Gangrene is a term that describes dead or dying tissue(s) of the body that occurs because the local blood supply to the tissue is either lost or disrupted. Gangrene has been recognized as a localized area of tissue death since ancient times. The Greeks used the term gangrin to describe the rotting (death) of tissue. Although many people associate the term gangrene with a bacterial infection, the medical use of the term includes any cause that, due to impaired blood supply, results in tissue death (necrosis). Therefore, a person can be diagnosed with gangrene, but does not necessarily have to be "infected".
There are two main types of gangrene: dry and wet (wet). Many cases of dry gangrene are not infected. All cases of wet gangrene are considered to be infected, almost always by bacteria. The most common sites for wet and dry gangrene are the fingers and toes and other extremities (arms, arms, legs, and feet).
What is the difference between wet and dry gangrene?
Wet (also sometimes called "wet") gangrene is the most dangerous type of gangrene because if left untreated, the patient usually develops sepsis and dies within hours or days. Wet gangrene results from an untreated (or improperly treated) infection in the body where the local blood supply has been reduced or stopped by tissue swelling, gas formation in the tissue, bacterial toxins, or all of these factors in combination. In addition, conditions that impair circulation may occur in the first place, such as burns or vascular injury (such as a knife wound that cuts off arterial flow). When germs enter the affected area, wet gangrene can occur.
Wet gangrene is the type most often understood when the term gangrene is used. Wet gangrene often produces oozing fluid or pus, hence the term "wet". Early stages of wet gangrene may include signs of infection, leg pain with swelling, reddish skin color or pale skin color if the area is elevated above the level of the heart, a feeling of coolness on the surface of the skin, the formation of ulcers, and a cracking sensation when the skin is pressed due to gas in fabrics. These stages can develop rapidly over a period of several hours.
Dry gangrene , unless it becomes infected and progresses to wet gangrene, does not usually cause sepsis or cause death in the patient. However, this can lead to local tissue death (necrosis), causing the tissue to peel off. Typically, progression of dry gangrene is much slower (days to months) than wet gangrene because vascular compromise develops more slowly. The stages are similar to wet gangrene (see above), except that there is no infection, pus, fluid, or a cracking sensation in the skin because there is no gas formation in the uninfected tissue. Dry gangrene is characterized by a cool, dry sensation and a pale area (sometimes called "mummified") without oozing fluid or pus, which is why the term "dry" is used.
Complications from other diseases
There are many diseases that can lead to dry gangrene; the most common are diabetes mellitus, atherosclerosis and tobacco addiction (smoking). Infrequently, dry gangrene can occur quickly, from a few hours to a few days, when there is rapid blockage of the arteries (for example, an arterial blood clot suddenly blocks a small artery).
Photo: Myriams-Fotos/Pixabay
What causes gangrene?
A common cause of wet or dry gangrene is the loss of effective local blood supply to any tissue. Loss of blood supply means tissues are deprived of oxygen and nutrients, leading to cell death. The most common causes of tissue loss are infections, injuries, and diseases that can affect blood vessels (usually arteries).
Cause of dry gangrene
Dry gangrene can result from any of a number of diseases or mechanisms that can reduce or block arterial blood flow. Although the most common diseases that can cause dry gangrene are diabetes, atherosclerosis and tobacco addiction, there are many other lesser-known diseases that can lead to this problem. For example, some autoimmune diseases that attack blood vessels (vasculitis syndromes) can cause enough damage to cause dry gangrene. In other cases, dry gangrene may result from various external mechanisms, such as burns, frostbite, and arterial trauma caused by accidents, wounds, or surgery.
Cause of wet gangrene
Wet gangrene can result from all of the cases listed above for dry gangrene, but always involves infection. In some cases, the initial cause of wet gangrene is considered to be an infection. Many species of organisms (mainly bacteria) are known to be involved in wet gangrenous infections; the classic bacterial organism associated with wet gangrene is Clostridium perfringens, an anaerobic bacterium that grows best in the absence of oxygen. These bacteria can cause myonecrosis (muscle death) with exotoxins and produce gas bubbles in dead and dying tissue (gas gangrene). This results in localized swelling with pressure and loss of blood flow to the tissue, allowing bacteria to spread infection to the connective tissue of muscles, skin, and other areas, causing necrotizing fasciitis (death of connective tissue).
