Symptoms of cerebral hemorrhage.
The general clinical picture of stroke cerebral hemorrhage is characterized by the following symptoms.
- Hoarse and intermittent breathing.
- Irregular and intermittent heartbeat;
- Sudden, severe headache;
- "Red floaters" in the eyes;
- "Burning", red face;
- Pressure surges, sudden increases;
- Involuntary urination;
- Paleness, low skin temperature;
- Fainting or severe inhibition of all reactions.
- Vomiting that does not bring relief;
- Numbness and paralysis of the facial nerves and facial muscles;
- Violation of innervation;
- Partial paralysis of the limbs;
- Dilated pupils;
- Inability to make swallowing movements.
Hemorrhagic stroke develops rapidly, so within the first few minutes the patient may lose consciousness. Everything depends only on the location of the hemorrhage - on which parts of the brain are damaged. Therefore, a person can suddenly become deaf, go blind, lose memory, etc.
The more blood that enters the brain from a ruptured vessel, the more serious the symptoms and the more severe the consequences. Severe hemorrhage is characterized by:
- Convulsions;
- Loss of consciousness;
- Coma onset.
Rehabilitation
Rehabilitation after a hemorrhagic stroke lasts quite a long time.
The speed of recovery processes is largely influenced by the severity of the resulting disorders and the patient’s age.
Young age is more favorable from the point of view of the possibility of restoring lost functions of the nervous system, but in old age, mastering previous skills can be more problematic.
The duration of hospitalization will depend on the patient's condition; as a rule, stabilization occurs after three weeks of treatment in the intensive care unit and hospital. For patients with severe neurological disorders, the medical commission draws up an individual rehabilitation program. According to this program, further rehabilitation of the patient is carried out both in the hospital and subsequently at home.
Complete restoration of lost functions is possible only with small hemorrhages and timely assistance. In the first year of rehabilitation, the process of mastering lost skills proceeds quickly, in the second year it slows down, and by the beginning of the third year, the remaining neurological abnormalities are likely to persist for the rest of life.
Diet
After a stroke, a special diet is immediately established for the patient. This is necessary because swallowing is difficult and accompanied by painful sensations.
In this situation, a transition to liquid food is required; as the patient recovers, porridge, vegetable purees, and ground soft foods can be added to the diet. Nevertheless, a person during this period needs a balanced diet, since recovery requires strength.
Products that should be in the diet:
- broccoli, carrots, spinach, peas, asparagus (green and purple vegetables are preferred);
- fruits, dried fruits, seeds, nuts;
- grain porridges, cereals, bran;
- lean meat, lean sea fish;
- low-fat cottage cheese, kefir, low-fat cheese.
It is prohibited to consume red fatty meat, foods high in cholesterol - margarine, butter, egg yolk and others. Any alcoholic drinks, strong tea, coffee, cocoa are prohibited. Salt is allowed to be consumed in strictly limited quantities.
Physiotherapy
Performing the simplest therapeutic exercises is possible only as prescribed by a rehabilitation physician. With good recovery dynamics, physical therapy exercises can be prescribed a week after the attack. As a passive load during the acute period, a gentle massage is indicated to prevent stagnation and swelling of the legs.
Once the condition has stabilized, physical therapy is carried out. At the initial recovery stage, simulators can be used to implement a set of therapeutic gymnastics exercises; classes are conducted in a specialized rehabilitation center.
The following physical therapy exercises are suitable for home performance:
- To develop the muscles of the shoulder girdle, an exercise that is performed while sitting on a chair is suitable. On the count of “one,” you need to inhale and try to close your shoulder blades behind your back. On the count of “two” we return to the starting position.
- You need to sit on a sofa or bed so that your legs hang freely. Then start swinging your legs forward and backward, first slowly, and then for a couple of minutes with a gradual increase in speed and amplitude.
- Take a small ball or any round object (small apple, tangerine, etc.) and throw it from one hand to the other. This exercise is good for restoring coordination of movements of the upper limbs; it should be performed with an assistant.
- To restore speech, simple articulation exercises are suitable: alternately biting the upper and lower lips, curling the lips into a tube, clicking movements with the tongue, slowly reciting the alphabet.
Stroke surgery.
Brain surgery is often the only way to save life in case of hemorrhagic stroke. However, it has quite a lot of contraindications and features. So, in what scenario is surgical intervention indicated:
- For lobar and putamenal hematoma.
- With a thalamic hematoma - when the middle part of the brain is affected.
- If the volume of damage to the thalamus is more than 10 cm3, then the feasibility of surgery is assessed.
- In case of a brain stem hematoma, surgery is possible, but it is not always advisable, since such injuries are, by definition, fatal.
