It is more logical to use the name cardiomyopathy, that is, in the plural, since even in ICD-10, two sections list a dozen and a half varieties that differ both in characteristics and causes of occurrence.
Note that the pathology has an extremely unfavorable prognosis. There is a high likelihood of complications that can lead to sudden death.
What is cardiomyopathy
The term cardiomyopathy was coined in 1957 by British cardiologist Wallace Brigden (1916 – 2008), who pioneered many innovations in the treatment of diseases of the cardiovascular system. This term defined a group of diseases whose causes were not clearly defined. Important. The cardiomyopathy group combines pathologies that represent selective deformation of the heart muscle (myocardium).
The essence of selectivity is that only the heart muscle changes structurally and functionally, but the important parts of the body associated with it, for example, the coronary arteries and the valvular apparatus of the heart, do not undergo changes.
Advances in understanding the essence of cardiomyopathies were marked by the 1980 classification, which referred to the unknown origin of pathologies of the heart muscle. And only in 1996, by the decision of the international society of cardiologists, the definition of cardiomyopathies as various myocardial diseases, which are characterized by disturbances of cardiac activity, was put to rest.
The diseases are characterized by pathological changes in the myocardium, which are manifested by heart failure, arrhythmia, fatigue, swelling of the legs, and a general deterioration in the functioning of the body. There is a significant risk of developing serious heart rhythm disturbances that can be fatal.
The disease affects people of any age category, regardless of gender. Cardiomyopathies are divided into several types depending on the specific effect on the heart muscle:
- hypertrophic,
- dilatational,
- arrhythmogenic,
- pancreas,
- restrictive.
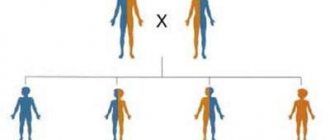
All types of the disease can be divided into primary (cause unknown) and secondary cardiomyopathy (hereditary predisposition or the presence of a number of diseases that impair the body's defenses). According to statistics, dilated and restrictive cardiomyopathies are the most common.
Hypertrophic cardiomyopathy is a thickening of the walls of the left ventricle (myocardial damage), while the cavities remain the same or decrease in volume, which significantly affects the heart rhythms.
Differentiation of the disease according to the reasons that caused cardiac dystrophy
Depending on the underlying causes that provoked cardiac pathology, all types of cardiomyopathies are differentiated into primary and secondary. Primary are those that develop independently against the background of genetic failures or during intrauterine development. Secondary - pathologies that are a consequence of past illnesses or other third-party effects on the body. Differential diagnosis when determining the type of cardiac pathology is very important.
Idiopathic (primary)
Primary cardiac pathology associated with disruption of the myocardium is also called unspecified, since the nature of its occurrence is unknown. Doctors attribute the causes of idiopathic pathology to genetics, congenital anomalies and very rarely viral etiology. That is, this type of cardiomyopathy develops on its own without obvious prerequisites. Idiopathic pathologies include arrhythmogenic myopathy. Arrhythmogenic pathology in most cases concerns only the right heart chamber. Here, zones with critically low pressure are formed in the right ventricle. In their place, fibrous-fatty layers form over time.
This is interesting: in most cases, arrhythmogenic pathology is hereditary and is inherited along with curly hair and keratoderma of the soles and palms, since these genes are located nearby. Women get sick more often.
Important : all other types of myocardial dysfunction are secondary. They develop as a result of microbiological, chemical or physical effects on the heart. A list of secondary cardiomyopathies is given below.
Toxic
Functional myocardial disorders develop against the background of prolonged exposure to various toxins on the body. This could be working in difficult chemical conditions (mercury vapor, heavy metal salts, etc.) or living in environmentally unfavorable areas.
Alcoholic
Develops under the influence of systematic libations. As you know, ethanol greatly disrupts metabolic processes in the body and washes away all electrolytes. Their lack provokes serious disturbances in the functioning of the heart. In most cases, alcoholics die from either cirrhosis of the liver or alcoholic cardiomyopathy (more often).
Metabolic
This type of cardiac pathology occurs against the background of seriously impaired metabolic processes. In this condition, the conduction of electrical impulses in the heart is disrupted. As a result, the myocardium suffers.
