Tularemia is a disease of a natural focal nature, manifested as an acute infection. Tularemia, the symptoms of which include damage to the lymph nodes and skin, and in some cases, the mucous membranes of the pharynx, eyes and lungs, is also distinguished by the symptoms of general intoxication.
Online consultation on the disease “Tularemia”. Ask a question to the experts for free: Infectious disease specialist.
- Description of the disease
- Features of transmission of the causative agent of tularemia
- Course of tularemia
- Forms of tularemia
- Symptoms of tularemia
- Complications of tularemia
- Diagnosis of tularemia
- Treatment of tularemia
general description
The causative agent of the disease is Francisella tularensis, a gram-negative aerobic rod bacterium. It is noteworthy that the tularemia bacillus is an extremely tenacious microorganism, and its viability in water is possible at a temperature corresponding to 4°C for about a month. In grain and straw, when the temperature corresponds to zero, the viability of the microorganism can be about six months; at 20-30 degrees, the survival of the microorganism is possible for 20 days, and in the skins of animals that died from tularemia, the bacterium can live up to a month at a temperature of 8-12 degrees. The death of bacteria occurs when they are exposed to high temperatures, as well as disinfectants.
Birds and wild rodents, including some species of mammals (sheep, dogs, lagomorphs, etc.), act as a reservoir of infection, as well as its source. The most significant contribution to the spread of this infection is observed in rodents (muskrat, vole, etc.). As for humans as a spreader of infection, they are not contagious.
In the transmission of bacteria, the most common mechanism is a transmissible mechanism. In this case, the microbe enters the animal’s body through the bite of a blood-sucking animal or tick. The typical route of infection for the disease is infection through the bite of an ixodid tick.
Considering the prevalence of tularemia, it should be noted that susceptibility to this disease is 100%. The majority of susceptibility to infection is observed among men, and those whose profession predisposes them to direct contact with animals. Territorial foci are formed during the migration of infected rodents. Tularemia is mainly relevant for rural areas, but in recent years there has been a clear trend towards an increase in incidence in urban areas.
Varying degrees of increase in incidence are observed year-round, while each time of year is characterized by the manifestation of the disease in its specific form. This is explained by etiological factors. A significant number of morbidity episodes are observed in the autumn period, meanwhile, vector-borne outbreaks of tularemia associated with haymaking and harvesting work in the fields often appear in the period July-August.
Epidemiology
Sources of infection among vertebrate animals in natural conditions are rodents and hares. In the Soviet Union, the natural reservoir of the pathogen is found in wild vertebrates (82 species). All animals are divided into three groups according to the degree of susceptibility and sensitivity to tularemia. It is created by some small mammals that are especially sensitive to this disease (mammals of group I): vole, house mouse, muskrat, hare, hamster, etc. The internal organs, blood and secretions of sick or dead mammals have many tularemia microorganisms.
Mammals of group II are small animals (ground squirrel, squirrel, rats, field mouse, Far Eastern voles) that are less sensitive to the disease.
Mammals of group III are the least susceptible to this disease: carnivores: fox, raccoon dog, ferret, and domestic cats and dogs. They are practically unimportant as sources of the tularemia pathogen.
Transmission of this pathogen among mammals is carried out through vector-borne arthropods, especially ixodid ticks, mosquitoes, and, to a lesser extent, fleas and gamasid ticks. Along with the blood route, a secondary role is played by food and contact infection (skin and mucous membranes), through water that contains the secretions of an infected animal.
Features of transmission of the causative agent of tularemia
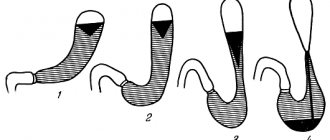
Below is a diagram indicating the characteristics of disease transmission depending on the metamorphotic development of the tick.
Features of transmission of the causative agent of tularemia depending on the metamorphosis of the tick
The number “1” indicates infection of tick larvae through small mammals with tularemia. The number “2” determines the next cycle, in which nymphs that have molted from larvae transmit the pathogen to small mammals. “3” indicates the transmission of the infectious agent by mature ticks that have molted from nymphs to large mammals.
Prevention
Important! The main method of prevention is vaccination of people with tularemia vaccine in epidemically disadvantaged areas. Lasting immunity lasts up to seven years, so re-vaccination is carried out after five years. If there is a threat of an epidemic, emergency prevention is possible by administering antibiotics intravenously.
