Most acute inflammatory processes are accompanied by pyretic temperature.
In this condition, which is also called pyretic fever, the mercury column of the thermometer is in the range of 39.1-40.9 degrees. The ailments in which pyretic fever develops are provoked by viruses and pathogenic bacteria. They enter the human body during contact with carriers of infection or as a result of violation of the integrity of the skin during injuries or operations. Often, pathogenic microbes are already present in the body, but are activated after hypothermia.
What is pyretic temperature
Normal human body temperature ranges from 35-37 degrees. An increase in the reading in the range of 37.1-37.9 is called low-grade fever. Moderate fever (febrile) is characterized by a rise from 38 to 39 degrees. At a pyretic temperature, the thermometer reaches values of 39.1-40.9 degrees. We are talking about a hyperpyretic increase if the thermometer shows above 41 degrees.
Pyretic fever is a condition that requires the use of antipyretic drugs. But the best way to get rid of the symptoms associated with high fever is to treat the disease that caused hyperthermia, i.e. overheating
Intense heat can cause deterioration in the condition of people suffering from chronic pathologies of the cardiovascular, nervous systems, kidneys and liver. In children, prolonged fever can provoke convulsions, and in the youngest – loss of consciousness and dehydration. Therefore, it is important to seek medical advice as soon as possible if the thermometer shows high levels. The specialist will not only prescribe adequate treatment for the underlying disease, but will also select a drug and calculate its dosage, focusing on the patient’s weight and age.
Etiology and pathogenesis
Acute and chronic rheumatic fever is caused by the activity of beta-hemolytic streptococci belonging to group A. The etiology of the disease identifies the following negative factors that influence the development of the pathology:
- Streptococcal infectious disease of acute or chronic course.
- Tonsillitis.
- Unfavorable living and working conditions.
- Seasonal weather changes.
- Age characteristics. In children aged 7-15 years, boys and women, rheumatic disease is observed more often than in other people.
- Genetic predisposition.
The pathogenesis of acute rheumatic fever is quite complex and goes through several stages:
- mucoid swelling;
- fibrinoid changes;
- granulomatosis;
- sclerosis.
The formation of granulomas occurs in the third stage of the disease.
At the initial stage, the connective tissue swells, increases in size, and collagen fibers split. Without treatment, the disease leads to fibrioid changes, resulting in necrosis of fibers and cell elements. At the third stage, rheumatoid arthritis provokes the appearance of rheumatic granulomas. The last stage is sclerosis with a granulomatous inflammatory reaction.
Causes of pyretic temperature
There are many pathological conditions that provoke fever above 39 degrees. In more than 80% of cases, the causes of pyretic body temperature are infectious processes and are caused by the following diseases:
- influenza, acute respiratory viral infections;
- meningitis;
- mononucleosis;
- gastroenteritis.
Infectious processes in the organs of the respiratory system can provoke a temperature jump. These diseases include pneumonia, tuberculosis, and pharyngitis.
There are other infectious diseases that cause fever above 39 degrees:
- especially dangerous - plague, cholera, anthrax, yellow fever, dengue fever, malaria;
- intestinal – dysentery, salmonellosis;
- genitourinary – genital herpes, chlamydia, gonorrhea, candidiasis, acute stage of pyelo- or glomerulonephritis;
- children's drips - measles, chicken pox, mumps, scarlet fever.
Hyperthermia with pyretic values can develop after transfusion of blood and its components, or transplantation of a donor organ. In this case, the cause of the temperature jump is inflammation and subsequent rejection of foreign tissue.
A fever that does not go away for more than 5 days is caused by the use of large doses of cocaine.
The same undesirable effect sometimes occurs with neuroleptic malignant syndrome, or after the use of gaseous anesthetics - halothane, isoflurane.
How is diagnosis carried out?
To make a diagnosis, the patient must take an oral smear.