Brain surgery is absolutely contraindicated and inappropriate for deep coma (below 7 on the Glasgow scale), since, firstly, it can be fatal, and secondly, it may not make sense due to global irreversible brain damage.
There are also a number of relative contraindications to the operation:
- The age limit is 70 years;
- Cardiovascular diseases;
- Impaired functioning of the kidneys and liver;
- Diabetes;
What is the meaning of the operation:
Surgery for hemorrhagic stroke involves removing blood clots from the hematoma in order to prevent the negative effects of decomposing blood toxins on brain cells. The operation is also aimed at normalizing blood supply and stabilizing blood pressure. Brain tissue is practically not affected.
Types of operations.
For cerebral hemorrhage, combined operations are usually performed, combining several of the methods listed below. Their use depends on the complexity of the injuries and the post-stroke condition of the patient.
Operations are divided by target focus:
- An operation to save areas of the brain responsible for vital functions in the body.
- Operations whose purpose is to preserve and restore brain tissue, which is responsible for transmitting impulses to its cortex, as well as to the spinal cord and the whole body. Such tissue is, for example, the internal capsule of the brain, which provides neural communication between the brain centers and the cortex.
By method of operation:
- Open surgery with craniotomy.
- Surgery through a puncture in the skull, puncture removal of hematomas.
- Puncture surgery using a drainage system, through which drugs that prevent the formation of blood clots (fibrinolytics) are administered for some time after the intervention. Also, dead blood is removed through the drainage, which, thanks to the drugs, does not form into blood clots, but remains in a liquid state.
Closed brain surgery.
The open method of surgery with opening the skull and excision of hematomas is indicated only in the presence of life-threatening factors for the patient, and is the last possible means of saving it. The consequences of such operations are always very serious, and there is also the possibility of death. The indications are:
- Subcortical, thalamic hemorrhages, cerebellar hematoma and subsequent sharp deterioration in general condition. A situation where it is urgently necessary to release areas of the brain compressed by a hematoma.
- Displacement of brain stem tissue caused by putamenal hemorrhage.
Closed-type operations are performed using an endoscope: the process is visualized on the screen. Data from preliminary CT or MRI studies are correlated with a program that controls the operation of the endoscope, which allows all manipulations to be performed with maximum precision.
Surgery to remove intracerebral hemorrhage:
Forecasts.
Even the most experienced doctors with many years of practice behind them cannot vouch for the success of surgery for hemorrhagic stroke. However, there are a number of cases where an unfavorable outcome is most likely, namely:
- With repeated hemorrhage.
- Transverse displacement of the medulla by 8-10 mm.
- Extensive hemorrhages in the ventricles of the brain.
- Hematomas with a volume of more than 80 cm3.
Prevention
The consequences of cerebral hemorrhage are very serious. Therefore, it is necessary to take all available preventive measures to prevent the dangerous development of the pathological process:
- Eliminate provoking factors as much as possible, especially in people over 40 years of age.
- Treat hypertension.
- Get examined in a timely manner if you have frequent headaches or surges in blood pressure.
About 70% of stroke patients die for the following reasons:
- Old age (over 70 years old).
- Concomitant disorders and diseases of internal organs.
- Extensive hemorrhage and multiple hematomas.
- Brainstem stroke.
Timely treatment, long-term rehabilitation in special centers, compliance with all doctor’s orders and careful attitude towards one’s health allows the patient to survive. People who know first-hand what a hemorrhagic stroke is, in most cases remain disabled, since dead cells and brain structures cannot be completely restored.
Clinical picture
The symptoms of both strokes are similar, which causes some diagnostic difficulties. But since the pathogenesis of the diseases is radically different, differential diagnosis can be made based on clinical signs. In hemorrhagic stroke, central nervous system disorders of the type of irritation will predominate; in ischemic stroke, by the type of prolapse.
Ischemic stroke
Ischemic stroke differs from hemorrhagic stroke in its gradual onset. Patients feel general weakness, nausea, and headache. Over time, these symptoms increase and are accompanied by focal signs of brain damage. Their severity depends on the location and extent of the affected area. Often attacks occur during sleep. In this case, the patient wakes up with a full clinical picture of the disease.
Since the pathogenesis is based on ischemia and necrosis of neurons, external manifestations consist in loss of central nervous system functions. Patients complain of absence or decreased sensitivity, weakness in the limbs, and impaired motor functions. Upon examination, facial asymmetry is determined - the patient cannot smile widely or push his tongue forward. Skin and tendon reflexes are weakened. The function of the limbs is impaired by the type of paresis or paralysis.
Hemorrhagic stroke
The onset of a hemorrhagic stroke is abrupt. The clinical picture develops after exposure to one or more unfavorable factors:
- severe stress;
- lifting weights;
- excessive physical activity;
- overwork.