Dysmetabolic
This type of secondary pathology is more common in young and resilient athletes. Dysmetabolic myopathy occurs as a result of constant and prolonged overstrain of the heart muscle. After such a load, a person’s hemostasis is seriously impaired, which leads to the formation of endotoxicosis.
Dishormonal
As a rule, such myopathy is formed against the background of insufficient functioning of the hormonal and endocrine systems. In particular, this process cannot be classified as inflammatory. However, the myocardium suffers seriously if the patient is diagnosed with thyrotoxicosis (increased levels of thyroid-stimulating hormone), diabetes mellitus (diabetic cardiopathy) and other diseases leading to metabolic disorders and disruptions in the production of hormones.
Ischemic
This type of cardiac pathology is formed against the background of coronary heart disease, that is, insufficient nutrition of the heart due to arterial stenosis or thrombosis. Due to IHD (coronary heart disease), the patient may even have a myocardial infarction.
Hypertensive
Hypertensive (hypertensive) cardiomyopathy is the rarest of all the secondary pathologies listed. Most often diagnosed in men against the background of persistent hypertension. It is quite a serious threat to the patient's life. With this pathology, the myocardium becomes inelastic, which leads to a decrease in the contractility of the ventricular walls. As a result, the patient does not receive enough oxygen and other nutrients from the blood.
Peripartum
This pathology is abbreviated as PPCM (peripartum cardiomyopathy). It is mainly formed in completely healthy women in the last month of pregnancy or within 5 months after a successful birth. With such cardiomyopathy, patients most often die. The pathology is characterized by serious disturbances in the functioning of the left heart chamber. That is, its complete dysfunction occurs. The disease is considered very rare (1 case in 3000 births). The reason for the development still remains unspecified.
Cardiomyopathy of mixed origin
Here, several provoking factors can play an important role in the formation of pathology. Therefore, when making a diagnosis, cardiologists often prefer to use the term “cardiomyopathy of mixed origin.”
Dilated cardiomyopathy
With this damage to the heart muscle, the chamber of the predominantly left (less often both) ventricle of the heart expands without thickening of the heart walls.
Due to dilatation (stretching) of all four chambers, the heart increases in volume, and parietal blood clots form. These changes entail a decrease in the ability of the ventricles to contract and a decrease in the ejection of blood into the aorta (systolic dysfunction). A decrease in contractile function occurs due to thickening of the chamber walls due to inclusions of scar tissue, which does not have the functionality of cardiac muscle cells. As a result of a decrease in blood ejection, blood residues accumulate in the ventricles. Congestion occurs, which leads to heart failure. DCM, due to congestion, has received another name - congestive cardiomyopathy.
It is believed that genetic factors in the development of dilated cardiomyopathy are responsible for up to 30% of cases of the disease. The viral nature is recorded by statistics in 15% of cases.
The situation with uneven thickening of the walls of the cavities of the heart has its own name - cardiomegaly. Otherwise, this pathology is called “huge heart.” As a variant of this form of pathology, ischemic cardiomyopathy is diagnosed. It is typical that with this diagnosis there are multiple atherosclerotic vascular lesions and it is possible that there have been heart attacks (after all, the scar tissue in the heart muscle came from somewhere).
Important. Ischemic cardiomyopathy is not similar to coronary artery disease with its chest pain, but is based on wall expansion and early heart failure. The brunt (nine out of ten!) falls on men under the age of 50 or so.
In addition, it should be noted that heart failure caused by blood stagnation (ie, congestive cardiomyopathy) is a common cause of sudden death.
Statistics show that, based on gender, DCM affects men 60% more often than women. This is especially true for age groups from 25 to 50 years.
In general, the cause of the disease can be:
- any toxic effects - alcohol, poisons, drugs, anti-cancer drugs;
- viral infection - common flu, herpes, Coxsackie virus, etc.;
- hormonal imbalance – protein deficiency, vitamin deficiency, etc.;
- diseases that cause autoimmune myocarditis - lupus erythematosus or arthritis.