Sometimes it is difficult for doctors to identify acute rheumatic fever, since the pathological signs are similar to those of other diseases. The examinations take into account different diagnostic criteria. To confirm the diagnosis, a comprehensive diagnosis is required, including such instrumental and laboratory tests as:
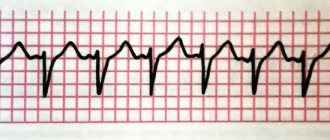
- echocardiogram using Doppler mode;
- an electrocardiogram that determines whether there are pathologies in the contraction of the heart muscles;
- general blood test;
- test for antibodies against streptococcus;
- bacteriological swab from the oral cavity to determine the hemolytic streptococcal agent.
Equally important is differential diagnosis, which allows one to distinguish the manifestations of acute rheumatic fever from the symptoms that occur with arthritis and other joint disorders. The doctor must differentiate deviations from such pathologies:
- mitral valve prolapse;
- endocarditis;
- viral inflammation of heart tissue;
- benign tumor in the atrium.
Signs of pyretic fever
Pyretic body temperature is difficult to tolerate for both adults and children. The malaise is accompanied by severe intoxication, decreased performance, and lack of appetite. Increased sensitivity to bright light often occurs. Most patients with high fever note that there are unpleasant sensations in the joints, twisting of the limbs and bones, pain in the muscles and skin.
During a fever, breathing and heart rate increase. Attacks of nausea and vomiting may occur. Children may develop seizures and short-term loss of consciousness.
Prevention of acute rheumatic fever
Prevention of the development of ARF consists of timely and correct treatment of various streptococcal infections ( sore throat , pharyngitis , skin infections ) by prescribing antibiotics. Treatment usually lasts at least one and a half weeks. Biseptol and ofloxacin to treat tonsillitis caused by streptococcal infection .
Prevention of acute rheumatic fever after infectious diseases includes a number of therapeutic measures. First of all, long-acting antibiotics, bicillin prophylaxis ( extensillin and retarpen ), are prescribed for a period of approximately 5 years. Treatment has continued for more than 5 years for those who have suffered rheumatic carditis.
It is necessary to follow the correct daily routine, eat regularly, exercise, stop smoking and drinking alcohol, strengthen the body, and walk in the fresh air. Do not forget that there are a lot of pathogenic organisms, and especially streptococci, in the environment; they are found in dust and dirty things, so it is necessary to frequently carry out wet cleaning and ventilate the room. carious teeth , tonsillitis , sinusitis and sinusitis untreated .
Features of pyretic fever in children
High body temperature during pyretic fever in a child requires special attention. In children, hyperthermia can cause serious disturbances in the functioning of the body. Much more often than adults, children suffer from dehydration, problems with the heart and blood vessels, and seizures.
The high need of the child's body for energy provokes a more active breakdown of glucose. If the baby has no appetite, the reserves of this carbohydrate are quickly depleted, and its synthesis from fat begins. As a result, acetone syndrome develops. It is accompanied by vomiting, diarrhea, and the appearance of a specific odor from the mouth.
What are the dangerous consequences?
The most severe complication of acute rheumatic fever is heart failure and cerebral ischemia. And other violations are also likely if treatment is not timely:
A serious complication of the pathology can be a kidney infarction.
- insufficient blood flow;
- atrial fibrillation;
- myocardiosclerosis;
- endocarditis;
- renal infarction;
- dysfunction of the spleen;
- adhesions in the area of the pleural or pericardial cavity;
- thromboembolism of the great vessels.
How to reduce pyretic temperature
The World Health Organization recommends reducing high temperatures in preschool children and primary schoolchildren already at 38.5 degrees. It is recommended for adults to reduce fever starting at 39 degrees. The condition, accompanied by pyretic numbers on the thermometer, is especially dangerous for children and adults with pathologies of internal organs.
Fever, in which the thermometer rises above 39, requires the use of antipyretic medications. The most effective drugs are those based on ibuprofen and paracetamol. The dosage of the drug, its form (tablets, suspension or rectal suppositories) should be determined by the doctor, focusing on the weight, age, and condition of the patient.
A decrease in temperature after taking antipyretics usually occurs after 30 minutes. If there is no effect from the medication, you must immediately call an ambulance.
As an auxiliary measure, immediately after taking an antipyretic, you can wipe the body with a cloth moistened with water at room temperature. It is necessary to ensure that there is an influx of fresh air into the room where the patient is located.