In some cases, the appearance of symptoms is preceded by a so-called aura - hot flashes, redness of the face, severe headache, flashing red spots in front of the eyes and seeing objects in red.
Patients clearly indicate a sudden attack of headache. It is so strong that the patient can lose consciousness.
The general condition of the patient is severe - noisy breathing, cold sweat, heavy heartbeat, excessively high blood pressure. The patient's gaze is often turned towards the lesion. Sometimes the pupil is dilated on the same side. As with ischemic stroke, when the corresponding areas of the brain are affected, facial asymmetry, impaired motor functions of the limb, and decreased skin and tendon reflexes can be observed.
Subarachnoid hemorrhage
Sometimes hemorrhage occurs in the subarachnoid space. Then the patient complains of a sharp pain, which is compared to a hammer blow to the head and a feeling of hot liquid being spilled in the head. Initially, the pain may be localized in the affected area, but very quickly spreads to neighboring areas, the neck, and the interscapular area. At the same time, nausea, vomiting, and severe dizziness appear. In a very short time, the patient develops meningeal symptoms - stiff neck, Brudzinski's, Kernig's symptoms. Doctors check for these signs using special techniques and call this phenomenon “meningism.” Their occurrence is based on irritation of the meninges by spilled blood. Respiratory disorders and disorders of the cardiovascular system are very often associated.
Subarachnoid hemorrhage is accompanied by an attack of sudden “thundering” headache
A harbinger of the disease may be an attack of acute pain in the frontal or parietal region, dizziness.
Characteristic symptoms
The clinical manifestations of the hemorrhagic form of stroke will be determined by the location of the lesion, its scale and the period of development of the pathological process.
There are two types of symptoms - cerebral and focal.
General cerebral symptoms characterize the state of the body; their etiology is associated with an increase in intracranial pressure due to the filling of brain structures with blood. Focal symptoms belong to the category of private manifestations characteristic of damage to certain areas of the brain.
General cerebral symptoms:
- sharp and severe headache;
- depression or complete loss of consciousness (lethargy, stupor, coma, stupor);
- feeling of constant nausea, vomiting, increased salivation;
- vegetative signs - sweating, increased body temperature, change in color of the skin on the face (most often redness);
- breathing disorders (rapid, noisy, confused);
- acceleration or deceleration of heart rate;
- the occurrence of seizures, epilepsy attacks.
Focal symptoms:
- unilateral paralysis of the limbs (depending on the hemisphere where the hemorrhage occurred);
- the “nasolabial triangle” is smoothed out, asymmetry is expressed on the face - one corner of the mouth is drooping, the pupil is dilated, one eye does not close;
- specific hemispheric disorders, for example, with damage to the left hemisphere - speech disorder;
- wandering gaze, inability to make coordinated movements of the eyeballs in different directions;
- symptoms of meningeal syndrome - increased tone of the occipital muscles, detected when trying to bend the patient’s head;
- prosoparesis – paresis of facial muscles;
- decreased muscle tone, lack of tendon reflex in response to mechanical irritation;
- sensory disturbances on one side of the body opposite the affected area.
There are warning signs of hemorrhagic stroke, knowledge of which can help avoid dire consequences.
Characteristic signs of a pre-stroke condition:
- numbness occurs in the limbs, fingers and toes, half of the face or any other part of the body on one side;
- nausea and vomiting;
- decreased clarity of vision, there may be “double vision” in the eyes, or partial loss of the visual field occurs;
- disorientation in space and time;
- loss of coordination of movements, loss of balance;
- when you try to stick out your tongue or smile, there is a curvature to one side;
- a person experiences difficulties if asked to raise both hands up at once, cannot formulate a coherent sentence and does not understand what others require of him.
Recovery after brainstem stroke
The rehabilitation period after a stroke of the brainstem is more difficult than with similar pathologies of other localizations. This is due to the fact that there are difficulties in eating; you need to feed pureed food or through a nasogastric tube.
It takes a long time for motor functions and sensitivity of the limbs to be restored; to develop it, you need to use special gymnastics, massage, reflexology, and physiotherapeutic procedures.
Even after the ability to walk, residual neurological deficits and inability to focus the gaze lead to unsteadiness and dizziness, falls and serious injuries. To restore speech, you will need sessions with a speech therapist.
It takes patients at least 1.5 - 2 years to return to their previous life. But most often, complete rehabilitation cannot be achieved, despite the efforts of doctors, relatives and patients.
What is the difference between ischemic stroke and hemorrhagic stroke?