Necrotizing fasciitis, in turn, allows the infection to spread, often at a rapid rate, from a locally infected area to other areas or into the bloodstream (sepsis). Although this cascade of events is observed with Clostridium perfringens often as one type of infecting organism, it can be caused by many other organisms, such as streptococcus, staphylococcus, bacteroides, and Escherichia coli. Typically, two or more of these organisms are found in an infection, and many researchers hypothesize that together the organisms help each other (synergy, cooperation) to spread the infection.
There are several subtypes of wet gangrene:
- Gas gangrene means that gas is present in the gangrenous tissue, as described above.
- Fournier's gangrene is a gangrene with necrotizing fasciitis that occurs primarily in the male genital organs.
- Internal gangrene is a general term that means gangrene affects an internal organ. Internal types of gangrene are usually named based on the organ that is affected (eg, gangrene of the appendix, gangrenous cholecystitis, and gangrenous bowel involving the colon, rectum, or other areas).
Difference between leprosy and gangrene
Leprosy (Hansen's disease, Leprosy) is not a variant of wet or dry gangrene, although it may result in localized tissue loss that may resemble gangrene. This is a disease caused by the mycobacteria Mycobacterium leprae and Mycobacterium lepromatosis, which is transmitted from person to person. Mycobacterium causes nodules and ulcers. M. leprae infection slowly destroys peripheral nerve endings in the limbs and mucous membranes over several years, resulting in decreased sense of touch. Fingers and other areas of the extremities suffer repeated trauma due to loss of sensation and may become disfigured. If these injuries become infected with other organisms, patients with leprosy may develop wet gangrene.
Forms of ischemia
What causes disruption of the blood supply to the intestines? Doctors distinguish two forms of ischemia: occlusive and non-occlusive.
Occlusive ischemia occurs due to blockage of the mesenteric veins and arteries. The following pathologies can provoke a violation of the blood supply:
- atrial fibrillation;
- heart defects;
- intestinal tumors;
- diseases of the gastrointestinal tract;
- cirrhosis of the liver.
Also, the occlusive form of the disease is observed in some patients who have undergone heart valve replacement.
Non-occlusive ischemia is observed in approximately half of the cases. Signs of pathology develop slowly. At present, the exact reasons for this violation have not been established. It is assumed that the following diseases and conditions can provoke non-occlusive ischemia:
- heart failure;
- chronic arterial hypotension;
- dehydration;
- taking medications that thicken the blood.
It is important to remember that any form of ischemia can lead to intestinal gangrene. Even if the blood supply disorder develops gradually, without treatment, sooner or later necrotic changes in the tissues occur.
What are the signs and symptoms of gangrene?
Symptoms of gangrene vary depending on the type of gangrene (wet or dry), anatomical location (external versus internal sites), and organ system involvement.
Symptoms of dry gangrene
Dry gangrene often begins with numbness and a feeling of coolness in the affected area. Levels of discomfort vary depending on the patient's perception. The affected area (such as the toes) then begins to discolor, usually turning from reddish to brown and eventually black. During this time, the affected area shrinks, becomes dry (mummified) and may peel off. Dry gangrene, caused by rapid loss of arterial blood supply, may initially appear pale or blue and then progress to more severe conditions as described above.
Symptoms of wet gangrene
Wet gangrene, unlike dry gangrene, usually begins with a swollen and very painful affected area, which may initially be red and show signs of decay (tissue peeling, suppuration, local oozing of fluid). Often the fluid and affected area develop a very bad odor, due to the presence of foul-smelling compounds such as cadaverine and putrescine. Dead and dying tissue develops a damp and black appearance. Additional symptoms that are often observed in patients with wet gangrene are fever and other signs of sepsis.