While waiting for the antipyretic medicine to work, you need to open the fever. This will help the body get rid of excess heat. Additionally, it is allowed to apply a cool compress to the liver area, in the groin folds, under the knees, and on the elbows.
A prerequisite for successfully reducing fever is drinking plenty of fluids. Doctors recommend drinking compotes from dried fruits or berries (for children they can be sweetened), and still mineral water.
Herbal teas have an antipyretic effect. You can offer the patient a healing drink from:
- linden color;
- chamomile;
- peppermint;
- blackberry leaves;
- wild strawberry leaves;
- sprigs of raspberry or willow.
Raspberry jam will be beneficial for fever. Freshly squeezed juice of half a grapefruit and two oranges will also help you get rid of hyperthermia faster. This mixture is diluted with a small amount of boiled water.
Classification
Acute rheumatic fever is divided into different forms and types, which depend on many indicators. When dividing a disease into types, the criteria of pathogen activity, severity of the disease and other parameters are taken into account. The table shows the main types of violation:
| Classification | View | Peculiarities |
| By phase | Active | Occurs with minimal, moderate or high activity |
| Inactive | There are no clinical or laboratory manifestations | |
| With the flow | Spicy | Sudden onset of acute rheumatic fever with severe symptoms |
| High degree of pathological process activity | ||
| Subacute | The attack lasts from 3 to 6 months | |
| The clinical picture is less pronounced than in the acute course | ||
| Protracted | It lasts a long time and can last more than 6 months | |
| Dynamics and activity are weak | ||
| Latent | Clinical, laboratory and instrumental manifestations are not detected | |
| Recurrent | Undulating course with severe exacerbations and short stages of remission | |
| According to clinical and anatomical manifestations | Involving the heart | Myocardiosclerosis and rheumatic carditis progresses |
| With damage to other internal organs | The function of blood vessels, lungs, kidneys, subcutaneous structures is impaired |
When a repeated fever occurs, the internal organs are significantly damaged and irreversible processes occur.
Consequences and complications
Pyretic temperature is a dangerous condition in which it is necessary to urgently consult a doctor.
Hyperthermia leads to disruption of body functions not only in children, but also in adults. The consequence of overheating of the body is disruption of the nervous system, cardiac dysfunction, vascular reactions, and breathing problems. The most common complications of hyperthermia are convulsions, fainting, and dehydration. It is also possible to develop heart failure.
In other articles on our website you can read more about febrile and hyperpyretic human body temperatures.
Author of the article : Elena Lobashova, physician and psychologist. In 1997 she graduated from Cherkasy Medical School with a degree in nursing. She worked for 5 years at the regional cardiological clinic. In 2005 she graduated from the Rivne Institute of Slavic Studies of the Kyiv Slavic University. From 2002 to 2010 she worked as an instructor in sanitary education at the Rivne Regional Health Center. Since 2010 - head of the organizational and methodological department, medical psychologist. Regular author of the website temperaturka.com.
Symptoms of acute rheumatic fever
The first symptoms of ARF appear 2-2.5 weeks after the illness, usually after tonsillitis or pyoderma . A person’s general health deteriorates, body temperature can rise to 38-40 degrees, joints hurt and swell, and the skin turns red. Palpation is painful, as is movement of the joints. Usually the large joints of the body (knees and elbows) are affected, and rarely the joints of the hands and feet. Inflammation of the joints is usually observed simultaneously in both limbs.
The pain is migrating, that is, it can move from one joint to another. These are manifestations of arthritis , which lasts no more than 10 days. After some time, the signs of arthritis disappear, more often in children, and in adults, sometimes arthritis can develop into Jaccoud's syndrome , characterized by deformation of the bones of the hands without dysfunction of the joints. As a result of repeated attacks, arthritis affects more joints, becoming chronic.
rheumatic carditis also develops . Sometimes there are no symptoms, but more often there is arrhythmia, shortness of breath , aching pain in the heart and swelling. Even with mild rheumatic carditis, the heart valves are affected, they shrink and lose their elasticity. This leads to the fact that they either do not open completely or do not close tightly, and valve disease .
