Gynecological screening is a comprehensive examination for women that is recommended once a year. Diagnostics makes it possible to assess the state of the reproductive and reproductive systems, to ensure the prevention of pathological processes and oncological diseases. If pathologies are detected, the doctor will be able to begin treatment on an individual basis in a timely manner.
In our clinic, screening is carried out on an outpatient basis; hospitalization is not required. Depending on age, the presence of chronic diseases, and the general condition of the body, the doctor recommends a specific examination program.
Indications for use
There are a number of symptoms for which thyroid screening is a mandatory procedure.
- Bad feeling. If the patient has an unusual body temperature (high or low), if he feels constant fatigue, weakness, if there is decreased performance, and the person gets tired quickly.
- Changes in mental state. In particular, disturbances in the functioning of the thyroid gland can be accompanied by disorders, attacks of causeless aggression that cannot be kept under control, as well as attacks of groundless fear and even despair. There may be constant irritability and nervousness.
- Changes in the operation of the reproductive system. In women, this manifests itself in the form of failure of menstruation or its complete absence, in men – in sexual impotence. Both sexes can experience a lack of sexual desire.
- Weight change. Screening is needed if, under normal conditions (absence of stressful situations, usual physical activity and nutrition), a person suddenly gains or loses a lot of weight.
- Changes in the condition of hair and nails. Nail plates become weak, brittle and flaking, hair becomes thinner and begins to fall out or turn gray prematurely.
- Disorders of the cardiovascular system. The thyroid gland can affect the functioning of the heart, so you should listen to the following symptoms: uncharacteristic pressure, persistently fast or rare pulse, impaired vascular tone.
- Hearing and vision impairment. This includes painful reactions to bright lights or loud noises (they may not have seemed as bright or loud before).
If a person has symptoms of at least one of these points, then this is a signal that the functioning of the thyroid gland is impaired, and you need to go to the hospital as soon as possible.
Elderly women should be screened regularly, since the thyroid gland reacts very sensitively to all changes in hormone levels.
Pregnant women are prescribed this examination to monitor the progress of pregnancy.
Every patient undergoes this examination if they suspect thyroid cancer.
Hormonal screening for maintaining health in men
We believe that all men over 50 years of age should undergo hormonal screening to detect age-related androgen deficiency, since early diagnosis and early treatment prevent the development of quite serious complications, among which the most serious danger is cardiovascular disease and osteoporosis. Moreover, it would be ideal to have a so-called hormonal passport, which would contain data on testosterone levels at 30 years of age, which would make it easy to determine the percentage of decrease in testosterone secretion in a particular man at 50 years of age and older.
Objectives
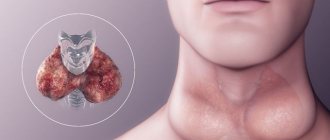
The purpose of a screening examination is to obtain reliable information about the condition of the thyroid gland in order to confirm or refute the presence of the disease, as well as to assess the general condition of the thyroid gland. This procedure makes it possible to identify autoimmune diseases of the gland (when the body perceives its own cells as foreign and begins to fight them).
The most common among them are autoimmune thyroiditis (or Hashimoto's thyroiditis) and diffuse toxic goiter (Graves' disease). Autoimmune diseases disrupt the synthesis of hormones necessary for the body to function, so it is important to identify them as early as possible.
Screening is carried out to diagnose disorders of hormone production and to monitor the progress of treatment of the organ.
Thyroid hormone test
- TSH. This hormone from the pituitary gland directly affects the thyroid gland and ensures complete circulation of other elements. The norm for a healthy person is from 0.4 to 4 mU/l. Elevated values indicate adrenal insufficiency, severe non-thyroid pathology, resistance to such hormones, neuropsychic agitation or drug use, in particular morphine. A reduced value means increased cortisol levels, thyrotoxicosis, excessive hormone therapy.
- T3 in free form . Provides metabolic activity and has feedback on the work of the pituitary gland. Normal values are from 2.6 to 5.7 pmol/l. Elevated values – peripheral vascular resistance syndrome, hormonal toxicosis or hyperthyroidism, taking methadone, amphetamine. Reduced value - peripheral vascular resistance syndrome, renal failure, disalbuminemic hyperthyroxinemia, fasting, taking iodine-containing drugs, dexamethasone, coumarin, phenytoin, artificial thyrotoxicosis, as well as a physiological decrease in the level in the summer.