- heredity (family predisposition) – up to 30%.
Major complications
With cardiomyopathy, irreversible processes occur in the heart that change its structure. Cardiomyocytes, the heart cells, are the first to be affected. They undergo dystrophic and sclerotic changes, characterized by thickening of the myocardial walls, stretching of the ventricles and the formation of interventricular adhesions.
All processes occurring during cardiomyopathy disrupt the inflow and outflow of blood, which entails many complications. This disease always affects ventricular function and affects the myocardium.
Based on the reasons for its appearance, cardiomyopathy is divided into primary and secondary. Based on functional changes in the myocardium, the disease is divided into four types:
- dilated cardiomyopathy;
- hypertrophic;
- restrictive;
- arrhythmogenic.
Each of these types of disease has its own characteristics in damage to the heart muscle and symptoms. But they all end in serious complications, which often result in the patient’s disability or death.
The main causes of death in cardiomyopathy include the following complications:
- heart failure;
- myocardial infarction;
- thromboembolism;
- various types of arrhythmias;
- swelling of the lungs;
- heart failure.
Heart failure
The syndrome is manifested by a violation of the pumping function of the heart muscle, which leads to poor blood supply to the entire body. The clinical picture depends on which ventricle is affected.
In the case of left-sided heart failure, fluid stagnation occurs in the pulmonary circulation. The main complication in this case is pulmonary edema.
| Signs that cardiomyopathy has led to left ventricular dysfunction include the following: |
|
| In right ventricular heart failure, there is an accumulation of excess fluid in the vessels of the systemic circulation. This pathology is accompanied by the following symptoms: |
|
Each type of heart failure is accompanied by chronic fatigue and fatigue. Treatment of the pathology is carried out with drugs that eliminate edema, stabilize heart contractions and prevent the formation of blood clots. The same medications are used to treat cardiomyopathy.
To determine congestive cardiomyopathy, manifested by heart failure, the patient is prescribed the following diagnostic methods:
- ECG;
- radiograph;
- echocardiogram;
- Ultrasound of the heart;
- MRI;
- physical exercise testing.
Myocardial infarction
Most often, myocardial infarction occurs with hypertrophic cardiomyopathy. The condition is the death of a section of the myocardium, formed due to poor blood supply.
A lack of blood during a heart attack is caused by the formation of a thrombus (blood clot), which clogs the vessel and prevents blood from entering the cavity of the heart and its tissues. How extensive the myocardial damage will be depends on how much blood will not flow into the organ.
Symptoms of a heart attack are increasing in nature and are manifested by the following signs:
- chest pain of prolonged and intense etiology;
- chest tightness;
- nausea;
- vomit;
- difficulty breathing;
- panic attack;
- causeless anxiety;
- dizziness;
- heavy sweating;
- loss of consciousness.
As the heart attack progresses, pain from the sternum spreads to the lower and upper parts of the body. A person feels pain in the forearm, back, jaw, and stomach. The skin becomes pale and sticky. During myocardial infarction, the pulse becomes weak and irregular.
After a heart attack, adhesions form on the tissues of the heart muscle, leading to post-infarction cardiosclerosis. An advanced form of such a process will inevitably lead to the death of the patient.
Thromboembolism
Cardiomyopathy can be complicated by the development of thromboembolism - a congestive process in the blood vessels caused by a blood clot. The appearance of such clots disrupts the blood supply, provokes the death of myocardial tissue and can result in the death of the patient.
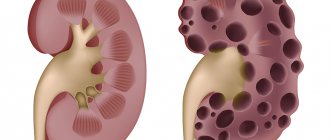
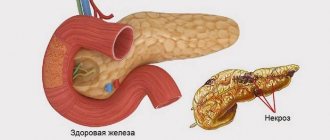
Thromboembolism can cause ischemic stroke, often fatal, due to the release of a blood clot entering the brain area. The disease can also provoke death of intestinal, lung, kidney tissue and necrosis of the extremities.
The symptoms of thromboembolism depend on the location of the blockage of the vessel. If the blood clot is located in the lower extremities, the pathology is accompanied by pain and the formation of gangrene. Blockage of blood vessels in the abdominal cavity is manifested by acute abdominal pain, vomiting, and nausea.