Typically, rheumatic carditis is observed at a young age from 15 to 25 years, and almost 25% of patients suffer from rheumatic heart disease as a result, especially in the absence of adequate treatment. By the way, ARF accounts for approximately 80% of acquired heart defects.
Many have a monosymptomatic course of ARF, with a predominance of symptoms of arthritis or rheumatic carditis .
On the skin, symptoms of acute rheumatic fever appear as ring-shaped rashes ( erythema ) and subcutaneous rheumatic nodules. These nodules are usually grain-sized and located in the periarticular tissues . They are absolutely painless, the skin is not changed. Rheumatic nodules often form over bony prominences in the joint area. They are found exclusively in children. Ring-shaped erythema is a disease, the characteristic symptom of which is the appearance on the body of pink spots with a diameter of about 5 centimeters. They spontaneously appear and disappear, and are localized on the chest, back and inner surface of the limbs.
Rheumatic damage to the nervous system caused by ARF is most often observed in children at a young age, as a result of which the child becomes capricious, he quickly gets tired, his handwriting and gait change. Minor chorea is often observed in girls 1.5-2 months after streptococcal infection. Chorea is involuntary twitching of the limbs and muscles that disappears during sleep.
In adolescents who have had a sore throat, acute rheumatic fever often begins gradually, the temperature rises to low-grade , pain in large joints and moderate signs of carditis . Relapses of ARF are associated with previous streptococcal infections, and usually manifest as rheumatic carditis.
The cause of acute rheumatic fever is beta-hemolytic streptococcus , which affects a weakened body. It is after a person has had a sore throat , scarlet fever or tonsillitis caused by streptococci that he begins to develop ARF. Please note that acute rheumatic fever is a disease of a non-infectious nature, because Streptococci do not affect joints. Simply, as a result of infection, the normal functioning of the immune system is disrupted. Research shows that some streptococcal proteins have many similarities with joint proteins, as a result of which the immune system, “responding” to the streptococcal challenge, begins to attack its own tissues, and inflammation develops.
There is a high chance of getting acute rheumatic fever in those whose relatives suffer from rheumatism. Children from 7 to 16 years old are susceptible to the disease; adults get sick much less often. In addition, the chance of infection with streptococcus increases in poor living conditions, insufficient nutrition and regular malnutrition.
Stages of the inflammatory process
Pathological processes in tissues with ARF occur in the form of:
- mucoid swellings (at this stage, there is disintegration and swelling of connective tissue and hyaluronic fibers);
- fibrinoid swellings (irreversible disorganization of connective tissue and hyaluronic fibers occurs, as well as the appearance of exudative (accompanied by accumulation of fluid) inflammation and foci of fibrinoid necrosis);
- proliferative inflammation (formation of specific Aschoff-Talalaev granulomas around necrotic foci in cardiac tissue);
- sclerotic lesions (formation of scars at the site of necrotic lesions).
As a result of sclerotic inflammation, deformation and fusion of valve structures occurs and the formation of acquired valve defects and signs of HF (heart failure).
Negative effects of fever
When compensatory mechanisms are depleted or a hyperergic version of fever develops, this becomes the cause of pathological conditions.
The younger the child, the more dangerous a rapid increase in temperature is for him due to the progression of metabolic disorders, cerebral edema and the occurrence of seizures.
- The depth and minute volume of respiration (MV) decreases, and the frequency of respiratory movements increases by 2–3 times, which leads to hypoxia.
- An increase in body temperature by 1°C increases the heart rate (HR) by 10 beats per minute, which worsens the functioning of the heart, since with an increase in metabolic rate, the myocardial need for oxygen increases.
- There is a change in consciousness of varying degrees of severity: from minor to delirium with hallucinations and delusions.
- The activity of the gastrointestinal tract is disrupted, which is manifested by a decrease in the secretory activity of digestive juices, motility and intestinal absorption. Clinically, there is a lack of appetite, dry mouth, constipation, and increased gas formation.
- Metabolic processes are upset: every degree above normal values increases the basal metabolism by 10%. Due to intoxication, proteins decompose, acidosis, hypoglycemia, loss of chlorides, potassium and sodium ions appear.
- Due to increased sweating and rapid breathing, the body loses fluid, causing dehydration.
- A clinical symptom of impaired blood microcirculation is the appearance of a marbled pattern on the skin and cold extremities.
- As a result of imperfect mechanisms of thermoregulation and immaturity of the central nervous system in children under 5 years of age, especially against the background of perinatal encephalopathy, epilepsy, cerebral palsy, the risk of developing febrile seizures increases.
Diagnosis of Q fever
Diagnosing Q fever is difficult because the symptoms are very similar to many other illnesses and vary greatly from person to person. The diagnosis may be suspected in people who have risk factors or who live in an area where Q fever is common.
To confirm the diagnosis, a blood sample may be tested to check for antibodies to the bacteria. Because antibody levels can remain high for many years after a person is infected, elevated antibody levels do not necessarily mean that the patient is acutely infected at that time. Samples should be tested again after a few weeks to look for changes in antibody levels, which confirm the diagnosis of acute infection.
Samples may also be sent for PCR (polymerase chain reaction) testing, which can detect infection earlier than antibody tests, but this method is not always available. People who test positive for acute infection should undergo follow-up testing for two years to monitor the progression of chronic Q fever infection.
For chronic infection, the diagnosis can also be made by testing tissue from infected heart valves if they have been removed and replaced surgically.
Culturing Coxiella burnetii from serum or tissue is possible, but requires special laboratory facilities due to the highly infectious nature of the organism. Once a diagnosis of Q fever is made, it must be reported to the state department of health.
Approaches to the diagnosis and treatment of rheumatism
Clinical guidelines for the diagnosis of acute rheumatic fever require an adequate assessment of symptoms, laboratory changes, recent bacterial infections, and family history.
Criteria for diagnosis include such manifestations as arthritis, cardiac damage, chorea, subcutaneous nodes and rash (major diagnostic signs). Minor signs are considered individual symptoms (joint pain, fever), specific laboratory changes and instrumental examination data.
Laboratory diagnosis of rheumatic fever is based on determining:
- ESR (increased);
- leukocytes (increased with a shift towards younger forms);
- C-reactive protein (not normally detected);
- antistreptococcal antibodies in increased quantities;
- microbe by bacteriological seeding of the tonsil contents.
Characteristic changes in the ECG are: an increase in the duration of the PQ interval, rhythm disturbances, etc. Additionally, an ultrasound of the heart is performed, showing the presence of a defect, myocarditis, and inflammation of the pericardium.
Treatment of acute rheumatic fever depends on the stage of the process, its activity, and the severity of symptoms. During the attack, hospitalization in the rheumatology department or cardiology is necessary. For the first 2-3 weeks, bed rest is indicated, which expands as the improvement continues. The duration of hospitalization can be up to one and a half months.
Appointed:
- Desensitizing agents - fenkarol, claritin, parlazin;
- Anti-inflammatory therapy - diclofenac, ibuprofen, indomethacin;
- Glucocorticosteroids - prednisolone, dexamethasone;
- Immunosuppressive therapy - chloroquine, azathioprine;
- Antibacterial therapy - drugs of the penicillin group (if the presence of infection is proven).
Antibiotics used to treat acute rheumatic fever are benzylpenicillin, azithromycin, clindamycin, clarithromycin, roxithromycin. In case of penicillin intolerance, macrolides and lincosamides are used.
When the defect and heart failure are formed, treatment is similar to that for these complications: diuretics, beta-blockers, cardiac glycosides, antiarrhythmic drugs, ACE inhibitors, etc.
After inpatient treatment, patients are observed by a cardiologist or rheumatologist at their place of residence, undergo regular tests, and undergo an ECG. Spa treatment in specialized sanatoriums, taking multivitamins, and a diet with sufficient protein but limited salt are indicated.
Acute rheumatic fever is one of those diseases that can be prevented through appropriate preventive measures. Primary prevention includes timely search and elimination of foci of streptococcal infection, strengthening the immune system, hardening, and a healthy diet.