Internal gangrene, a variant of wet gangrene, has less obvious initial symptoms because wet gangrene occurs in the internal organs. The patient's condition may be severe due to sepsis. Sometimes the skin covering the organ with wet gangrene may become reddish or discolored, and the area may become swollen and painful. When the surgeon reveals the infected organ, signs of wet gangrene become obvious. Symptoms also vary depending on the organ system infected.
How is gangrene diagnosed?
A person may suspect gangrene if an area of the body changes color (especially if the skin is red, blue, or black) and becomes numb or painful. If symptoms include those listed above for dry or wet gangrene, the person should seek medical attention immediately.
Diagnosis is usually based on clinical symptoms of wet or dry gangrene. Often other tests are performed in cases of wet gangrene to further determine the infecting agent(s), type of gangrene, and extent of infection. For example, X-rays or CT scans are performed to see how gas or necrosis (or both) is progressing from the local area. These tests are often performed to help determine the extent of gangrene in both the extremities and internal types of gangrene. Blood cultures, as well as cultures of infected tissue and exudates, are routinely performed to identify the infectious agent(s) and to determine appropriate antibiotic therapy.
For dry gangrene, vascular surgeons often perform angiography (a radiological test with a dye that shows arterial blood flow in tissue, also called an arteriogram) to see the extent of current or potential loss of arterial blood in tissue.
What is the treatment for gangrene?
Treatment for gangrene depends on the type of gangrene (dry or wet), the subtype of wet gangrene, and how much tissue is affected by the gangrene. Immediate treatment is necessary in all cases of wet gangrene and in some cases of dry gangrene. Treatment for all cases of gangrene usually includes surgery, medication, support, and sometimes rehabilitation.
Treatment of dry gangrene
Dry gangrene is usually treated with surgery to remove the dead tissue(s). How much tissue is removed may depend on how much arterial blood flow is still reaching other tissue(s). Patients are often treated with antibiotics to prevent infection of the remaining viable tissue. The patient may also take anticoagulants to reduce blood clotting. Supportive care may consist of surgical treatment of wounds and rehabilitation to restore the finger or limb. Some patients simply destroy the dry gangrenous tissue and this is called autoamputation. This occurs most often when medical and surgical care providers are not always available to the patient in remote areas or in some third world countries. Many patients, if they do not become infected, can recover from autoamputation.
Treatment of wet gangrene
Wet gangrene is a medical emergency and needs immediate treatment. Treatment is usually done in a hospital and a surgeon must be involved because the local area needs surgery (surgical removal of dead and dying tissue). In some patients, drug treatment will not work and a limb may need to be amputated. At the same time as surgery, intravenous antibiotics (usually a combination of two or more antibiotics, one effective at killing anaerobic bacteria such as Clostridium perfringens and another antibiotic effective against methicillin-resistant Staphylococcus aureus, or MRSA) must be administered. Consultation with an infectious disease specialist and surgeon is recommended.
Internal gangrene requires surgery in a hospital to remove the gangrenous tissue. Some patients develop sepsis and require the support of an intensive care unit, which can provide supportive care and control for other life-threatening problems such as hypotension (low blood pressure). Rehabilitation therapy for amputation patients is highly recommended.
Some clinicians treat gangrene, especially wet gangrene, with hyperbaric oxygen (oxygen under pressure with the patient inside a chamber). Because some studies show that hyperbaric oxygen treatment improves oxygen supply to tissues and can inhibit or kill anaerobic bacteria, this therapy is used to treat patients with gangrene. However, it is not available in many hospitals and is used in combination with the therapeutic modalities described above rather than as a primary therapy for wet gangrene.
How to prevent gangrene?
If the tissue receives good oxygenation (oxygen) from normal arterial blood flow and is not infected by microbes, then both dry and wet gangrene can be prevented. Therefore, by avoiding tobacco use and avoiding external injuries such as frostbite, gangrene can be prevented. Perhaps the best way to prevent gangrene, especially in developed countries, is to keep diabetic patients under good glucose control and regularly examine their feet for any signs of cutting, infection or redness. Patients with diabetic neuropathy (eg, numbness in the extremities) should do this daily.