A blood clot formed in the right ventricle or atrium can cause heart failure and congestion in the systemic circulation. If such a blockage comes off, then the process of pulmonary embolism will be inevitable, which in 70% of cases ends in death.
Thrombotic blockages formed in the left side of the heart almost always lead to myocardial or cerebral infarction.
Arrhythmias
Cardiomyopathy is often complicated by arrhythmias, which are diagnosed in almost 90% of all patients. Arrhythmia is a pathological condition of the heart muscle in which disturbances occur in the contractile functioning of the organ.
Arrhythmia is divided into two types:
| Bradycardia | slow heartbeat |
| Tachycardia | accelerated beat |
With bradycardia, the contractile system decreases to 40–60 beats per minute. This pathology is accompanied by oxygen starvation of the body and is dangerous for the development of thromboembolism.
Tachycardia is characterized by an increased heartbeat, which can reach from 90 to 240 beats per minute. The main complication of tachycardia is cerebral hemorrhage - stroke.
Cardiomyopathy accompanied by arrhythmias has the following symptoms:
- frequent dizziness;
- darkening of the eyes;
- fainting;
- rapid breathing or shortness of breath;
- heart sinking;
- constant weakness;
- chronic fatigue;
- numbness of the arms and legs (bradycardia);
- pale skin;
- chest pain;
- insomnia;
- rapid heartbeat (tachycardia);
- mood swings;
- decreased performance.
Treatment of arrhythmias occurs with the help of antiarrhythmic drugs, which must be taken for cardiomyopathy.
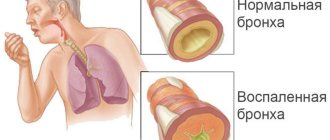
Pulmonary edema
A similar syndrome appears due to stagnation of blood in the pulmonary circulation. Typically, fluid accumulation in the lungs is observed with cardiomyopathy localized in the left side of the heart.
Pulmonary edema in cardiomyopathy occurs shortly after the development of heart failure. If the latter is not detected in a timely manner and treatment is not started, then the disease becomes stagnant, which provokes swelling of the lungs.
Clinical manifestations of fluid in the lungs change their intensity as the pathology progresses. At the initial stages of development, the symptoms do not cause severe discomfort, which cannot be said about the later stage of swelling.
Signs of pulmonary edema as it progresses:
- cough with sputum (foam or mucus);
- wheezing when breathing;
- dyspnea;
- rapid breathing;
- difficulty inhaling and exhaling (in later stages);
- cyanosis of the skin;
- cold sweat;
- swelling of the venous arteries.
With excessive accumulation of fluid, the patient practically cannot breathe, attacks of suffocation become more frequent, the pulse becomes thready, and confusion is observed. With such neglect of the disease, patient survival is significantly reduced.
Restrictive cardiomyopathy
This type of disease has a primary or secondary nature of heart damage.
This rare disease of the myocardium (and, in rare cases, the endocardium) manifests itself in the reduction of the chambers of the heart, without thickening the walls and impairing the diastolic function of the ventricles. The size of the heart does not increase, or only minor changes occur. One or both atria are enlarged. The appearance of fluid is often observed in the pericardial cavity. In the systemic circulation, blood stagnation occurs in the veins; even with minimal physical activity, shortness of breath and weakness, swelling appear, tachycardia and paradoxical pulse appear. Cardiohemodynamics are disrupted (the elastic stiffness of the ventricles increases sharply), as a result of which the intraventricular pressure in the veins and pulmonary artery increases sharply.
Hydropericardium: causes, signs, diagnosis, treatment
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day.
Normally, between the parietal and visceral layers of the pericardium there is about 15-50 ml of clear yellowish liquid, which ensures constant hydration and normal functioning of the cardiac membrane. An increase in the volume of pericardial fluid can be caused by diseases accompanied by hemodynamic disturbances, edematous, hemorrhagic syndrome, as well as tumor processes. As a result of increased vascular permeability and impaired absorption in the pericardial leaves, from 150 to 300 ml (sometimes up to 1 l) of non-inflammatory transudate can accumulate in the pericardial sac. It contains a small amount of endothelial cells, some protein, traces of fibrin and other blood cells. Cardiologists call this pathology hydropericardium.
