribed various courses of breathing exercises, and bronchodilators and expectorants are prescribed to thin the viscous sputum and stimulate its removal.
Prevention of atelectasis
This pathology can be completely prevented in some cases if the factors predisposing to the disease are eliminated. Preventive measures are as follows:
- You need to give up bad habits. Smoking increases the risk of developing atelectasis.
- After the operation, the patient must do breathing exercises, which helps maintain normal airway patency. In addition, chest massage and early rise after operations are indicated.
- Bedridden patients should often be turned over in bed and given massage.
- Timely treatment of inflammatory diseases of the bronchi and lungs.
Prevention also includes maintaining a healthy lifestyle, when rest alternates with moderate physical activity. Proper nutrition also plays an important role in preventing disease.
Atelectasis is often observed in people with various chest deformities, as well as neurological pathologies. In this case, patients are recommended special devices that make breathing easier and prevent lung tissue from collapsing.
How to prevent the development of pathology
There are many factors that cause pulmonary atelectasis:
- Blockage of the bronchus, and therefore the resorption of air below the closed area Formation of abundant exudate in the pleura, as a result of which it compresses the lung tissue Blockage of the passage with a blood clot formed as a result of internal bleeding Closure of the lumens with viscous mucus released during the inflammatory process (bronchitis, pneumonia and other diseases) Compression of the lung tissue by a neoplasm, an enlarged lymph node or a foreign body that has gotten inside. Impaired ventilation of the lungs and the formation of copious viscous sputum after the use of anesthesia during surgery. Chest injuries. Narcotic and sedatives. Consequences of prolonged bed rest, immobility of the patient.
The development of pathology of lung tissue in lung cancer is indicated by pronounced signs:
- Chest pain Tachycardia Shortness of breath Feeling of lack of air Low blood pressure Weakening of voice and breathing When a bacterial infection occurs, body temperature rises.
To prevent damage to the lung tissue and prevent the development of atelectasis, it is necessary to exclude the causes that provoke it:
- Give up cigarettes. Smoking increases the production of sputum, injures the mucous membrane of the lungs, and provokes the development of lung cancer. Carefully monitor small objects and prevent them from entering the respiratory tract. Monitor children's behavior while eating, and prevent them from indulging in bread crumbs, seeds, nuts and other foods. For any respiratory diseases, as well as in the postoperative period, do breathing exercises. When on bed rest, avoid lying in one position for a long time. It is required to regularly change body positions, and if the doctor allows it, then get out of bed.
The development of atelectasis in lung cancer not only seriously complicates the already poor condition of the patient, but also provokes the following complications in the functioning of the body. Correct diagnosis and timely treatment are required to eliminate the pathology.
Possible consequences
If the disease is not treated in a timely manner or the treatment is carried out in full, then the following complications may occur:
- Acute respiratory failure. At the same time, the supply of oxygen to the body is greatly limited.
An infection occurs, due to which pneumonia and lung abscess develop. The latter case is dangerous because a cavity forms in the respiratory organ, which is filled with pus.
If the size of the affected area is too large or the entire lung is compressed, then death is possible, especially if the disease develops rapidly.
How does atelectasis manifest in lung cancer?
The development of pathology of lung tissue in cancer patients is of the obstructive type in origin - that is, atelectasis develops due to the closure of the bronchial lumen from the inside by a formed tumor or accumulated sputum.
When the lumen is not completely blocked, air enters the bronchus when inhaling, but cannot leave it when exhaling. It remains in the alveoli, and gradually accumulates, contributing to partial emphysema in the affected organ. If the lumen is completely closed, the movement of air stops - it does not pass through either inhalation or exhalation.
Symptoms of atelectasis can manifest themselves in different ways, depending on the area and number of affected areas. With the sluggish development of the pathology, affecting a small part of the organ, the symptoms appear weakly, inexpressively or completely absent. They intensify as the condition of the lung tissue worsens. Typical manifestations of atelectasis are:
- Difficulty breathing and shortness of breath Unproductive cough without sputum, which does not bring relief Sharp pain in the chest, intensifying with inhalation and exhalation Cyanosis (bluish color of the skin) Reduction in the volume of the chest on the side of the affected organ Narrowing of the intercostal spaces Displacement of the spine to the healthy side.
But if atelectasis occurs suddenly, develops at high speed and affects a large part of the lung, then the symptoms of respiratory failure manifest themselves violently and can even cause a state of shock in the body. There is a sharp decrease in blood pressure and the development of tachycardia. In addition, a feverish state may occur - most often this happens as a complication of pneumonia.
With pulmonary atelectasis, favorable conditions are created for pathogenic microorganisms. Abscesses develop, accompanied by fever and other symptoms, which greatly complicates diagnosis. According to medical statistics, 10% of abscesses occur due to cancer and atelectasis.
Find out more about lung cancer here.
Classification
By origin, atelectasis of the lung lobe can be congenital (that is, primary) or acquired (that is, secondary).
By primary disease we mean a condition when a newborn baby’s lung does not expand. As for acquired atelectasis, in this case there is a collapse of the lung tissue, which was previously involved in the breathing process.
It must be said that such phenomena should be distinguished from intrauterine atelectasis, that is, the airless state of the lungs that is observed in the fetus, and physiological (that is, hypoventilation that occurs in completely healthy people and represents a certain functional reserve of the lung tissue).
Treatment
Treatment of atelectasis is best carried out under round-the-clock medical supervision in a hospital setting. If the attending physician considers it acceptable to prescribe treatment at home, it must be strictly adhered to, performing breathing exercises, taking medications and strengthening the general immune system.
A collapsed lung is a condition from which recovery is not possible using folk remedies.
Treatment of atelectasis during pregnancy is difficult, and therefore it is better to prevent the disease. If there are factors predisposing to atelectasis, it is necessary to take all possible preventive measures to prevent the collapse of the lung.
https://www.youtube.com/watch?v=Swtw_Ok20Qk
The type (surgical, radiological, palliative, chemotherapy) is selected based on the stage of the process, histological type of tumor, medical history). The most reliable method is surgery. For stage 1 lung cancer, 70-80%, stage 2 - 40%, stage 3 - 15-20% of patients survive the control period of five years. Types of operations:
- Removal of a lobe of the lung corresponds to all principles of treatment.
- Marginal resection removes only the tumor. Metastases are treated in other ways.
- Removal of the lung completely (pneumoectomy) - with a tumor of 2 degrees for central cancer, 2-3 degrees - for peripheral cancer.
- Combined operations - with the removal of part of the adjacent affected organs.
Surgery is not recommended for serious concomitant diseases (myocardial infarction, diabetes mellitus, renal and liver failure) if the tumor affects the trachea.
Chemotherapy has become more effective thanks to new drugs. Small cell lung cancer responds well to polychemotherapy. With the right combination (taking into account sensitivity, 6-8 courses with an interval of 3-4 weeks), survival times increase 4 times. Chemotherapy for lung cancer. It is carried out in courses and gives positive results for several years.
Non-small cell cancer is resistant to chemotherapy (partial tumor resorption occurs in 10-30% of patients, complete resorption is rare), but modern polychemotherapy increases survival rate by 35%.
They also treat with platinum preparations - the most effective, but also the most toxic, which is why they are administered with large (up to 4 liters) amounts of liquid. Possible adverse reactions: nausea, intestinal disorders, cystitis, dermatitis, phlebitis, allergies. The best results are achieved with a combination of chemotherapy and radiation therapy, simultaneously or sequentially.
Radiation therapy uses gamma-ray installations of beta-trons and linear accelerators. The method is designed for inoperable patients of grade 3-4. The effect is achieved due to the death of all cells of the primary tumor and metastases. Good results are obtained with small cell cancer. In case of non-small cell irradiation, irradiation is carried out according to a radical program (in case of contraindications or refusal of surgery) for patients of 1-2 degrees or for palliative purposes for patients of 3 degrees. The standard dose for radiation treatment is 60-70 gray. In 40% it is possible to achieve a reduction in the oncological process.
Palliative care - operations to reduce the impact of the tumor on the affected organs to improve the quality of life with effective pain relief, oxygenation (forced oxygen saturation), treatment of associated diseases, support and care.
Traditional methods are used exclusively to relieve pain or after radiation and only in consultation with a doctor. Relying on healers and herbalists for such a serious diagnosis increases the already high risk of death.
After studying the results of all diagnostic measures, the clinician draws up an individual treatment strategy for each patient, taking into account the etiological factor.
However, in almost all cases, conservative techniques are sufficient. Thus, treatment of pulmonary atelectasis may include:
- suction of exudate from the respiratory tract using a rubber catheter - this measure is indicated for patients with primary atelectasis. In some cases, newborns may need to be intubated or inflated with air;
- therapeutic bronchoscopy – if the etiological factor was the presence of a foreign object;
- lavage of the bronchi with antibacterial substances;
- sanitation of the bronchial tree endoscopically - if the collapse of the lung is caused by the accumulation of blood, pus or mucus. This procedure is called bronchoalveolar lavage;
- tracheal aspiration - in cases where pulmonary atelectasis was caused by a previous surgical intervention.
For a disease of any nature, patients are advised to:
- taking anti-inflammatory drugs;
- performing breathing exercises;
- completing a percussion massage course;
- postural drainage;
- exercise therapy class;
- UHF and drug electrophoresis;
- inhalations with bronchodilators or enzyme substances.
It is worth noting that patients are prohibited from independently treating the disease with folk remedies, since this can only aggravate the problem and lead to the development of complications.
If conservative methods of therapy are ineffective in straightening the lung, they resort to surgical intervention - resection of the affected area of the lung, for example, with atelectasis of the middle lobe of the right lung or other localization of the pathology.