If any wound or burn occurs, it should be treated immediately to prevent infection. This is especially important in people with diabetes, vasculitis, or a compromised immune system.
Some patients who notice coolness and redness in a specific area (such as the toes) should undergo an angiogram, which will show whether there is an arterial blockage and, if detected early, dry gangrene (and possibly wet gangrene) can be successfully prevented. However, this must happen quickly so the vascular surgeon can remove the clot or obstruction in the artery.
Reasons for the development of the disease
You may be interested in: The drug "Acecardol": instructions for use, indications, analogues and reviews
The location of the pathological process is determined by the anatomical features of the structure of the human body. The skin of the external genitalia and perineum and subcutaneous fatty tissue are quite loose. There are many sebaceous and sweat glands and hair follicles, a dense network of veins and a small number of arteries concentrated here. During the inflammatory process in this area, blood flow slows down and tissue circulation is disrupted. Ischemia begins to spread to the connective tissue membrane, provoking the development of gangrene of the skin. Then necrosis of the scrotal membranes occurs, swelling and microabscesses develop.
Thus, Fournier’s gangrene has the following causes of development:
- Superficial injury to the genital organs.
- Diseases of the urogenital tract and the genitourinary system as a whole.
- Use of steroid enemas.
- Carrying out injections into the external genitalia.
- Presence of a foreign body in the rectum.
- Genital piercing.
Provoking factors that create a high risk of developing pathology include:
- Alcoholism and drug addiction.
- Liver cirrhosis and HIV infection.
- Circulatory disorder.
- Diabetes and obesity.
- Treatment of oncology with chemotherapy.
- Cancerous neoplasms.
- Long-term use of glucocorticosteroids.
- Crohn's syndrome.
What is the prognosis (prognosis) for a patient with gangrene?
Patients with dry gangrene usually feel well until they become infected. These patients lose some local function due to tissue loss and, if they have an ongoing disease such as diabetes, may develop dry gangrene again. In general, patients recover with minimal complications if tissue loss is small.
Patients with wet gangrene generally have a poorer prognosis than patients with dry gangrene. Statistics for the United States indicate low mortality in patients hospitalized with gangrene. Mortality increases if the patient becomes septic. If treatment is started early, some patients require amputation (finger, limb). Although mortality remains unchanged, cases of gangrene have been increasing in developed countries in recent years, possibly due to an increase in the number of patients with diabetes and other diseases that affect the vascular system, but these data are not complete.
Diagnostics
In terms of frequency of cases, gangrene of the lower extremities ranks first.
In this case, gangrenous lesions also occur:
- Intestinal sections.
- Gallbladder.
- Other abdominal organs.
- Fingers and hands.
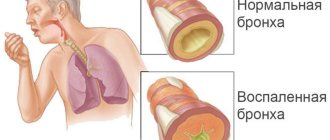
- Light.
To diagnose this pathology, modern medicine uses the following types of examinations:
- Blood chemistry.
- General clinical blood test.
- Blood test for sterility.
- Analysis of released exudate.
- In the biochemistry of blood in the disease obliterating atherosclerosis with gangrene, an increased level of cholesterol is observed. With diabetes, there will be an increased level of glucose in the blood.
- A general blood test will show leukocytosis with a characteristic increase in the number of band neutrophils of more than 5 percent.
- Blood is tested for sterility in the event of sepsis. The analysis identifies the pathogen, determines its type and susceptibility to antibiotics.
- Purulent exudate released from the wound is examined by bacteriological and bacterioscopic methods. This makes it possible to determine the nature of the rotting agent and its reaction to the action of medications.
Gangrene of the lung on an x-ray is shown in the following photo:
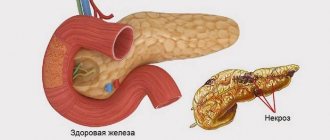
This is what gangrene of the small intestine looks like: