Prolactin plays a key role when a woman begins lactation after giving birth. It promotes the maturation of colostrum, and then its transformation into full-fledged milk. But even in non-pregnant women, this hormone does not disappear anywhere, and has a noticeable effect on the maturation of the egg in the first phase of the menstrual cycle.
If prolactin is elevated, this can cause infertility, and with low values, a woman may not only experience problems conceiving a child, but also experience irregular menstruation.
The endocrine system is designed in such a way that the production of the hormones FSH and LH, the action of which is aimed at the maturation of the dominant follicle in the ovary, directly depends on the increase in prolactin levels. The higher its level, the more the production of luteinizing and follicle-stimulating hormones is inhibited.
Features of hormone secretion and its effect on the body
How is this hormone produced?
Prolactin is secreted by pituitary cells, breast tissue, and if a woman is pregnant, then by placental tissue. The production and synthesis of the hormone is directly dependent on estrogen: the higher the level of female sex hormones in the blood, the greater the production of prolactin.
That is why in non-pregnant and non-lactating patients with an excess amount of estrogen, colostrum may be released when pressing on the mammary gland.
The effect of increased prolactin on the first phase of the cycle
If the hormone level is at the upper limit of normal or exceeds it, then processes of inhibition of egg maturation are initiated. The higher the lactogenic hormone, the more suppressed the production of FSH and LH. Therefore, a woman during breastfeeding has some protection from unwanted pregnancy.
However, it is not worth using this hormonal imbalance as the main means of protection: if before lactation FSH and LH were also at the upper limit of normal or exceeded it, then the high level of prolactin during breastfeeding will not be able to inhibit the process of egg maturation and ovulation will occur anyway.
Accordingly, if a non-pregnant and non-lactating patient has an increased level of lactogenic hormone, then using ultrasound folliculometry the doctor will diagnose regular anovulatory monophasic menstrual cycles.
The effect of increased prolactin on the second phase of the cycle
High levels of lactogenic hormone have a negative effect on the luteal phase, in particular on the functioning of the corpus luteum. If a woman’s prolactin is normal, then the length of the period from the moment of ovulation until the start of a new cycle is no more than 12-14 days.
- If the hormone is more than normal, then the second phase of the cycle is delayed.
Sex hormone prolactin
Other names for this substance are lactotropic, lactotropin, mammotropin. Produced by the pituitary gland under the influence of other hormones (endorphin, oxytocin, thyrotropin).
The main effect is on the development and functioning of the mammary glands in women. Also involved in the process of ovulation, regulation of the menstrual cycle, synthesis of other sex hormones, and sperm formation.
Reasons for increased prolactin in women
Why might prolactin be elevated?
An increase in the level of lactogenic hormone, which is diagnosed over a long period of time, is dangerous for the patient’s health - such a hormonal imbalance can provoke a malignant breast tumor. Before prescribing treatment, the doctor needs to find out what caused the hyperfunction of the pituitary gland and mammary gland tissue. There may be several reasons for increased prolactin in women:
- Features of physiological processes are considered natural hyperprolactinemia. Hormone levels increase during sleep, pregnancy or lactation.
- Pituitary tumors or hypothalamic tumors. Since these parts of the brain are responsible for the production of the lactogenic hormone, their dysfunction leads to increased production of prolactin.
- PCOS is diagnosed using ultrasound of the ovaries and tests for the hormones DEHA and 17 dihydroprogesterone. Ovarian dysfunction can cause hyperprolactinemia, especially in cases where the woman does not receive any hormonal treatment for the primary disease.
- Use of antihistamines or drugs containing estrogens.
- Diagnostic uterine curettage, non-drug termination of pregnancy.
- Chronic kidney diseases.
- Dysfunction of the adrenal cortex, due to which the level of androgens, estradiol and, as a result, prolactin may increase.
Detection of symptoms of increased prolactin depends on how much the hormone level exceeds normal values. With minor deviations, the disease does not have clear signs.
If an excess amount of the hormone enters the blood for a long time, then hyperprolactinemia manifests itself in the following:
- Regular menstrual irregularities
- No menstrual bleeding
- Infertility
- The release of milk from the breast, not associated with feeding the baby.
- Decreased sexual desire
- Excessive hair growth (hirsutism)
- Excess body weight
- Development of osteochondrosis, decrease in bone density
- Long-term depression
Symptoms of elevated prolactin in women intensify if the cause of hormonal dysfunction is pituitary tumors.
Diagnosis of pathology
If two or three of the above symptoms appear, a woman needs to check her prolactin level. To obtain an accurate result, it is recommended to donate blood at least twice, excluding the following factors that affect hormonal synthesis:
- Stressful situations;
- Excessive physical activity, sports;
- Painful sensations;
- Overeating or starvation, an abundance of protein and carbohydrate foods;
- Having sex, sexual stimulation of nipples and areolas;
- Drinking alcohol, smoking;
- Thermal procedures - taking a bath, visiting a sauna;
- Lack of sleep.
If the above factors cannot be avoided, it is recommended to postpone the analysis to three days later. If a woman is taking medications that affect prolactin synthesis, the medications must be discontinued. If it is impossible to stop the medication, you should warn your doctor to avoid distorting the test results.
A referral for testing can be issued by any specialist to whom the patient has addressed with complaints. The study is carried out in the morning, no later than 3 hours after waking up - preferably between 9 and 11 am. Hormonal analysis is carried out strictly on an empty stomach, you are only allowed to drink a couple of sips of still water. The accuracy of the study does not depend on the day of the menstrual cycle, but some doctors advise checking prolactin levels on days 5–8 of the cycle.