An increase in the volume of transudate in the pericardium is often provoked by edematous syndrome, which can be observed with:
Our readers successfully use ReCardio to treat hypertension. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
- congenital diverticulum of the left ventricle;
- heart failure;
- kidney pathologies;
- stagnation;
- with direct communication between the peritoneal and pericardial cavities;
- inflammatory diseases;
- allergic reactions;
- injuries;
- anemia;
- exhaustion;
- anorexia.
In more rare cases, hydropericardium is provoked by tumors of the mediastinum, myxedema, taking vasodilators or radiotherapy. Hydropericardium can also be observed in pregnant women or in the elderly (in isolated form).
The types of hydropericardium are:
- hemopericardium: accumulation of blood in the pericardial sac, which can be provoked by rupture of an aneurysm of the heart or vessels located in the pericardial cavity, myocardial infarction, trauma, severe cardiac obesity, etc.;
- chylopericardium: accumulation of milky fluid in the pericardial sac, caused by the formation of a fistula between the pericardial cavity and the thoracic duct, trauma and compression of the thoracic duct by a tumor.
When a large amount of fluid accumulates in the pericardium, the patient develops signs of cardiac dysfunction, which are caused by compression of the heart and difficulty in its functioning:
- constant shortness of breath;
- discomfort in the chest (when bending forward);
- chest pain;
- attacks of suffocation;
- swelling of the lower extremities;
- puffiness of the face and hands;
- decrease in systolic pressure;
- increased heart rate;
- increased venous pressure.
When listening to heart sounds, their weakness and deafness are noted. In the area of the jugular veins, they are depressed and overflowing.
If the pericardial cavity is significantly overfilled, cardiac tamponade may develop, that is, its chambers cannot relax normally and pump the required volume of blood. The patient develops acute heart failure:
- increasing weakness;
- heaviness in the chest;
- severe shortness of breath;
- fear of death;
- profuse cold sweat;
- psychomotor agitation;
- tachycardia;
- a sharp decrease in blood pressure (even to the point of fainting);
- shallow and rapid breathing;
- increased venous pressure;
- dullness of heart sounds.
Without immediate medical attention, cardiac tamponade can lead to acute heart failure, shock, cardiac arrest, and death.
Hydropericardium in the fetus
The development of hydropericardium in the fetus is caused by intrauterine disruption of the development of the left ventricular myocardium. This pathology leads to diverculitis: protrusion of the wall of the left ventricle at the apex of the heart. Fluid accumulates between the pericardial layers, and this impedes the functioning of the fetal heart and can provoke tamponade.
To prevent this congenital malformation of the heart of the unborn child, a pregnant woman needs constant monitoring by a doctor and fetal cardiography. In some cases, spontaneous disappearance of fluid from the pericardial cavity is possible, but more often it is necessary to perform pericardiocentesis (pericardial puncture) in the fetus. This manipulation is difficult to perform and is performed under ultrasound control, since it is accompanied by a high risk of injury to the fetus and the expectant mother.
Diagnostics
A plain chest x-ray shows signs of fluid accumulation in the pericardial cavity.
To identify hydropericardium, the doctor needs to collect a medical history and conduct a series of diagnostic examinations:
- Echo-CG;
- chest x-ray;
- clinical urine and blood tests;
- blood chemistry.
The most informative diagnostic method for this pathology is Echo-CG. During this procedure, the doctor determines the size of the discrepancy (separation) between the parietal and visceral layers of the pericardium. Normally it should not exceed 5 mm. Based on this parameter, the doctor can draw conclusions about the stage of hydropericardium:
- initial – 6-10 mm;
- moderate – 10-20 mm;
- pronounced - more than 20 mm.
A quantitative assessment of the volume of transudate is also carried out:
- minor – up to 100 ml;
- moderate – up to 500 ml;
- large – more than 500 ml.