- T3 general . Thyroid hormone in the serum state, responsible for the peripheral functioning of the glands. Normal values are from 1.3 to 2.7 nmol/l. An increase in the indicator indicates pregnancy, HIV infection, hepatitis, porphyria, hyperproteinemia, taking tamoxifen, oral contraceptives, amiodarone, amphetamine, and estrogens. Decreased – acromegaly, TSH deficiency, gastrointestinal, liver and kidney diseases, fasting, hemolysis, somatic pathologies, taking testosterone, anabolic steroids, caffeine.
- T4 is free . The main thyroid hormone is responsible for the functioning of transport proteins and maintains their balance in the body. The norm for a healthy person is from ten to 22 pmol/l. Elevated values indicate lipemia, mental or somatic diseases, adrenal insufficiency, taking aspirin, amiodarone, furosemide, or a hereditary increase in TSH. Reduced values – intense physical activity, pregnancy, fasting, autoantibodies with thyroid hormones, taking methadone, salicylates, triiodothyronine, rifampicin.
- T4 general . One of the main thyroid hormones. Normal values are from 58 to 161 nmol/l. An increase indicates obesity, pregnancy, acute hepatitis, intermittent porphyria, HIV infection in the inactive phase, hyperbilirubinemia, taking contraceptives, tamoxifen, heparin, thyroid drugs. Reduction - physical activity, fasting, acromegaly, congenital TSH deficiency, somatic pathologies, gastrointestinal and kidney diseases, taking testosterone, liothyronine, diphenyl, salicylates, anabolic steroids.
- TSG . This glycoprotein from the polypeptide chain is considered the third main binding carrier protein and functional element of the thyroid gland. Normal values are from 259 to 573.5 nmol/l. Elevated values are diagnosed with hyperproteinemia, pregnancy, hepatitis in the acute phase. A decrease indicates somatic pathology, ovarian hypofunction, high levels of catabolism, acromegaly, and congenital hormone deficiency.
- Antibodies to thyroglobulin . They are a useful indicator for identifying a number of problems in the body, especially after surgery. Normal values for this indicator are up to 40 IU/ml. An excess indicates perciotic anemia, Graves' disease, idiopathic myxedema, Hashimoto's thyroiditis, thyroid carcinoma, subacute thyroiditis, and other chromosomal and autoimmune problems.
- Antibodies to thyroid peroxidase . Indicator of resistance to a known enzyme. Its above-normal values indicate autoimmune diseases of the thyroid gland. The normal value of the parameter is up to 35 IU/ml.
- Thyroglobulin . The hormone, consisting of 2 subunits, is produced exclusively by the thyroid gland and is analyzed as a marker of various neoplasms, as well as a kind of “monitor” of the condition of a patient with a removed gland or a person undergoing radioactive iodine therapy. The norm is from 1.7 to 56 ng/ml. A decrease in the indicator indicates a deficiency in the productive function of the thyroid gland in relation to this hormone in hypothyroidism. An increase indicates a benign adenoma, thyrotoxicosis, subacute thyroiditis, as well as primary manifestations of thyroid cancer.
Preparation stage
In order for the test results to be correct, it should be taken into account that certain factors may influence the screening. What to do to avoid this:
- A few days before the procedure, the patient should stop taking hormonal medications. This may affect hormonal levels in the blood, which will directly affect the reliability of the analysis;
- do not drink alcoholic beverages or smoke on the day of the procedure (even better – the day before);
- try to avoid emotional and physical overload, stop playing sports, and it is recommended to spend the last 20-30 minutes before blood sampling in a calm, relaxed state;
- Screening is best done in the morning and always on an empty stomach. The only liquid you can drink is water.
What can affect the analysis results:
- acute pathological diseases;
- old age (from 80 years);
- for pregnant women - the first trimester;
- if seven days before donating blood the patient underwent a radioisotope examination.
How is the procedure performed?