Anti-epidemic measures include suppression of possible routes of transmission of the tularemia pathogen and disinfection of sources of infection. In epidemically disadvantaged areas, at agricultural enterprises and catering facilities, a full range of measures is carried out to combat the spread of infection (disinfection, disinfestation, deratization).
It is necessary to pay special attention to individual protection from the causative agent of tularemia for people involved in hunting wild animals, especially in the process of skinning and butchering carcasses and for people taking part in deratization activities when collecting rodent corpses. Hands must be protected with rubber gloves, after removing which it is imperative to disinfect the skin. Water may only be consumed from reliable, verified sources.
If a patient with tularemia is identified, then all things that could be infected must be disinfected.
Tularemia is a dangerous disease that requires mandatory treatment. Only constant monitoring of the patient by doctors and competently administered therapy ensure complete recovery without complications.
Konev Alexander. Therapist
9, total, today
( 192 votes, average: 4.71 out of 5)
Proteus infection: symptoms, treatment and prevention
SARS caused by coronavirus: symptoms, treatment, risks - outbreak in China in January 2020
Related Posts
Course of tularemia
Penetration of the pathogen occurs through the skin, even if it is not damaged. As we have already indicated, the areas for penetration are the mucous membranes of the respiratory tract and eyes, as well as the gastrointestinal tract.
The area of the so-called entry gate primarily determines the clinical features of the course of tularemia. Often in this area, the development of primary affect occurs, in which the sequence of spots, papules, vesicles, pustules and ulcers replacing each other becomes relevant. Somewhat later, tularemia bacilli enter the area of regional lymph nodes, in which their subsequent multiplication occurs with the simultaneous development of the inflammatory process. It should be noted that the inflammatory process is accompanied by the formation of a primary bubo (that is, an inflamed lymph node). The death of Francisella leads to the release of the lipopolysaccharide complex (endotoxin), which, in turn, increases local inflammation and provokes the development of intoxication when it enters the blood.
With hematogenous dissemination, generalized forms of infection develop, occurring with characteristic toxic-allergic manifestations. In addition, secondary buboes are also formed, and various systems and organs are affected (in particular, the lungs, spleen and liver). In the area of the lymph nodes, as well as internal organs that have been damaged, a specific type of granuloma is formed in combination with central areas of necrosis. There is also an accumulation of granulocytes, lymphoid and epithelial elements.
The formation of granulomas is predisposed by the incomplete process of phagocytosis, which is determined by the characteristics of the properties of the pathogen (in particular, there are factors that prevent killing within cells). Often the formation of granulomas in primary buboes leads to the formation of suppuration in them, followed by spontaneous opening. This process is characterized by prolonged healing of the resulting ulcer.
As for secondary buboes, for them, as a rule, suppuration is not a characteristic sign. When necrotic areas that have arisen in the lymph nodes are replaced with connective tissue, suppuration does not occur, but the buboes become sclerotic or dissolve.
Forms of tularemia
The clinical classification of the disease in question identifies the following forms:
- In accordance with the localization of the local process:
- Tularemia bubonic;
- Ulcerative bubonic tularemia;
- Tularemia oculobubonic;
- Tularemia angino-bubonic;
- Pulmonary tularemia;
- Tularemia abdominal;
- Generalized tularemia.
- Acute tularemia;
- Protracted tularemia;
- Recurrent tularemia.
- Tularemia is mild;
- Moderate tularemia;
- Tularemia is severe.
What it is?
Tularemia is an infectious natural focal pathology with an acute course, characterized primarily by damage to the organs of the lymphoreticular system, skin, mucous membranes of the pharynx and pulmonary parenchyma with a pronounced intoxication symptom complex.
The first mention of a disease clinically reminiscent of the bubonic plague dates back to 1910, which after numerous scientific studies was called “tularemia.” Vaccination had not yet been carried out in those days, and due to the high natural susceptibility of people to the causative agent of this pathology, reaching almost 100%, with each contact of a healthy person with a source of infection, vivid clinical symptoms of tularemia developed.
Tularemia: symptoms
The duration of the incubation period is about 1-30 days, but most often it is 3-7 days.
General signs characteristic of tularemia, and, accordingly, signs characteristic of any of its clinical forms, are manifested in an increase in temperature (up to 40 ° C) and in symptoms indicating intoxication (headache, muscle pain, chills, weakness, anorexia - lack of appetite, in which its complete absence is noted). Most often, the fever has a remitting nature, as well as a constant, wavy or intermittent nature. The duration of the fever can be about a week, but it can also last for two to three months. Meanwhile, its duration mainly fluctuates within three weeks.