Secondary prevention is carried out by administering bicillin to those patients who have already experienced an attack of rheumatism:
- For five years to all patients (without carditis);
- Until the 25th birthday or 10 years in case of an attack with carditis, but without a defect;
- Lifelong for rheumatism with heart disease.
Current prophylaxis with antibiotics and anti-inflammatory drugs is indicated for acute associated infections associated with rheumatism.
The prognosis for acute rheumatic fever in case of timely diagnosis and early initiation of treatment is favorable. If the disease has been neglected, a defect has developed, it becomes doubtful, and in the case of chronic circulatory failure - unfavorable.
Symptoms of fever and fever
An increase in body temperature in most cases is accompanied by the following symptoms:
- There is a feeling of heat in the head, and if you touch the patient’s forehead with your lips, you feel increased hotness of the skin;
- general malaise of the body, increased fatigue, weakness;
- aching in the limbs, as if someone were twisting their arms and legs;
- muscle pain;
- pain in the eyes and their redness, sometimes there is a kind of “shine” in the eyes;
- headache, dizziness;
- chills;
- increased fluid loss - sweating, urge to go to the toilet;
- body cramps;
- delusions and hallucinations, especially at night;
- heart and respiratory failure
- Enlargement of the lymph nodes (lymphadenopathy), which can turn into inflammation (lymphadenitis).
At the same time, if the temperature rises too high, it depresses the activity of the central nervous system (CNS). Heat leads to dehydration, poor circulation in internal organs (lungs, liver, kidneys), and leads to a decrease in blood pressure.
How is fever treated?
Fever is a symptom, not a disease in itself. The most important treatment approach is to identify the underlying cause. In some cases, such as viral infections, it is self-limiting - disappearing after the infection is removed.
The temperature is reduced by using drugs belonging to the group of antipyretics. Among them, acetaminophen (paracetamol as referred to in some countries) is a safe, effective treatment for fever.
Aspirin is used in adults but should be avoided in children. Other drugs, such as ibuprofen, diclofenac, can also be used instead of acetaminophen.
Treatment of Q fever
Acute Q fever is treated with antibiotics (usually doxycycline ) for 14 days. Pregnant women with acute Q fever should take the antibiotic trimethoprim / sulfamethoxazole (Bactrim, Septra) from diagnosis until 32 weeks of pregnancy. Treatment for chronic Q fever is longer and usually requires several months to several years of antibiotics.
Photo: qimono/Pixabay
Outpatient
After visiting a doctor, the woman underwent an outpatient examination. Tests showed mild anemia - Hb 102 g/l (normal 110–160 g/l) and hematocrit 32.2% (normal 35–47%). The number of leukocytes and platelets, as well as the leukocyte formula, were normal. At the same time, inflammatory markers turned out to be elevated: ESR 135 mm/h (normal
X-rays of the chest and legs showed no pathological changes, including fractures.
Doctors immediately ruled out a urinary tract infection: a bacteriological examination of urine showed no growth of cultures.
Types of disease
Depending on the degree of temperature increase, the following types of fever are distinguished:
- Subfibrality (37-37.9°C)
- Moderate (38-39.9 °C)
- High (40-40.9 °C)
- Hyperpyretic (from 41°C)
Based on the nature of temperature fluctuations, fever is divided into the following types: Constant fever. High temperature for a long time. The temperature difference in the morning and evening is no more than 1°C.
Relieving fever (remitting). High temperature, morning low above 37°C. Daily temperature fluctuations are more than 1-2°C.
- Wasting fever (hectic). Large daily temperature fluctuations (3-4 °C), which alternate with a decrease in temperature to normal levels and below. Accompanied by severe sweating.
- Intermittent fever (intermittent). Short-term increases in temperature to high levels alternate with periods of normal temperature
- The reverse type of fever is when the morning temperature is higher than the evening temperature.
- Irregular fever (atypical) - varied and irregular daily fluctuations.
Fever is classified according to its form:
- Undulating fever (undulating). Periodic increases in temperature, and then a decrease to normal levels for a long time.
- Relapsing fever is a strict, rapid alternation of periods of high temperature with fever-free periods.