Types of stroke differ from each other not only in the pathological mechanisms of their development, but also in their clinical symptoms. The main differences between ischemic and hemorrhagic stroke, as well as subarachnoid hemorrhage, are presented in the table.
| Symptom | Ischemic stroke | Hemorrhagic stroke | Subarachnoid hemorrhage |
| Previous transient ischemic attacks | Frequently observed | Happens extremely rarely | Not observed |
| Onset of the disease | Relatively slow | Fast (from several minutes to several hours) | Sudden (several minutes) |
| Headache | Weak or absent | Very strong | Very strong |
| Vomit | Not typical except in cases of brainstem involvement | Often | Often |
| Hypertensive crisis | Often | Almost always noted | Relatively rare |
| Consciousness | May be lost | Usually lost | Usually lost instantly |
| Neck muscle stiffness | Absent | Often | Marked in all cases |
| Hemiparesis | Often from the very beginning of the disease | Often from the very beginning of the disease | Rarely and not from the very beginning of the disease |
| Dysphasia (speech disorders) | Often | Often | Very rarely |
| Early cerebrospinal fluid analysis | Usually colorless | Often bloody | Always bloody |
| Retinal hemorrhage | Absent | May be | May be |
How can I help you
The life of a person who suddenly has an attack depends on the actions of others:
- They try to position the patient so that the head rises above the level of the body.
- Constrictive clothing (belts, shoes, collar, cuffs) should be removed or undone.
- When vomiting, turn the head to the side so that the victim does not suffocate or choke.
- It is necessary to provide access to oxygen - open the windows, turn on the air conditioner or fan.
Ischemic and hemorrhagic stroke mechanisms of occurrence and course of diseases
Ischemic stroke occurs due to insufficient blood supply, and, accordingly, malnutrition of certain parts of the brain, which can happen when the carotid artery, which carries the bulk of the blood to the brain, is blocked by atherosclerotic plaques. In addition, the development of ischemia may be due to cardiac arrhythmias or problems in the hemocoagulation system.
The occurrence of a hemorrhagic stroke, on the contrary, is associated with excessive blood flow into the brain, the increased pressure of which leads to rupture of the artery. This disorder can be caused by congenital vascular pathologies, but most often – by a hypertensive crisis (a critical increase in blood pressure). Therefore, treatment of hypertension is the best prevention of stroke.
Ischemic and hemorrhagic stroke differ not only in the mechanisms of occurrence, but also in the course of the pathology itself.
Ischemia is characterized by gradual development: from several hours to days. A hemorrhagic stroke occurs instantly - a sudden intense headache and loss of consciousness appear. However, both forms of stroke may have similar clinical manifestations: tingling and numbness of one half of the body or face, for example: fingers of the right or left hand, right or left half of the tongue, lower or upper lip. In addition, severe sharp pain in the eye and blurred vision may occur. The patient may have difficulty maintaining balance or difficulty understanding or pronouncing words. Afterwards, paralysis may develop.
Diagnostics
Additional examination will confirm the diagnosis and identify a pathological focus in the brain tissue.
If contact with the patient is not broken, the doctor begins the diagnosis by interviewing the patient or his relatives. During the conversation, the doctor learns about the manifestations of the disease and the time of its onset, and also gets acquainted with the anamnesis and life history.
The interview is followed by an examination, checking sensitivity and pathological reflexes, measuring blood pressure, pulse and respiratory rate, and temperature.
Next, a clinical and laboratory (general and biochemical blood tests, coagulogram parameters) and instrumental (MRI, CT of the brain, ECG, ultrasound of blood vessels, angiography, lumbar puncture with a study of the composition of the cerebrospinal fluid, EEG, radiography of the skull) examination of the patient is carried out.
After the manipulations, differential diagnosis is carried out for the presence of other diseases and a clinical diagnosis is made with complications and concomitant pathologies (if any).
Ischemic and hemorrhagic stroke. Differences
Doctors at the Yusupov Hospital make a diagnosis of stroke based on a thorough examination of the medical history, identification of risk factors and analysis of neurological symptoms. Hemorrhagic and ischemic stroke have different symptoms. Manifestations of acute cerebrovascular accident depend on its nature and location of the pathological focus.
Focal neurological symptoms of stroke are manifested by the occurrence of the following disorders:
- motor (complete and incomplete paralysis of one, two or four limbs, pathologically sudden involuntary movements in the limb, dysfunction of the cranial nerves);
- speech (impaired pronunciation, difficulty or inability to pronounce words while maintaining the pronunciation of individual sounds and understanding speech, impaired understanding of speech while maintaining the ability to speak);
- sensitive (abnormally low sensitivity to pain, lack of ability to distinguish between cold and heat, impairment of deep and complex types of sensitivity;
- coordinator (vestibular or cerebellar violation of the coordination of movements of various muscles in the absence of muscle weakness, loss of the ability to stand and walk);
- visual (the appearance of a blind spot in the visual field, not associated with its peripheral boundaries, bilateral blindness in half of vision, partial or complete blindness, not accompanied by visible damage and deficiencies of the organ of vision itself);
- cortical functions (astereognosis, apraxia);
- memory (time disorientation, fixation amnesia).
General cerebral symptoms are manifested by a decrease in the level of wakefulness from subjective feelings of “vagueness,” “fogginess” in the head and mild stupor to deep coma, headache and pain along the spinal roots, nausea and vomiting.
Neurologists at the Yusupov Hospital identify meningeal symptoms in stroke patients:
- tension in the posterior cervical muscles;
- positive symptoms of Kernig, Brudzinsky - lower, middle, upper, and ankylosing spondylitis.
For hemorrhagic and ischemic strokes, there are no symptoms unique to this type of circulatory disorder. Neurologists at the Yusupov Hospital take into account the following combination of signs to make a diagnosis of hemorrhagic stroke:
- the presence of high blood pressure and evidence of previous hypertensive cerebral crises;
- acute onset of the disease, often in the morning or afternoon, during vigorous activity;
- rapidly progressive deterioration of the patient's condition;
- development of coma in the first minutes or hours of the disease;
- the predominance of general cerebral symptoms over focal ones;
- severe autonomic disorders (pallor or flushing of the face, increased body temperature, sweating, greasiness of the skin;
- early onset of symptoms caused by displacement and compression of the brain stem.
At the onset of the disease, single or repeated vomiting and a generalized convulsive seizure are possible.
The following signs are characteristic of an ischemic stroke:
- data that the patient suffers from coronary heart disease, diabetes mellitus, suffered a myocardial infarction or transient ischemic attack;
- slow progression of symptoms of acute cerebrovascular accident;
- development of an acute disorder;
- the predominance of focal symptoms over cerebral manifestations.
The disease debuts against the background of normal or low blood pressure numbers. Can an ischemic stroke turn into a hemorrhagic stroke? This is possible if, against the background of high blood pressure in patients suffering from ischemic stroke, a cerebral artery ruptures.
Sources
- https://motusauto72.ru/ishemicheskij-i-gemorragicheskij-insult/
- https://www.aif.ru/health/life/41918
- https://www.neboleem.net/stati-o-zdorove/18499-vidy-insulta-chem-otlichajutsja-ishemicheskij-i-gemorragicheskij-insult.php
- https://GolovaLab.ru/insulto/prichiny_diagnostika/ishemicheskij-i-gemorragicheskij-insult-razlichiya.html
- https://yusupovs.com/articles/neurology/vidy-insulta-ishemicheskiy-i-gemorragicheskiy/
Risk group
A tendency to acute disorders associated with cerebral hemorrhage is observed with:
- Obesity.
- Hypertension.
- High cholesterol.
- Low white blood cell count.
- Poor nutrition, fasting.
- Constant consumption of fatty foods.
- Abuse of alcohol and smoking.
- Stress, overwork, depression.
- Diabetes mellitus.
- Chronic heart disease.
- Genetic predisposition.
Causes and mechanisms of stroke development
The cause of ischemic stroke is a violation of blood flow through the arteries of the brain. Most often, doctors observe 2 types of ischemic stroke - embolic, caused by embolism from a distant source, and thrombotic, which developed as a result of primary blockage of cerebral vessels by a thrombus. Primary thrombotic blockage usually develops in a vessel whose lumen is narrowed as a result of atherosclerosis. The most common source of embolism is the heart.
Cardiogenic embolism can occur with atrial fibrillation or myocardial infarction, with infective endocarditis, myxoma (a benign tumor growing into the lumen of the atrium). It occurs in patients with prosthetic heart valves. Less commonly, the source of emboli is ulcerated atherosclerotic plaques located at the mouth of the great vessels and the aortic arch.
Atherosclerosis of the carotid artery can be the cause of its primary thrombotic occlusion, but more often it is the source of embolism of the intracranial arteries. With an ischemic stroke, an infarction of a region of the brain develops, around which there is a zone in which nerve cells have not died and, with timely treatment, can restore their function.
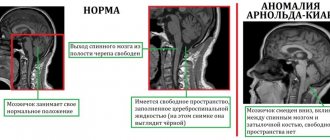
Hemorrhagic stroke develops as a result of a violation of the integrity of the cerebral arteries, the release of blood from the vessel and compression of the brain substance. Its cause is high blood pressure, congenital or acquired anomalies in the structure of the cerebral arteries. A primary hematoma is a relatively large, homogeneous collection of blood that occupies a certain volume and causes cell destruction, displacing and destroying the surrounding brain tissue. Infarction-hematoma manifests itself as a homogeneous focus of high density, shaped like a lake. Hemorrhagic infarction is characterized by blood permeation of ischemic brain tissue without displacement or destruction of brain cells.
Causes
The main cause of the pathological process is reduced strength and elasticity of blood vessels. The loss of their flexibility is associated with:
- Hypertension. Both sudden jumps in blood pressure and its consistently high level are scary.
