What is necrosis
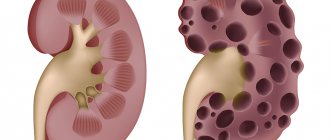
Pancreatic necrosis is a pathological phenomenon that is characterized by changes and death of its tissues. It occurs as a result of the development of acute pancreatitis. The function of the pancreas is to produce digestive enzymes that enter the duodenum and allow the body to break down fats, proteins and carbohydrates, generally aiding digestion. If the ducts of the gland are damaged or obstructed, enzymes begin to act on the pancreas itself, dissolving and digesting it.
Why does hemorrhagic pancreatic necrosis occur?
The following factors contribute to the development of pancreatic necrosis:
- inflammation of the pancreas with disruption of its functions and cessation of the outflow of pancreatic juice;
- intoxication of the body due to systematic consumption of alcoholic beverages;
- frequent reflux of pancreatic juice into the pancreatic ducts, which occurs with cholelithiasis;
- infectious diseases of the gallbladder and bile ducts;
- thrombohemorrhagic syndrome, accompanied by blood clotting inside the vessels;
- acute bacterial and viral infections;
- long-term use of cytostatics;
- radiation exposure;
- autoimmune pathologies (hemorrhagic vasculitis);
- coronary heart disease, causing circulatory disorders in all organs and tissues;
- pancreatic injuries, including complications of surgical interventions.
Regardless of the cause of pancreatic necrosis, the mechanism of its development is based on:
- on damage to the acinus secretory center responsible for the production of pancreatic enzymes;
- on increasing the level of enzyme content to critical values. In this case, the substances begin to destroy pancreatic tissue - hydrolyze proteins;
- on damage to the walls of blood vessels. The accumulation of the enzyme elastase in tissues leads to hemorrhages. Gastroenterologists call this phenomenon pancreatic autoaggression;
- on the aggressive effects of trypsin and pancreaticopeptidase - proteolytic enzymes necessary for the breakdown of protein foods;
- on a failure in the humoral process of controlling the synthesis of digestive enzymes.
Classification of pancreatic necrosis
Necrosis of the gland can be focal or extensive, characterized as progressive or sluggish. Depending on how pancreatic disease progresses, it is considered hemostatic, edematous, destructive or functional. Hemorrhagic pancreatic necrosis is possible. Acute edematous necrosis of the gland can be treated conservatively if measures are taken in a timely manner.
With necrosis, swelling of the parenchyma occurs, pressure on pancreatic cells increases and movement along the ducts is disrupted. If the disease is not stopped, then food enzymes will destroy the gland and the decomposition process will begin. This can lead to pus from the pancreas entering the abdominal cavity, resulting in acute peritonitis and purulent sepsis. This situation threatens the patient’s life and requires immediate surgical intervention.
Pancreatic necrosis is secondary to acute pancreatitis. Depending on where pancreatic necrosis occurs, it is called local, when only one anatomical area is affected, diffuse, if there are two or more such areas. It varies according to the depth of the lesion. Pancreatic necrosis can be superficial, deep, or total. Based on how the disease passes and develops, it is recognized as recurrent, progressive, regressive, fulminant or abortive.
Mild disease is diffuse or edematous necrosis of the gland with small foci. At an average stage, diffuse or local pancreatic necrosis is characterized by larger foci. In severe cases, pancreatic necrosis is diffuse or total in nature and has large foci. There is also an extremely severe stage, in which pancreatic necrosis is accompanied by various complications that lead to irreversible consequences and, as a result, death. There is also a difference in the origin of pancreatic necrosis.
Causes
Pancreatic necrosis occurs as a result of pancreatitis if it has not been treated for a long time, or the patient has engaged in ineffective self-medication without the supervision of a specialist.
Pancreatitis is formed as a result of:
- constant alcohol abuse;
- unhealthy diet, in which high-fat foods predominate;
- diseases of the bile-forming and excretory organs;
- pathologies of any abdominal organs.