Diagnostic features
Diagnosing lung cancer is not an easy task, because oncology looks like pneumonia, abscesses, and tuberculosis. More than half of tumors are detected too late. For the purpose of prevention, it is necessary to undergo an x-ray annually. If cancer is suspected, they undergo:
- Fluorography to determine tuberculosis, pneumonia, lung tumors. If there are deviations, you need to take an x-ray.
- X-ray of the lungs more accurately assesses the pathology.
- Layer-by-layer X-ray tomography of the problem area - several sections with the focus of the disease in the center.
- Computed tomography or magnetic resonance imaging with the introduction of contrast on layer-by-layer sections shows in detail and clarifies the diagnosis according to explicit criteria.
- Bronchoscopy diagnoses central cancer tumors. You can see the problem and take a biopsy - a piece of affected tissue for analysis.
- Tumor markers test the blood for a protein produced only by the tumor. The NSE tumor marker is used for small cell cancer, the SSC and CYFRA markers are used for squamous cell carcinoma and adenocarcinoma, and CEA is a universal marker. The diagnostic level is low; it is used after treatment for early detection of metastases.
- Sputum analysis has a low probability of suggesting the presence of a tumor if atypical cells are detected.
- Thoracoscopy - examination through camera punctures into the pleural cavity. Allows you to take a biopsy and clarify changes.
- A biopsy with a CT scan is used when there is doubt about the diagnosis.
The examination must be comprehensive, because cancer masquerades as many diseases. Sometimes they even use exploratory surgery.
Making a correct diagnosis, as well as finding out the localization and extent of the pathological process, is possible only with the help of instrumental examinations of the patient. However, before carrying out such procedures, it is necessary for the pulmonologist to independently carry out several manipulations.
Thus, the primary diagnosis will include:
- studying the medical history and collecting the patient’s life history - to identify the most likely etiological factor;
- a thorough physical examination, including auscultation of the patient. In addition, it is necessary for the doctor to assess the condition of the skin, measure pulse and blood pressure;
- detailed survey of the patient - to obtain detailed information regarding the first time of onset and the degree of intensity of symptoms. This will allow the doctor to assess the severity of the disease and its form, for example, atelectasis of the lower lobe of the right lung.
Laboratory research is limited to carrying out only blood biochemistry, which is necessary to study its gas composition. Such an analysis will show a decrease in the partial pressure of oxygen.
To definitively confirm the diagnosis, the following is carried out:
- bronchoscopy - will help to accurately identify the cause of this disease;
- X-ray – performed while inhaling. In this case, there will be a displacement of the organs of the mediastinal region towards the affected lung, and on exhalation - towards the area of the healthy half;
- bronchography and angiopulmonography - to assess the level of damage to the pulmonary-bronchial tree;
- CT scan of the lungs is performed in case of questionable radiographic findings and to clarify the localization of the pathology, in particular, to identify atelectasis of the upper lobe of the left lung or any other focus.
Atelectasis of the lung on a radiograph
To determine atelectasis in lung cancer, studies are carried out:
- Examination of the patient, familiarization with the medical history. Palpation – determines the degree of voice trembling. With complete atelectasis, the sign is absent; it intensifies with partial pathology of the organ. Percussion. Auscultation helps determine breathing. It is absent from the affected organ or is greatly weakened. Radiography. The images detail the condition of the lungs and show the location and degree of changes in the organ. On an x-ray, the compaction of lung tissue is determined by the degree of darkening. Depending on the affected area - the entire organ or individual areas. CT scan: helps to determine the area of atelectasis, as well as clarify other causes of the pathology. Bronchoscopy determines the causes of bronchial obstruction.
In addition, additional studies may be needed for diagnosis using PET-CT.
Prevention
Prevention of atelectasis is quite important. In case of bronchitis, in people who have reason to assume a tendency to develop pulmonary atelectasis, care should be taken to expectorate the accumulated sputum as best as possible. With processes that reduce the capacity of the chest cavity, it is often not possible to prevent the development of atelectasis; but where possible, for example, with effusion pleurisy, pressure on the lung should be relieved to prevent atelectasis.
It is also important to ensure that patients, especially those in a coma or unconscious state, do not lie on one side or on their back for a long time. Patients who breathe shallowly, or who for other reasons have a tendency to atelectasis, should be forced to inhale and exhale deeply several times during the day in a sitting position, in order to thus eliminate congestion in the parts of the lungs that are not ventilated and contain less air. between the walls of the bronchi, and if this has already happened, to help move them apart.
You can prevent the occurrence of atelectasis of any kind if you follow the following rules:
- Adhere to a healthy lifestyle.
- During the recovery period after bronchopulmonary diseases, follow all doctor’s recommendations.
- Control your weight.
- Do not take medications without a doctor's prescription.
- Be regularly examined for preventive purposes.
The success of treatment depends on the cause of atelectasis and timely measures taken. A mild form of the disease can be cured quickly.