The thyroid hormone screening procedure consists of several stages:
- examination and examination of the organ, including palpation;
- determination of hormone levels using a hemotest;
- screening is almost always complemented by an ultrasound examination, which will help detect inflammation, changes in the size of the cervical nodes or the appearance of a tumor.
For analysis, blood is taken from a vein, which is tested in the laboratory for the level of thyroid-stimulating hormone. If this indicator is normal, then there is no need for further diagnosis. If the level is abnormal, the blood is checked for the levels of hormones T3 and T4 (thyroxine and triiodothyronine).
Normal levels of hormones in the blood of a woman of reproductive age
| Hormones | Indicators |
| Prolactin | (120–500) mIU/l |
| LH | (4.0–9.0) IU/l |
| FSH | (3.5–6.0) IU/l |
| Estradiol | (228–400) pmol/l |
| Progesterone | (20–90) nmol/l |
| Testosterone | (1.5–2.5) nmol/l |
| DHEAS | (1.3–6.0) nmol/l |
| Cortisol | (200–400) nmol/l |
| TSH | (0.4–4.0) mIU/l |
| General T3 | (1.4–2.8) nmol/l |
| General T4 | (77–142) nmol/l |
| Free T3 | (1.0–1.7) nmol/l |
| Free T4 | (100–120) nmol/l |
| AT to thyroid peroxidase, AT to thyroglobulin |
An ACTH test is effective for detecting latent adrenal hyperandrogenism. First, the initial level of cortisol and 17OP are determined. Blood for this is taken in the morning at 9 o’clock. Then an intravenous injection of synactendepo (1 mg/ml) is given. Nine hours later, blood is taken again. The indicators of both analyzes are processed using the discriminant function, which is calculated using the following formula:
D=0.052 [X1]+0.005 [X2–0.018 [X3], where X1 is 17OP at 18 hours; X2 - cortisol/17OP ratio at 9 hours; X3—cortisol/17OP ratio at 6 p.m.
If D >0.069, then the sample can be regarded as positive. In this case, the woman is considered a carrier of the 21 hydroxylase gene allele.
The dexamethasone test is based on the fact that the drug is able to suppress the production of ACTH in the pituitary gland. As a result, the synthesis of androgens in the adrenal glands slows down. Note that this sample can be small or large.
The small one is carried out in this way: 5 mg of dexamethasone is prescribed every 6 hours for 3 days. Two days before the test itself, the blood is examined for the level of dehydroepiandrosterone, testosterone, and 17OP. When the course of dexamethasone is completed, wait a day and take blood for analysis again. If blood levels drop by 50%, the test is positive. This suggests an adrenal factor in the development of hyperandrogenism. If hormone levels have not dropped, we can say that hyperandrogenism is organic in nature. With a moderate decrease (up to 30%), ovarian pathology is suspected.
A large sample is recommended for patients in whom organic pathology of the adrenal glands is suspected. In such cases, dexamethasone is used at a dosage of 2 mg every 6 hours for 3 days. The hormone content is determined in the same way as for a small sample. If a negative result is obtained, there is a high probability of the presence of a virilizing tumor in the adrenal cortex.
When examining patients diagnosed with PCOS, a hCG test is used, which gives doctors the opportunity to identify the cause of increased androgen production. First, the initial values of testosterone, dehydroepiandrosterone and 17OP are determined. Then the woman is given an intramuscular injection of 4500 IU hCG. After 36 hours, blood is taken again. If the level of hormones has risen, then ovarian hyperandrogenism is diagnosed.
To assess insulin resistance, women suffering from hyperandrogenism undergo a carbohydrate metabolism study. This diagnostic procedure involves two stages. The first step is to assess your glycemic profile throughout the day. The first portion of blood is taken on an empty stomach in the morning at 9 o’clock. Then blood is taken every 3 hours, while eating the usual. It is worth noting that in the first morning blood test, both glucose and insulin levels are determined.
If the glycemic profile is within normal limits, proceed to the second stage of diagnosis. It is a standard glucose tolerance test. Before the procedure, a woman should receive up to 200 mg of carbohydrates per day for three days. There are no restrictions on drinking water. The test is performed in the morning on an empty stomach. The patient is prescribed glucose in the amount of 75 mg per 300 ml of water. After half an hour, an hour, one and a half and two hours, blood is taken for analysis.