The most popular reason why people end up in surgery is the simultaneous abuse of large doses of alcohol and overeating fatty foods. As a rule, after festive gatherings with a full meal, the departments of surgery and gastroenterology are overcrowded with patients.
Necrosis of the head of the pancreas means an urgent call for an ambulance or delivery of the patient to the surgical department. Unfortunately, most victims are immediately diagnosed with pancreatic necrosis, since before entering the hospital there were preconditions for pancreatitis.
It is also worth noting the rarer causes of this diagnosis:
- diseases of the digestive system of an infectious or parasitic nature;
- dysfunction of the sphincter of Oddi (a group of small muscles in the gastrointestinal tract that controls the movement of digestive fluids between different organs);
- abdominal organ injuries;
- endoscopic procedures;
- congenital pancreatic pathologies;
- after surgery on internal organs.
If any of the above cases exist, the person should be regularly monitored by a gastroenterologist to prevent complications.
Symptoms of the disease
The main symptom of pancreatic necrosis is, first of all, severe pain under the ribs on the left side. It often encircles, passes around the entire body, extending to the shoulder blade and shoulder, resulting in a false feeling that it is a heart attack. Signs of pancreatic disease are bluish spots on the sides of the abdominal cavity, upset stool, nausea. The abdominal anterior wall becomes tense, its palpation causes pain.
Fluid accumulations may be observed in the pericardium and pleural cavity. At the same time, the temperature becomes higher, redness may appear on the skin in the pancreatic area, or, conversely, it will become paler. All this, as a rule, is accompanied by increased gas formation, bloating, and nausea. The chronic form of pancreatic necrosis has complications such as diarrhea, diabetes mellitus, jaundice, liver dystrophy, intestinal and gastric bleeding.
Main features
- Pain. The strength of the pain syndrome depends on the severity and course of the disease, and therefore is not always pronounced. Unbearable and debilitating pain occurs in almost 90% of patients, some of them are accompanied by sudden cardiovascular failure (collapse), sometimes fatal. The rest of the patients report moderate pain.
- Gagging or vomiting that is not related to food intake and does not improve the patient’s well-being. Due to the destruction of blood vessels, the vomit contains blood in the form of clots mixed with bile. Debilitating vomiting contributes to dehydration of the body, a decrease in diuresis occurs, which entails a lack of urination and severe thirst.
- Flatulence. Fermentation processes in the intestines contribute to increased gas formation. This leads to gas retention and causes severe bloating, causing constipation due to weakening peristalsis.
- Intoxication. During the period of progressive development of necrosis, bacterial toxins lead to intoxication of the body. All of the above symptoms are accompanied by severe weakness and decreased blood pressure. The patient experiences shortness of breath and increased heart rate. Under the influence of a large number of toxins, encephalopathy may occur, which, in addition to disorientation of the patient, can lead to the development of coma.
- Pale skin (hyperemia). At an advanced stage of the disease, after severe intoxication of the body, the patient’s skin becomes yellow with an earthy tint. As a result of internal hemorrhages, blue spots appear on both sides of the abdomen and back, and sometimes in the navel area.
- Purulent complications are a fairly advanced stage of necrosis. Due to inflammation and intoxication, the pancreas greatly increases in volume, this leads to the formation of a purulent infiltrate, the development of toxic hepatitis and a disappointing prognosis.
Complications of necrosis:
- Enzyme deficiency;
- Stomach ulcer and abscess;
- Stomach bleeding;
- Peritonitis and fistulas;
- Thrombosis of mesenteric veins.
Diagnosis of the pancreas
If the presence of discomfort in the abdominal cavity and the pancreas begin to bother you, if there is a suspicion that this is necrosis of the gland, then you should consult a therapist. After examining the patient and finding out all the circumstances, he performs palpation and finds out the presence, nature and location of painful manifestations. If a pathology of the gland is detected, the patient is referred to an endocrinologist. In case of pancreatic necrosis, the therapist writes a prescription for anti-inflammatory medications and recommends nutritional therapy and enzymes.
After undergoing treatment and new tests, the doctor makes a decision on further combating pancreatic necrosis or states that the disease has receded. The endocrinologist intervenes when the patient notices disturbances in the production of insulin and prescribes a precisely adjusted dose of the artificial analogue. An oncologist can also get involved in treatment if neoplasms or tumors are found on the gland.
Ultrasound, MRI and CT make it possible to understand the condition of the pancreas, to see whether there is an abscess, swelling, whether there are signs of inflammation, whether there are deformities, changes in size or neoplasms. Ultrasound will help to understand the echogenicity of the parenchyma and the presence of exudate, determine the presence of stones and cysts on the gland, and understand the condition of the ducts. Computed tomography and magnetic resonance imaging are similar to ultrasound in that they can demonstrate the condition of the pancreas, but do so with greater accuracy.
Laboratory studies provide information about the processes occurring in the gland, the state of digestive enzymes and hormones. An increase in amylase levels in the blood and urine will confirm the presence of pancreatic necrosis. The level of glucose in the blood will indicate abnormalities in the functioning of the endocrine system. Only having the data of all examinations that will help check the condition of the gland, a specialist will make a final diagnosis.
Life forecast
Hemorrhagic pancreatic necrosis has an extremely unfavorable prognosis. Even with timely initiation of treatment, the death of the patient is observed in half of the cases. If you refuse therapy, this figure approaches 100%.
Causes of death
The main causes of sudden, sudden death in pancreatic necrosis:
- septic complications that impair the functions of all organs;
- infectious-toxic shock, due to which infection is considered a negative factor in the course of the pathology;
- irreversible change in the structure of the pancreas;
- total tissue necrosis;
- reactive changes in affected tissues.
In the situations described above, death occurs instantly or after a few days. It is extremely rare for a patient to survive more than 2 weeks.
Treatment methods
In most cases, pancreatic necrosis is noticed at an early stage, then a special diet is prescribed along with a course of medications. For some time, a patient with a diseased pancreas may be put on a therapeutic fast to remove toxins. Antispasmodics, anti-enzyme drugs, immunostimulating and antibacterial agents are often prescribed. In the early stages of pancreatic necrosis, it is possible to avoid surgery, which is dangerous because it is difficult to know which areas are affected.
Medicines
To treat the pancreas, diuretics are used, and a local novocaine blockade is performed. To combat gland necrosis, antihistamines are used, and antispasmodics are administered intravenously in the presence of severe pain. A patient with a diseased pancreas receives insulin; if his blood glucose level increases, protease inhibitors are used. Patients take choleretic drugs if there are no gallstones.
Mineral waters containing alkali, cooling the pancreas, and fasting may be appropriate. If the disease was noticed in time, diagnosed and treated in a timely manner, then recovery and relief from the symptoms of necrosis is possible in 1-2 weeks. When the gland cannot be cured therapeutically, the patient is referred to a surgeon.
Find out how the pancreas is treated with medications.
Folk remedies
During an exacerbation of necrosis, the patient experiences severe pain. However, not only traditional medicine can cope with this. If you don’t want to stuff yourself with chemicals, try treating your pancreas with folk remedies. For this, plants and berries are used that can fight inflammation and reduce pain during necrosis. Let's find out how to treat your pancreas using natural remedies.
A decoction of Japanese Sophora will be useful. Pour a glass of boiling water over a spoonful of herbs and leave for several hours. The decoction should be drunk warm and consumed before meals. The course of Sophora to combat gland necrosis should not last more than ten days. It should take several weeks before using it again. The action of Sophora is primarily aimed at alleviating pain from pancreatic necrosis.
Blueberries are useful as an anti-inflammatory agent for necrosis. Leaves or berries are brewed, no matter dried or fresh. Use the drink as a daily drink to treat your pancreas. Immortelle has a similar effect. A spoonful of dry immortelle should be poured with a glass of boiling water. The resulting decoction, which must be divided into three times, should be enough for a day. This is a good remedy for the treatment of gland necrosis. Treatment of pancreas with folk remedies involves the use of oat decoction. It also relieves irritation and promotes the removal of toxins.
How does pancreatic necrosis develop?
In patients with pancreatic necrosis, the development of pathology can occur gradually or rapidly, but always in 3 stages:
- At the initial stage, toxic substances of bacterial origin appear in the blood.
- An abscess occurs in the tissues of the pancreas and nearby organs.
- Purulent pathological changes begin in the tissues of the pancreas and neighboring organs.
According to the prevalence, the disease can be divided into focal and extensive necrosis. The first implies that the disease occurs only in the pancreas, and in the second case, necrosis can spread to other organs.
Nutrition for necrosis
Pancreatic necrosis of the pancreas imposes certain restrictions on the patient's diet. It may contain vegetarian soups with cereals such as oatmeal, buckwheat, rice or semolina. Soups may contain vermicelli; the following vegetables will not be out of place: carrots, potatoes, zucchini, pumpkin. Add lean meat, chicken or beef to the menu. These types of meat are a good solution for patients with pancreatic necrosis.
If you have a diseased pancreas, pureed porridges cooked in water are allowed, to which it is acceptable to add a little milk. Egg white omelettes, boiled pasta, calcined cottage cheese, milk, fermented milk drinks, sweet berries and fruits are not prohibited. Patients with gland necrosis are recommended to receive at least 10 grams of refined vegetable oils per day.
For patients with gland necrosis, coffee and cocoa, broth-based soups, alcohol, smoked meat and sausages, canned food, fatty fish, soda, mushrooms, fresh bread, jam, egg yolk, ice cream, barley, millet, pearl barley will be prohibited for consumption forever. cereals, baked goods. It will not be possible to include pancreas, grapes, figs, sweet peppers, bananas, garlic, and onions in the diet of a sick person.
Special diet
The therapeutic diet for pancreatic necrosis is the basis of treatment and is prescribed at the very beginning of the disease and in the postoperative period. For complete recovery, the duration of the diet should be at least six months. The diet for the treatment of pancreatic necrosis should ensure frequent intake of food into the body in small portions.
In the first days from the onset of the disease and immediately after the operation, doctors prescribe a zero table, that is, the patient cannot eat or drink anything. The patient receives all the necessary nutrients and vitamins through the blood. Such nutrition is called parenteral; usually, such a diet includes medications injected into the blood (20% glucose, amino acid solution, insulin and fatty emulsions). It is very important that the patient does not smell food during the fasting period, since even this can provoke the body to produce enzymes.
If you have necrosis of the pancreas, you should not eat fried, fatty, spicy, salty, smoked and pickled foods.
It is recommended to stop smoking and drinking alcohol.
Fresh bread and other fresh flour products are prohibited. It is recommended to consume only dried bakery products. The diet excludes baked goods; from baked goods you can eat unsweetened biscuits.
In case of necrotizing pancreatitis, at first it is recommended to eat only first courses, vegetables must be chopped, there should be no pieces. Soups can be prepared with rice, noodles, oatmeal and buckwheat; for fat content, no more than 1 tsp can be added to the finished dish. sour cream or a small piece of butter per serving, but not earlier than 1-2 weeks after leaving the hospital.
Important information: Causes of enlarged pancreas
Meat and fish can be consumed with necrotizing pancreatitis, but preference should be given to lean, low-fat varieties (veal, rabbit, beef, chicken and turkey, pike). Meat and fish broths can be eaten no earlier than 4 weeks after discharge from the hospital. You can only eat white omelettes without adding yolks.
Some of the most necessary consumer products for pancreatitis are milk, fresh low-fat cottage cheese and other fermented milk products. Fruits can only be consumed when they are very ripe and soft, or in the form of mousses and jellies. For drinks, it is advisable to drink weak tea and dried fruit compotes.
The diet for pancreatic necrosis and after recovery is designed for six months. Often patients become so accustomed to this diet that they continue to eat properly for the rest of their lives.