- Vascular deformations of acquired or congenital nature (dissection, protrusion, abnormal plexus of veins or arteries).
- Atherosclerosis. The walls of the cerebral arteries become weak and thinned due to cholesterol plaques accumulated on them.
- Dystrophic vascular changes against the background of inflammation due to encephalitis, cerebral vasculitis, toxic poisoning, systemic lupus erythematosus.
- Poor blood clotting caused by hemophilia or overdose of blood-thinning medications.
- Tumors that compress tissues and brain structures that impede blood circulation.
Treatment.
When talking about the treatment of hemorrhagic stroke, one should take into account the fact that a cerebral hemorrhage has already occurred, and the process of tissue damage and death occurs very quickly in this situation. If the process of an ischemic stroke from the beginning to the final stage takes on average several days, due to which doctors have enough time to eliminate and treat it, then in the case of a cerebral hemorrhage, speed and time play a decisive role. The sooner the ambulance arrives, the sooner a diagnosis is made and treatment begins, the greater the patient’s chances of surviving and even recovering from surgery. The actions of doctors must be clear and coordinated, decisions must be made quickly, and in this case doctors have no right to make mistakes.
Surgical intervention.
In case of extensive hemorrhages and a number of the above indications, surgery is prescribed to remove brain hematomas. The hematoma must be removed in the first two days, since coagulated blood not only impedes the work and nutrition of the brain, but, when decomposed, causes inflammation, swelling and necrosis of surrounding tissues. The faster the hematoma is eliminated, the higher the chance of survival and recovery.
Conservative therapy.
Small hemorrhages do not require surgical intervention and are eliminated through conservative therapy. However, neurosurgical treatment should be used in combination with it.
The therapy is aimed at alleviating and eliminating a whole range of disorders and damage in the body caused by a stroke.
- Correction of blood pressure.
To correct and stabilize it, ACE inhibitors, beta blockers and antispasmodics are prescribed. The pressure is brought back to normal in accordance with the individual characteristics of the patient’s body. As a rule, hemorrhagic stroke almost always occurs against the background of hypertension.
- Relieving cerebral edema.
The first condition for relieving cerebral edema is intensive saturation of it with oxygen and all necessary nutrients. Therefore, the patient is injected with oxygen into the lungs through an artificial respiration apparatus, inhaler or other devices.
Another important condition is the elimination of the cause of edema - hematoma, which is performed through surgery. In some cases, it is recommended to install a drainage system to pump out excess fluid
To restore blood circulation, venous and liquor outflow from tissues, vasoconstrictor and anticonvulsant drugs are prescribed. It is also necessary to eliminate all external stimuli - bright light, noise, and limit the patient’s movements. The use of painkillers also helps relieve brain swelling. It is necessary to reduce the patient's body temperature to normal. In some cases, diuretics are prescribed to drain excess fluid.
- Hemostatic therapy.
On the one hand, it is necessary to minimize the possibility of blood clots, on the other hand, to prevent the resumption of bleeding. Therefore, the damaged vessel is surgically repaired and vasoconstrictor drugs are prescribed. The administration of drugs that stimulate blood clotting is strictly prohibited.
- Sedative therapy.
This type of therapy is aimed at eliminating external stimuli and ensuring a stable emotional state of the patient - peace and sleep. Phenozepam, Elenium, and sleeping pills are prescribed.
Therapy
The sooner specialized assistance is provided to the victim, the greater the chances of his salvation. Treatment measures can be divided into 3 stages:
- Emergency medical care.
- Specialized assistance.
- Rehabilitation.
Emergency medical care
When transporting a patient to a hospital where there is an intensive care unit, specialists carry out the following actions:
- Consciousness and reflex reactions to stimuli are assessed.
- The pulse is measured and the heartbeat is studied. If necessary, cardiac massage is performed.
- Respiratory function assessment.
- In case of convulsions and vomiting, the patient is placed on his side to ensure normal breathing and free passage of saliva or foam from the mouth.
- Blood pressure is determined and adjusted. Often it is necessary to lower it.
- An ice pack is placed on the patient's head to constrict blood vessels.
Specialized assistance
Patients are placed in a department where a number of necessary measures can be performed (install an IV, connect the patient to mechanical breathing).
- The pressure is corrected by intramuscular administration of Enap, Benzohexonium, Oxybral. If the patient is able to swallow, then use Farmadipin drops, Corinfar tablets, Clonidine. For low blood pressure, non-glycoside cardiotonic drugs are used.
- If there is a breathing disorder, forced supply of the gas mixture into the lungs is required. While breathing is maintained, oxygen is supplied through a mask.
- To reduce cerebral edema, diuretics are administered.
- Nutrition of brain cells is provided by intravenous administration of Ceraxon, Actovegin, Cavinton, Piracetam.
- Hemostatic medications are used: Vikasol, Tranexam, Takhacomb.
- Blood microcirculation is supported by intravenous infusion therapy with Rheosorbilact, Cytoflavin, and Glucose.
Some cerebral hemorrhages are treated surgically. Surgical treatment is indicated for:
- Large hemispheric hematomas.
- Blood entering the anastomosing cavities of the brain.
- Aneurysm rupture.
- High intracranial pressure.
Modern neurosurgeons use the following types of operations:
- Craniotomy . In this case, a bone fragment is cut in the problem area and the accumulated blood is removed. The advantage of this type of surgery is that it reduces swelling of the brain by reducing pressure in the skull.
- Puncture intervention . The skull is punctured and the blood is sucked out under the control of high-precision equipment. This type of stroke surgery is effective for hematomas in the deep parts of the brain.
- Drainage . Tubular drains are installed in the anastomosing cavities of the brain to relieve intracranial pressure.
After surgery to remove blood from the hematoma, the pressure decreases, which significantly increases the chance of recovery.
Rehabilitation
Treatment of hemorrhagic stroke at this stage is:
- Regularly taking medications that restore neurons. They normalize dopamine levels, have a beneficial effect on the bioelectrical activity of cells, and have a specific effect on the cerebral cortex.
- Vitamin therapy and providing a weakened body with vital elements. If swallowing is preserved, then the patient is shown protein and fortified foods. If swallowing function is impaired, mixtures are fed through a probe. In the absence of consciousness, infusion therapy with amino acids is carried out.
- The body of a bedridden patient must be rubbed with camphor oil every 2 hours and its position changed to avoid bedsores.
- Antibiotics are administered to prevent infectious diseases of the respiratory system (the development of pneumonia).
- Exercise therapy, gymnastics, and massage begin after the patient’s condition has stabilized.
Types of hemorrhagic stroke.
Hemorrhagic stroke of the brain stem.
It should be noted that a brainstem stroke results in almost instantaneous death. Only in rare cases is it possible to save the patient’s life with such a diagnosis. At the same time, there is no likelihood of returning to a full life.
The brain stem is the center of all body systems and is directly connected to the spinal cord. It serves as a link between the commands of the brain centers and the nerves of the body: it is thanks to it that we are able to move, breathe, swallow, see, hear, and so on. The brain stem also regulates the circulatory system, thermoregulation, and heartbeat. That is why damage to it during a stroke most often leads to death.
Possible consequences
Hemorrhagic stroke has terrible consequences, many of them are irreversible and will become a serious obstacle to a full life. The most severe complication is coma. The survival rate in this case is only 10-15%. Coma after a hemorrhagic stroke is short-term. The exit from it is observed on 8-10 days.
The dangerous period after a stroke lasts from the first day to three weeks. At this time, the likelihood of a recurrent attack, progression of cerebral edema and increased formation of blood clots is highest.
After a hemorrhagic stroke, any of the existing disability groups (I, II, III) can be assigned. It all depends on the patient’s condition after rehabilitation and his ability to self-care. When deciding on the assignment of disability, the presence of mental pathologies, epilepsy attacks, speech disorders, movement and coordination disorders is important.
Left side lesion
A left-sided stroke disrupts the functioning of the right side of the body and face. The left hemisphere is responsible for oral, written language and mathematical abilities. They are the ones who suffer as a result of a stroke, so a person may lose the ability to read and write. Patients experience problems in situations that require step-by-step processing of information and cannot form a whole from parts. Speech memory impairments are noted. Behavior is characterized by slowness and increased caution.
Right side lesion
A right-sided stroke leads to paralysis of the left half of the body and face. A person loses the ability to navigate in time and space, he is characterized by impulsiveness, short temper, and irritability. There are disturbances when working with holistic images, three-dimensional perception, behavioral and motor (motor) memory, sense of rhythm, and imagination suffer.
Hemorrhagic stroke classification
Depending on the location of the hemorrhagic focus, a stroke can be:
- intracerebral (parenchymal);
- meningeal (subarochnoidal, epidural, subdural);
- combined (stroke of a subarachnoid-parenchymal or parenchymal-ventricular nature, ventricular (intraventricular hemorrhage, or parenchymal infarction with blood breaking into the ventricles)).
Also, a hemorrhagic stroke can be subcortical, cerebellar, brainstem, etc.
Intracerebral hemorrhagic strokes are divided into:
- lateral (the hematoma is located outside the VC (internal capsule));
- medial (the hematoma is located medially from the VC and affects the area of the 3D (optic tubercle) and supratubercle);
- mixed.
Signs of hemorrhagic stroke.
