| Angioedema | |
| ICD-10 | D 84.1 84.1, T 78.3 78.3 |
| ICD-10-CM | T78.3 |
| ICD-9 | 277.6 277.6 , 995.1 995.1 |
| ICD-9-CM | 995.1 [1] |
| OMIM | 606860 |
| DiseasesDB | 13606 |
| MedlinePlus | 000846 |
| eMedicine | emerg/32 med/135 med/135 ped/101 ped/101 |
| MeSH | D000799 |
| Media files on Wikimedia Commons | |
Angioedema,
or
Quincke's edema
, is a reaction to various biological and chemical factors, often of an allergic nature. Manifestations of angioedema are enlargement of the face or part or limb. The disease is named after the German physician Heinrich Quincke, who first described it in 1882.
Clinical picture [edit | edit code ]
The disease is manifested by the occurrence of edema in places with developed subcutaneous tissue - on the lips, eyelids, cheeks, and oral mucosa. The color of the skin does not change. There is no itching. In typical cases, it disappears without a trace after a few hours (up to 2-3 days). The swelling may spread to the lining of the larynx, which can cause difficulty breathing. In this case, there is a hoarseness of the voice, a barking cough, difficulty breathing (first exhale, then inhale), noisy breathing, the face is hyperemic, then suddenly turns pale. Hypercapnic coma occurs and then death may occur. Nausea, vomiting, abdominal pain, and increased peristalsis are also noted.
Angioedema differs from ordinary urticaria only in the depth of skin damage. It should be noted that manifestations of urticaria and angioedema may occur simultaneously or alternate.
Symptoms
The main sign of the development of angioedema is immediate swelling of body parts, which can be seen in the photo below.
The swelling can be asymmetrical and affect the face, neck, and arms. With the development of edema, no changes in skin color are observed, and there is no itching.
In most cases, in patients, swelling disappears without a trace within several hours or days.
When swelling spreads to internal organs, more serious symptoms appear. When the respiratory system is affected, hoarseness and a dry cough develop. Subsequently, signs of respiratory failure due to asphyxia appear. If the swelling has spread to the digestive organs, nausea, abdominal pain, and vomiting are felt.
Development mechanism [edit | edit code ]
An acute allergic reaction is the result of three mechanisms: allergenic, non-allergenic, combined type:
- With the allergenic mechanism, an allergen—food, medicine, pollen—invades for the first time, the body perceives it as an antigen and produces antibodies. There is an increased sensitivity to the effects of irritants. Reintroduction of the allergen destroys the cell containing the antibodies. Histamine is released and swelling develops.
- In a non-allergenic mechanism, histamine is released in response to insect venom, medication, food or olfactory stimulus.
- Congenital angioedema is a combined form. Complement proteins are present in the blood in an inactive state. A stressful situation can serve as an activator. Proteins of the complement system mistake host cells for antigens. Edema occurs [2].
Diagnostics
Diagnosis of angioedema is relatively simple. Due to its appearance, a physician should be able to recognize it after a simple physical examination and a detailed medical history.
Additional tests, such as a blood test, may be needed to accurately determine the type of angioedema.
Allergy tests may be performed to detect allergens (allergic angioedema) . Hereditary angioedema can be diagnosed by using a blood test to check the levels of proteins regulated by the C1-INH gene: very low levels confirm the presence of the disease.
Diagnosis and treatment of hereditary angioedema are highly specialized and should be performed by a specialist in the field of clinical immunology.
Angioedema may be associated with other medical problems, such as iron deficiency, liver disease , and thyroid disease, which doctors will investigate with simple blood tests (it's helpful to check for or rule out these conditions).
Idiopathic angioedema is usually confirmed by a method known as a “diagnosis by exclusion”; in practice, the diagnosis is confirmed only after various studies have been carried out to exclude any other disease or condition with similar manifestations.
First aid [edit | edit code ]
Since angioedema is a rather dangerous condition, it is important to be able to provide first aid for its manifestations.
- First of all, you need to call an ambulance.
- Immediately stop the patient's contact with the allergen if the allergen is known.
- If swelling occurs after intramuscular injection of the drug or an insect bite, then you need to apply a pressure bandage above the injection site (bite). If it is not possible to apply a bandage (for example, the injection was made in the buttock), then a cold compress or ice should be applied to the injection (bite) site. This will slow down the spread of the allergen due to vasoconstriction.
- Unbutton or loosen the patient's clothing.
- Provide the patient with fresh air.
- Try to calm the victim until the ambulance arrives.