When the pericardial layers are separated by more than 20 mm, the patient must undergo a pericardial puncture under the control of Echo-CG or radiography. The transudate shows signs of its difference from exudate:
- relative density – less than 1.016;
- protein level is less than 1-3%.
Microbiological and cytological laboratory tests of the transudate obtained during pericardial puncture are also carried out.
With a small amount of fluid in the pericardial sac, patients are not bothered by any symptoms, and such hydropericardium does not require special therapy and goes away on its own. In such situations, it is necessary to identify the cause of a significant accumulation of transudate and eliminate it.
With a more significant accumulation of fluid in the pericardial layers, the main goal of treatment of hydropericardium is aimed at eliminating the primary disease and is carried out in a hospital. Individual tactics are recommended for each patient. In the initial or moderate stage with an elucidated etiology, conservative therapy with diuretics can be used, and if the pericardial layers are separated by more than 10-20 mm and the cause is unclear, the patient undergoes a pericardial puncture for diagnostic and therapeutic purposes.
Causes of primary cardiomyopathy
The reasons that provoke the development of this disease are quite different. Primary pathology is often caused by the following
factors:
- autoimmune processes that lead to self-destruction of the body. Cells act as “killers” in relation to each other. This mechanism is triggered both by viruses and by certain pathological phenomena that progress;
- genetics. At the level of embryonic development, a disturbance in the formation of myocardial tissue occurs, caused by nervousness, poor diet or smoking, or alcoholism of the mother. The disease develops without symptoms of other diseases due to cardiomyocytes acting on protein structures involved in the contraction of the heart muscle;
- the presence in the body of a large number of toxins (including nicotine and alcohol) and allergens;
- poor functioning of the endocrine system;
- any viral infections;
- cardiosclerosis. Connective fibers gradually replace cardiac muscle cells, depriving the walls of elasticity;
- previously suffered microcarditis;
- general connective tissue disease (diseases that develop with weak immunity, causing inflammatory processes with the appearance of scars in organs).
- cumulative, which is characterized by the formation of pathological inclusions in or between cells;
- toxic, which occurs when the heart muscle interacts with antitumor drugs and thereby receives damage; frequent drinking of alcohol over a long period of time. Both cases can cause severe heart failure and death;
- endocrine, which appears in the process of metabolic disorders in the heart muscle, losing contractile properties, and wall degeneration occurs. Occurs during menopause, gastrointestinal disease, diabetes;
- nutritional, arising from malnutrition during diets, fasting and a vegetarian menu.
Carrying out diagnostics
Making a diagnosis can be difficult if the patient seeks help at a district clinic, undergoes a remote examination and is not able to visit a specialized cardiac center. In order for the diagnosis to be correct, as well as to differentiate the types of cardiomyopathy, a whole range of examinations is required under the guidance of an experienced cardiologist. Diagnostic methods and their possible results are as follows:
- Physical examination - palpation, percussion, auscultation of the heart, external examination of the body. Pathological pulsation in the abdomen and neck, swelling of the legs, pale and blue discoloration of the skin, moist rales in the lungs, weakening of heart sounds, displacement of the boundaries of the heart, etc. are detected.
- ECG. There are signs of myocardial hypertrophy, various disturbances of heart rhythms, conduction, and changes in ventricular complexes. The most common arrhythmias are ventricular tachycardia and atrial fibrillation. If the ECG does not provide the necessary information, Holter monitoring is performed, during which 85% of people with cardiomyopathies detect certain types of arrhythmia.
- Ultrasound of the heart with Doppler sonography. There is thickening of the interventricular septum, changes in valve movement, and a decrease in the cavity of the left ventricle. In addition to the exact dimensions of the heart and its chambers, this technique allows us to identify hemodynamic disorders, systolic and diastolic dysfunction. Instead of an ultrasound examination, it is advisable to perform an MRI or CT scan of the heart, which gives a more complete picture of the disease.
- Chest X-ray. Dilatation, hypertrophy of the heart muscle, an increase in the overall size of the heart, taking on the shape of a ball, and congestion in the lungs are detected.