Hemorrhagic stroke occurs suddenly. It is characterized by piercing, sharp pain in the head and subsequent loss of consciousness. However, the pre-stroke state can last from several hours to several days. If you have at least a few of the following signs, this may be a signal of a pre-stroke condition and a reason to be examined by a doctor:
- Vomiting and nausea without an objective reason, which do not bring relief;
- Dizziness;
- Constant headache;
- General weakness;
- Reduced skin sensitivity;
- Numbness of the limbs;
- A rush of blood to the skin of the face, sharp redness;
- Uneven, intermittent pulse.
A sharp and acute headache and subsequent loss of consciousness are the first signs of a hemorrhagic stroke.
If the person next to you suddenly becomes ill, you should certainly call an ambulance immediately. And performing the following small test will help identify the onset of a stroke and take the first measures to save his life before the ambulance arrives:
- Smile.
Ask the person to smile: his smile will be distorted, one half of his face will remain motionless.
- Language.
Ask to show your tongue: it will be unnaturally curved in your mouth.
- Ask for a show of hands.
A person in a pre-stroke state will not be able to lift them at the same time and keep them at the same height.
- Speech.
Ask him to say his name or a simple sentence. His speech will be slurred, he will stammer, chew his words, since during a stroke part of the speech apparatus is paralyzed.
First aid for hemorrhagic stroke:
- The victim is laid horizontally, with the head positioned significantly higher than the body.
- All clothing that restricts breathing is removed.
- The head is turned to the side so that the person does not suffocate from vomiting.
- Windows are opened to provide fresh air.
- An ambulance should be called simultaneously with these activities, if possible. The faster the patient receives qualified assistance, the fewer irreversible consequences a stroke will cause.
About the signs of a stroke and subsequent rehabilitation.
What it is
In a hemorrhagic stroke, the thinned wall of a blood vessel ruptures, causing uncontrolled hemorrhage into the brain tissue. A large volume of blood can enter the brain in a short time. Its flows are destructive for neurons. They displace tissues, causing hematoma and swelling. If the patient is not given immediate assistance, tissue necrosis and death occur.
Medical care for a cerebral stroke is effective if provided no later than 3 hours after the onset of the attack. Then the process will become irreversible, and it will be impossible to eliminate complications. If such a patient manages to survive, he will remain disabled for life.
With hemorrhagic stroke the following are noted:
- Suddenness. In more than half of patients, acute circulatory disorders in the brain begin without any primary symptoms.
- High mortality rate. 70% of victims die within the first days after the development of the pathology.
- Severe disability of surviving patients. According to statistics, 80% of patients cannot move independently and become a burden for the family. The remaining 20% have pronounced deviations.
80% of cerebral hemorrhages are associated with high blood pressure. For hypertension, taking antihypertensive medications significantly reduces the risk of stroke, the amount of possible bleeding and the severity of the disease.
Coma due to hemorrhagic stroke
Disorders of consciousness are characteristic of many pathologies, manifested by inhibition of the functions of the reticular formation of the brain.
Brain dysfunctions develop under the influence of:
- Endo- and exotoxins – derivatives of the end products of metabolism;
- Oxygen and energy starvation of the brain;
- Metabolic disorders in brain structures;
- Expansion of the volume of brain matter.
The most important factors in the development of coma are acidosis, cerebral edema, increased intracranial pressure, and impaired microcirculation of brain fluids and blood.
The state of coma affects the functioning of the respiratory system, excretion (kidneys) and digestion (liver, intestines).
It is impossible to recover from a coma at home, and it is very difficult even in intensive care conditions.
The clinical definition of coma is carried out using the GCS (Glasgow Coma Scale), and some other methods that are important for clinicians are used. There are precoma and four stages of coma. The easiest is the first, and the hopeless state of the patient corresponds to the fourth stage of coma.
Brain and its membranes
The brain is located in the bony cranium, surrounded by three meninges and cerebrospinal fluid. The dura mater lines the inside of the cranial bones. The processes that form the brain sections extend from it. In certain places, the hard shell is divided into sheets that form sinuses. Venous blood flows through them. This membrane of the brain contains the maximum concentration of pain receptors in the human body.
Under the dura mater there is the arachnoid membrane and the subdural space, which is filled with serous fluid.
The second membrane, the arachnoid, covers the brain and furrows on top, but does not extend into them. It has no vascular supply and is nourished by cerebrospinal fluid. It fills the gaps between the soft and arachnoid membranes in places where the soft membrane enters the grooves of the brain (subarachnoid cisterns).
The choroid covers the grooves and convolutions of the brain. It consists of thin connective tissue with vessels branching in it. The filamentous processes of this membrane penetrate into the substance of the brain.
This is a general simplified idea of the membranes of the brain. There are a large number of diseases that interfere with its functioning.