- You can give the victim a few tablets of activated carbon dissolved in warm water.
Forecast
- Swelling of the larynx can be fatal if medical assistance is not provided on time;
- If angioedema with urticaria periodically worsens over 6 months, then the risk of their recurrent course in the next 10 years reaches 40%;
- In half of the patients with angioedema and chronic urticaria, spontaneous remission is determined;
- Both hereditary and acquired forms of the disease are considered chronic pathologies, but properly selected therapy can prevent acute attacks and significantly improve the patient’s life.
Drug treatment [edit | edit code ]
- When blood pressure decreases, 0.1-0.5 ml of a 0.1% adrenaline solution is injected subcutaneously;
- For asphyxia (swelling of the mucous membrane of the respiratory tract), adrenaline injections;
- Hormonal therapy: glucocorticoids (prednisolone 60-90 mg IM or IV; dexazone 8-12 mg IV;)
- Desensitizing treatment: antihistamines (Suprastin 2% - 2.0 IM, Claritin, Zyrtec, Erius, Telfast).
- Diuretics: Lasix 40-80 mg IV bolus in 10-20 ml saline;
- Protease inhibitor drugs: contrical - 30,000 units IV in 300 ml of saline, epsilon-aminocaproic acid 5% - 200 ml IV drip, then 100 ml after 4 hours or 4 g per os 4-5 times a day the day until the reaction is completely relieved;
- Detoxification therapy - hemosorption, enterosorption;
- Hospitalization in the allergy department.
Indications for consultation with doctors
A patient with suspected angioedema needs consultation with doctors of narrow specialties, these are:
- Dentist. If necessary, the oral cavity is sanitized;
- Gastroenterologist. Gastrointestinal pathologies are excluded;
- Otorhinolaryngologist. Patients with AO often have a high degree of fungal infections and opportunistic microorganisms in the oral cavity, and the development of edema in the larynx is typical;
- Surgeon. Consultation with this specialist is necessary for patients with abdominal syndrome;
- Oncologist. A malignant process is excluded;
- Allergist-immunologist;
- Rheumatologist. Consultation with this specialist is especially necessary if the swelling is localized in the area of the articular surfaces.
What is angioedema?
Angioedema (synonyms: angioedema, angioedema, angioedema, Quincke's edema) is an inflammatory reaction of the skin, similar to urticaria, characterized by the sudden appearance of edema in areas of the skin, mucous and submucous membranes. Symptoms of angioedema can affect any part of the body, but most commonly affect the eyes, lips, tongue, throat, genitals, arms and legs.
In more severe cases, angioedema also affects the lining of the airways and upper intestines, causing chest or abdominal pain. Angioedema is short-lived: swelling in the affected area usually lasts from one to three days.
In most cases, the reaction is harmless and leaves no trace, even without treatment. The only danger is that the throat or tongue may be damaged, as their severe swelling can cause rapid airway obstruction, shortness of breath and loss of consciousness.
Prevention
After diagnosing angioedema, the patient must undergo examination to identify the allergen that provoked such an aggressive reaction of the immune system.
In the future, a person must avoid contact with him to prevent a relapse. The list of preventive measures also includes the following:
- Following a hypoallergenic diet and proper drinking regimen.
- Maintaining an active lifestyle. It is recommended to engage in physical exercise or sports, and often take walks in the fresh air.
- Stressful situations should be avoided.
- People who are prone to allergies need to carry antihistamines with them at all times. They should be taken when the first alarming symptoms appear.
Angioedema is one of the most severe manifestations of allergies. But with the right approach to treatment and prevention, it disappears without a trace and may never appear again.
How is angioedema different from urticaria?
Angioedema and urticaria are the result of the same pathological process, so they are similar in some respects:
- Often both clinical manifestations coexist and overlap: urticaria is accompanied by angioedema in 40-85% of cases, while angioedema can occur without urticaria in only 10% of cases.
- Hives are less severe because they only affect the superficial layers of the skin. Angioedema, on the other hand, affects the deep subcutaneous tissues.
- Urticaria is characterized by the temporary occurrence of an erythematous and itchy reaction in well-defined areas of the dermis (the appearance of more or less red and raised blisters). With angioedema, on the other hand, the skin maintains its normal appearance without blisters. In addition, swelling may occur without itching.
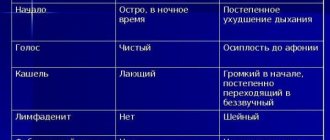
The main differences between urticaria and angioedema are shown in the following table:
Angioedema (Quincke's edema) is an acute condition characterized by the rapid development of local edema of the mucous membrane, subcutaneous tissue and the skin itself. It most often occurs on the face (tongue, cheeks, eyelids, lips) and much less often affects the mucous membranes of the genitourinary organs, gastrointestinal tract, and respiratory tract.