Examination of patients indicates hyperemia and general pastiness of the face (that is, whitening of the skin in combination with loss of elasticity, caused by mild swelling), and hyperemia (redness) of the conjunctiva is also observed. In frequent cases, the appearance of exanthema of one nature or another (maculopapular, erythematous, vesicular, roseolous or petechial) becomes possible. Pulse is rare, blood pressure is low. After several days from the onset of the disease, the development of hepatolienal syndrome is noted.
It should be noted that the development of one or another clinical form of tularemia is determined based on the mechanism of infection, as well as the entry gates of infection, which, as we noted, indicate the local localization of the process. the bubonic form develops , which manifests itself, accordingly, in the form of lymphadenitis (bubo), regional in relation to the gate of infection. Lymphadenitis refers in particular to inflammation of the lymph nodes.
In addition, a combined or isolated lesion becomes possible, which affects various groups of lymph nodes (inguinal, axillary, femoral). Hematogenous dissemination of pathogens can also contribute to the formation of secondary buboes. This is accompanied by pain and subsequent enlargement of the lymph nodes, which can reach the size of a hazelnut or a small chicken egg. Gradually, pain reactions in their manifestations decrease, and then disappear altogether. The contours characteristic of the bubo do not lose their distinctness; minor manifestations of periadenitis are noted. The dynamics of tularemia are characterized by slow resorption and suppuration with the appearance of a fistula, this is accompanied by the release of creamy pus.
Ulcerative-bubonic form. The development of this form occurs predominantly in the case of vector-borne infection. The place where the microorganism has been introduced is characterized over the course of several days by the sequential replacement of such formations as a spot and a papule, a vesicle and a pustule, after which a shallow type of ulcer with slightly raised edges is formed. Its bottom is covered with a dark-colored crust; its shape resembles a “cockade.” In parallel with this, the development of regional lymphadenitis (bubo) also occurs. Subsequently, the ulcer scars at an extremely slow pace.
When the bacterium penetrates through the conjunctiva, the oculobubonic form of the disease is formed. This is accompanied by damage to the mucous membranes of the eye, which occurs on the principle of conjunctivitis, formations of the papular type, and then formations of the erosive-ulcerative type when yellowish pus is released from them. The process of corneal damage in this case is an extremely rare phenomenon. These symptoms are accompanied by severe swelling of the eyelids, as well as regional lymphadenitis. The severity and duration of the disease are noted.
Anginal-bubonic form. Its development occurs when the pathogen penetrates through water or food. There are complaints from patients about manifestations in the form of moderate sore throat, difficulty swallowing. Examination reveals hyperemia of the tonsils, their increase in size, and swelling. In addition, they are fused with the fiber surrounding them. The surface of the tonsils (mainly on one side) is covered with a grayish-white necrotic coating, which is difficult to remove. Severe swelling of the tongue and arches is observed. As the disease progresses, the tissue of the affected tonsil is destroyed with the formation of long-healing and fairly deep ulcers. The concentration of tularemic buboes covers the cervical, parotid and submandibular regions, which mainly corresponds to the side of the almond lesion.
Abdominal form. Its development occurs due to lesions in the area of the mesenteric lymph nodes. Symptoms include severe abdominal pain, and in some cases, vomiting and anorexia. Diarrhea is also noted in some cases. Palpation determines pain in the navel area; symptoms indicating irritation of the peritoneum cannot be ruled out. In addition to the listed symptoms, hepatolienal syndrome also occurs. Palpation of mesenteric lymph nodes is possible in rare cases; their enlargement is determined using an examination method such as ultrasound.
Pulmonary form. Its course is possible in bronchitis or pneumonia.
- Bronchitic course. This option is caused by damage to the paratracheal, mediastinal and bronchial lymph nodes. It is characterized by moderate intoxication and dry cough, pain in the chest area. Dry rales are noted when listening to the lungs. As a rule, this course is characterized by its own ease, and recovery occurs within 10-12 days.
- Pneumonic course. It is characterized by an acute onset, the course of the disease in this form is debilitating and sluggish, and fever is an accompanying symptom for a long time. The pathology that forms in the lungs has manifestations in the form of focal pneumonia. Pneumonia is distinguished by the severity and acyclicity of its course, as well as the tendency to subsequent development of complications (segmental, lobular or disseminated pneumonia with a characteristic enlargement of the lymph nodes of one or another of the listed groups, as well as pleurisy and cavities, including gangrene of the lungs).
Generalized form. Its clinical manifestations are similar to typhoid-paratyphoid infections or severe sepsis. Fever is characterized by the intensity of its manifestations and its long-term persistence. Symptoms of intoxication (chills, headache, weakness, muscle pain) also become pronounced. Lability (variability) of the pulse, muffled heart sounds, and low blood pressure are noted. In the vast majority of cases, the first days of the disease occur with the development of hepatolienal syndrome. Subsequently, it becomes possible to form an exanthema of a persistent roseolous petechial nature when the elements characteristic of the rash are localized in the area of symmetrical areas of the body (hands, forearm, foot, lower leg, etc.). This form does not exclude the possibility of the development of secondary buboes, which are caused by the dissemination (spread) of the pathogen, as well as the dissemination of specific metastatic pneumonia.
Instructions for use
Before administering the drug, you should carefully study the instructions for it, learn about the composition, vaccination rules and possible side effects.
When is the vaccine given?
It is recommended to carry out preventive measures two to three weeks before possible interaction with the source of infection (on the eve of a trip to a region with a high incidence, due to the nature of the activity). However, this is not always possible, especially when it comes to agricultural workers. They are usually grafted at the beginning of the working season.
Dosage rules and administration technique
There are two ways to administer the drug.
- Cutaneous.
- Subcutaneous.
In the first case, the vaccine is diluted with water for injection (0.1 ml). Then the ampoule is shaken so that the liquid becomes homogeneous. The resulting solution is applied to the skin in the middle third of the shoulder. Application is carried out with a sterile pipette in two places at a distance of 30-40 mm. The skin at the vaccination site is stretched, two 10 mm incisions are made, into which the drug is rubbed when blood appears. You should wait 10 minutes until it dries.
When administered subcutaneously, the medicine is diluted in the same way as in the first case. 1 ml of solution is drawn into a syringe, and 19 ml of sodium chloride is added to it. In a dose of 0.1 ml, the drug is injected into the upper third of the shoulder.
Diagnosis of tularemia
The use of nonspecific laboratory techniques (urine and blood tests) determines the presence of signs characteristic of inflammation and intoxication. In the first days of its course, the disease manifests itself in neutrophilic leukocytosis in the blood, then a drop in the total number of leukocytes is observed. At the same time, the concentration of monocyte and lymphocyte fractions increases.
Serological specific type diagnostics is carried out using RNGA and RA. The progression of the disease is characterized by an increase in antibody titer. Determination of tularemia becomes possible already on the 6-10th day from the moment of its onset, for which immunofluorescence analysis (ELISA) is used. This serological test in relation to diagnosing tularemia is characterized by the greatest sensitivity. As for the possibility of earlier diagnosis of the disease (its first days), it is possible using PCR.
A very specific and, at the same time, rapid diagnosis is made using a skin allergy test, which is performed using tularemic toxin. The result is determined by 3-5 days of illness.
Treatment of tularemia
Treatment of tularemia is carried out exclusively in a hospital setting, and discharge is made only after complete recovery from the disease. Specific therapy is used in the form of a course of antibiotics. Intoxication symptoms are relieved using therapy oriented in this direction in combination with antipyretic and anti-inflammatory medications. Additionally, antihistamines and vitamins are prescribed. In some cases, if necessary, drugs are also used to normalize cardiovascular activity.
Sterile dressings are used for skin ulcers. The festering buboes are opened and drained
If symptoms characteristic of tularemia occur, you should contact an infectious disease specialist.
Contraindications to vaccination
Not all children are allowed to be vaccinated against tularemia. The following situations are contraindications:
- previous tularemia;
- allergy to a vaccine component;
- acute infectious disease;
- exacerbation of a chronic disease;
- oncology education;
- blood diseases;
- chronic skin disease;
- reduced immunity;
- diabetes;
- elevated temperature.
In certain conditions (for example, acute infectious disease), vaccinations are contraindicated
Some of these contraindications completely exclude the introduction of the vaccine (for example, allergies or a history of tularemia). Others suggest simply postponing vaccination (acute infection, exacerbation of a chronic illness, etc.). In any case, the child’s condition is carefully assessed by the attending physician before the proposed vaccination.