- General, biochemical blood tests, general urinalysis, blood tests for hormones. These techniques are necessary to differentiate the causes of secondary cardiomyopathy, for example, to detect electrolyte imbalances.
- Ventriculography, coronary angiography. The techniques are invasive, but with their help you can clarify the diagnosis and better examine the structure of the heart. If probing of the heart cavities is performed, this allows taking a biopsy sample for morphometry.
Cardiomyopathy. Symptoms and signs
Symptoms depend on the type of disease itself. With the development of dilated cardiomyopathy, all four cavities of the heart become enlarged and the ventricles and atria expand. As a result, the heart muscle cannot cope with the load.
Signs of DCM. Even with minimal physical exertion, shortness of breath occurs; the legs become swollen and a feeling of fatigue appears; the area around the mouth, wings of the nose, earlobes, fingers, ankles and feet become bluish.
With hypertrophic cardiomyopathy, thickening of the walls of the heart occurs, which entails a decrease in the size of the heart cavities themselves. This affects the release of blood with each contraction. Its amount is much less than necessary for normal blood circulation in the body.
Signs of hypertrophic cardiomyopathy . Tachycardia, pain in the heart area, pale complexion, constant fainting, weakness and shortness of breath appear.
With the development of restrictive cardiomyopathy, scarring of the heart muscle occurs. The heart can never relax, its work is disrupted.
Signs of restrictive cardiomyopathy. The skin becomes bluish in color, attacks of shortness of breath become more frequent, swelling occurs not only in the limbs, but also in the abdomen, and the liver increases in size.
This type of cardiomyopathy is considered the most severe and rare.
Symptoms of manifestation
There are no specific signs of these pathologies; almost all of them resemble the symptoms of other heart diseases. Almost all components of the clinical picture are caused by cardiac (ventricular) failure, which affects one or both parts of the heart. It also happens that a young man, unaware of his existing pathology and considering himself completely healthy, suddenly dies, which happens more often among athletes.
Some symptoms should necessarily make the patient think about the need to visit a cardiologist. In children, the disease manifests itself similarly, but all signs can increase at a higher rate than in adults. These include:
- Breathing disorders, especially shortness of breath, which can lead to attacks of suffocation. Shortness of breath most often appears after physical exertion, during stress, and as the disease progresses against the background of stagnant processes in the pulmonary circulation, shortness of breath is detected even at rest.
- Cough, which is also caused by damage to the left side of the heart. The more the left ventricular ejection fraction decreases, the more frequent the attacks of wet cough and wheezing in the chest become. When there is pulmonary edema from the respiratory tract, the patient develops foamy sputum when coughing.
- Heart rhythm disturbances and increased palpitations. Often this symptom accompanies hypertrophic cardiomyopathy. The patient may experience a feeling of a strong and loud heartbeat in the chest, as well as pulsating blood in the neck or upper abdomen.
- Pale skin. This symptom is also associated with a drop in ejection fraction, as less blood flows to the tissues. Paleness is often accompanied by blueness of the nail plates, fingertips, as well as excessive coldness of the extremities.
- Swelling. As a rule, it is noticeable in the lower extremities and is more characteristic of damage to the right side of the heart. Swelling can be detected in the evenings, and after a night's rest it goes away. In advanced stages of congestive heart failure, swelling can be almost constant.
- Pain in the chest, in the region of the heart. Since in advanced stage cardiomyopathy oxygen starvation of myocardial tissue develops, ischemia occurs, which manifests itself as chest pain. As a rule, the pain is identical to that of an angina attack.
- Dizziness and other cerebral symptoms. They are caused by hypoxia of brain tissue associated with a decrease in blood output. For the same reason, a person’s blood pressure may drop, he can suddenly lose consciousness, constantly experience weakness, and his performance is impaired.
- Enlargement of the peritoneal organs - liver and spleen. Congestive heart failure also leads to this phenomenon. The patient experiences discomfort in the liver area, as blood accumulates in the vena cava, which leads to swelling and stagnation in the peritoneum.