Angioedema is a common pathology. It occurs in every fifth person at least once in a lifetime, and in half of the cases it is combined with allergic urticaria.
Attention! Photo of shocking content. To view, click on the link.
Type of edema
Angioedema or Quincke's edema is divided according to the following criteria:
According to the course of the disease:
- acute – lasts no more than six weeks;
- chronic – lasts more than six weeks;
- combined with symptoms of urticaria;
- individual.
According to the mechanism of formation:
- due to the activity of the complement system;
- participation of other mechanisms;
- has an idiopathic form.
The hereditary form of angioedema is divided into:
- Type 1 – there is no C1 inhibitor in the body;
- Type 2 – formed when there is a lack of inhibitor;
- Type 3 – occurs with a normal amount of inhibitor.
Acquired form of angioedema:
- Type 1 – absence of C1 inhibitor.
- Type 2 – lack of inhibitor and formation of antibodies to it.
Impaired immune function and the addition of infectious diseases (fever, itchy skin, sudden weight gain, etc.).
How long the pathology lasts depends on many factors; if it is an acute form of Quincke's edema, then it goes away in less than six weeks; if it does not go away during this time, then the pathology has become chronic.
Allergic
The allergic type of angioedema occurs together with urticaria. The characteristic symptoms of this type of allergy are severe itching. May be one of the components of an anaphylactic reaction. The cause of the disease is direct contact with the allergen. It goes away in a couple of days.
Hereditary
Hereditary angioedema is in no way associated with the appearance of urticaria. A predisposing factor for hereditary angioedema is a genetic predisposition. The onset of the disease occurs in childhood. The condition usually worsens during puberty.
After physical activity
Quincke's edema occurs in a patient after severe physical exertion. Why this condition develops and what it leads to has not yet been fully established by medicine.
Causes
In most cases, angioedema is a manifestation of an immediate allergic reaction in response to allergens entering the body (poisons of stinging insects, medications, food allergens).
Once in the body, allergens trigger an “antigen-antibody” reaction, which is accompanied by the release of serotonin, histamine and other allergy mediators into the blood. These substances have high biological activity; in particular, they are capable of dramatically increasing the permeability of the walls of blood vessels located in the submucosal layer and subcutaneous fat. As a result, the liquid part of the blood begins to sweat from the lumen of the vessels, which leads to the development of angioedema, which can be both local and widespread.
Angioedema can also be a manifestation of a pseudoallergic reaction, which is based on individual hypersensitivity to certain medications or foods. But in this case, there is no immunological stage in the pathological mechanism of edema development.
To prevent recurrent allergic angioedema, the patient should adhere to a hypoallergenic diet and not take any medications without a doctor’s prescription.
Angioedema can develop as a complication of therapy with ACE inhibitors or angiotensin II receptor antagonists. This form is usually diagnosed in older people. The development of edema in this situation is based on the blockade of angiotensin-converting enzyme by drugs. As a result, the destruction of bradykinin slows down and the activity of angiotensin II decreases, which leads to persistent dilation of blood vessels and increased permeability of their walls.
Symptoms of pathology
Quincke's edema always begins with warning signs. These are preliminary symptoms manifested in the appearance of burning and tingling on the face, neck and limbs. In a third of patients, along with the appearance of warning signs, redness of the skin on the face and neck is noted.
The swelling itself begins with swelling of the mucous epithelium . Then the skin and subcutaneous tissue are affected. In this case, the color of the skin most often does not change. The photo clearly shows that swelling on the face is most pronounced: the cheeks, eyelids, and lips increase in size.
The most dangerous symptom of the disease is damage to the larynx and tongue. This causes difficulty swallowing and a sore throat. The patient's face is deformed. The tongue becomes so large that it may fall out of the mouth. The person first begins to wheeze and then choke. Against this background, acute respiratory failure .
Quincke's edema can also cause fluid to leak from the vessels into the pleural cavity. This phenomenon is accompanied by chest pain and severe cough.
If the swelling is localized in the abdominal cavity, then a characteristic symptom appears - quite severe pain in the abdominal area. They may be accompanied by nausea and diarrhea.
When the bladder is damaged, urinary retention occurs.
If Quincke's edema manifests itself in a severe form and affects the meninges, then the patient experiences a convulsive syndrome and may develop serious disturbances of consciousness.