Almost all patients with dilated cardiomyopathy develop heart failure, which is aggravated by atrial fibrillation. Death can occur within 5 years, which is almost inevitable in 70% of patients without regular courses of treatment. Hypertrophic cardiomyopathy has a more favorable prognosis and can often be successfully corrected with surgery. The most serious prognosis and severe complications are observed with restrictive cardiomyopathy - arterial and pulmonary thromboembolism, fatal arrhythmias, and a high risk of early onset of sudden death syndrome.
Treatment
Treatment methods are relatively the same, focused on eliminating the underlying disease.
The specialist can prescribe a course of therapy that will support the overall functioning of the heart, slow down further development and improve the condition of the myocardium. The patient needs constant monitoring by a cardiologist, periodic hospital treatment and adherence to the rules of a healthy lifestyle (moderate physical activity, proper nutrition, giving up bad habits, etc.).
Therapeutic treatment directly depends on the stage of development of the disease. If this is a primary disease, it is necessary to restore the normal functioning of the heart muscle and exclude heart failure. In case of a secondary disease, the main task is to treat the underlying disease. For example, when an infection occurs, antibiotics and anti-inflammatory drug treatment are initially prescribed. And only after this is the restoration of heart activity.
If the disease is too advanced, surgery (heart transplantation) is required. Surgery to treat cardiomyopathy is relatively rare. It is used only in the case of a secondary form of the disease, when eliminating the primary disease. An example is heart disease.
Cardiomyopathy in childhood
If a child is diagnosed with dilated myopathy, then in most cases the prognosis is unfavorable. Only 50% of patients survive five years after diagnosis. If the child is diagnosed with hypertrophic or restrictive myopathy, in this case the prognosis is more positive. The mortality rate is only 2–5%. Moreover, children die from heart failure, and children of older adolescence from sudden arrhythmia (heartbeat disturbance), which is a consequence of heart pathology.
If a child is diagnosed with tonsillogenic myocarditis (a consequence of rheumatism), the prognosis is relatively favorable against the background of constant drug correction.
Preventive measures
It cannot be said that there is a special method that can reduce the likelihood of developing dilated cardiomyopathy to zero. If there is a genetic predisposition in the family, then, of course, it is necessary to undergo an annual cardiac examination.
Often, those who have had cases of the disease among their relatives are advised to give up professional sports and are not advised to choose a profession where they will have to deal with increased physical stress on the body.
The most basic preventive measures, like any other disease, are no different in the case of cardiomyopathies of all types. It is necessary to completely abandon bad habits, follow a sleep and rest schedule, and receive a healthy and balanced diet.
With the achievements of modern medicine, dilated cardiomyopathy is not a death sentence. Of course, this is a very unpleasant diagnosis, but timely treatment of the disease can significantly reduce the risk of sudden death. The main thing is to seek medical help at the first unpleasant symptoms of the heart. Otherwise, when the disease begins to develop and enters an advanced stage, there is a high risk of ending up on the operating table.
However, even in the most terrible scenarios, it is possible to prolong life through competent surgical intervention. The five-year survival rate for patients diagnosed with dilated cardiomyopathy averages 80 percent. If you follow all the instructions of a qualified attending physician, lead a correct lifestyle and have the necessary psychological attitude, then it is quite possible to maintain a decent quality of life.
Version: MedElement Disease Directory
Causes and classification
Primary cardiomyopathies are caused by various causes, the nature of which cannot always be established. These include the following cardiomyopathies:
- dilated (or stagnant);
- hypertrophic;
- restrictive;
- arrhythmogenic dysplasia of the right ventricle.
Among the possible reasons for the development of such pathologies of the heart muscle, scientists highlight the following:
- muscular dystrophy;
- gene mutations;
- genetic predisposition;
- hemochromatosis;
- autoimmune diseases;
- fungi, viruses, bacteria;
- Loeffler's disease;
- malignant neoplasms;
- sarcoidosis;
- amyloidosis;
- pathological conditions during pregnancy;
- poisoning with nicotine, alcohol, drugs, etc.
Secondary cardiomyopathies are caused by various lesions of the heart muscle during certain diseases: diabetes mellitus, thyrotoxicosis, frequent stress, hypertension, myocardial infarction, storage diseases, toxic lesions, etc.