Prolactin levels are not stable and sudden hormonal fluctuations are possible. If the lactotropic hormone is exceeded by 1.5 - 2 times, but there are no pathological symptoms, it is recommended to retake the test after 2 - 3 weeks.
In addition to hormonal analysis, the examination includes the following diagnostic measures:
- MRI, CT or x-ray of the skull in two projections - to exclude a pituitary tumor;
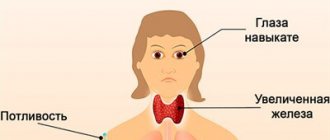
- Ultrasound of the thyroid gland - to exclude hypothyroidism;
- Pregnancy test or ultrasound examination of the pelvic organs – for women of reproductive age to exclude pregnancy;
- Biochemical blood test - to determine the condition of the kidneys and liver;
- Ophthalmological examination;
- Gynecological examination;
- Hormonogram - to exclude endocrine pathologies. Usually it is prescribed to test hormones such as: TSH, LH, FSH, somatomedin-S, macroprolactin.
Prolactin norms by age and cycle phases
A blood test for prolactin should be taken from the 3rd to the 5th day of the menstrual cycle if the purpose of the examination is a general determination of the level of this hormone in the blood. But in some cases, the gynecologist needs to look at his behavior over time, and then a blood test must be taken three times per cycle: in the first phase, during ovulation and in the second phase. The table of prolactin norms in women in this case will be as follows:
- Follicular phase – 136 – 999 mIU/ml. This is the time of maturation of the dominant follicle, growth of the endometrium and accumulation of estradiol concentration, which directly affects the gradual increase in the lactogenic hormone.
- Ovulation phase – 190 – 1484 mIU/ml. This phase is short, lasting only a day (exactly as long as the egg lives). To be sure that it has begun, you need to visit an ultrasound room. The folliculometry procedure can quite accurately calculate the time after which ovulation will begin - then you need to take a blood test for prolactin.
- Luteal phase – 148 – 1212 mIU/ml. The body is preparing for a possible pregnancy, so the concentration of lactogenic hormone will be higher than in the two previous phases. Many women report pain in their breasts.
In addition to the phases of the menstrual cycle, prolactin levels in women should be distinguished by age:
- Children's age (7-10 years) – 40 – 400 mU/l
- Youth and childbearing age – 40 – 600 mU/l
- Menopause – 25 – 400 mU/l (trend to constant decrease).
In order for the blood test to be highly accurate, you must follow the rules for preparing for it:
- Abstain from sexual intercourse 2 days before going to the treatment room.
- Staying awake for more than 4 hours before donating blood (prolactin concentration increases during sleep).
- The last meal should be 9–10 hours before the test.
- You should not rub or knead your breasts - this can stimulate a short-term increase in hormone levels.
The importance of prolactin in the female body
In the female body, this hormone plays a major role in the reproductive and menstrual functions of the body and is found in three fractions: monomeric, dimeric and three-dimensional prolactin. Monomeric prolactin has the highest activity, the concentration of which reaches 80% compared to other fractions. Synonyms for prolactin are mammotropin or lactotropic hormone (LTH).
The leading functions of mammotropin in the female body:
stimulating the growth and development of the mammary glands during puberty and gestation;- secretion of colostrum during pregnancy, and after childbirth of milk;
- maintaining progesterone levels during gestation;
- regulation of the second phase of the menstrual cycle;
- regulation of the composition of amniotic fluid;
- participation in metabolic processes;
- maintaining water-salt balance;
- participation in achieving orgasm;
- increasing the threshold of pain sensitivity (reduces pain during childbirth);
- suppression of ovulation during the first 6 months after childbirth and breastfeeding;
- formation and maintenance of maternal instinct;
- participation in immune processes.
Treatment regimens for elevated prolactin
What to do in this case?
The type of therapy directly depends on what causes the disease. Treatment of elevated prolactin can be medicinal and surgical.
You should consult a doctor in any case, because a constant strong deviation from the norm of the lactogenic hormone can lead to serious consequences.
Physiological increase in hormone
In this case, no therapy is carried out, since a short-term change in blood parameters does not cause any harm to the body. If hyperprolactinemia is caused by lactation, which needs to be artificially interrupted, the doctor will prescribe medications such as Bromocriptine or Cabergoline.
Under no circumstances should the breast be bandaged, as this will lead to stagnation of milk and the formation of tumors, which can subsequently become malignant.
Increased hormone levels when taking medications
If prolactin has increased due to taking antiemetics, estrogen-containing or antihistamines, then treatment will be the abolition of these drugs. The hormone level should return to normal within 3 to 5 days.
If a blood test shows that there has been no decrease in the concentration of the lactogenic hormone, you need to consult a doctor who will decide on the advisability of taking medications to reduce its production.
Pathological hyperprolactinemia
As a rule, this type of disease is the most difficult to correct. Often the impossibility of a complete cure is associated with a general hormonal imbalance. The most effective in this case is considered to be drug treatment, which can be carried out with drugs used for elevated prolactin: Bromocriptine, Cabergoline or Quinagolide.
The first two of them are derivatives of ergot ancaloids. The results of the study revealed that patients tolerate treatment best with Quinagolide, which is considered more effective than Bromocryptonide.
Surgical help is resorted to only when drug treatment does not bring results. During surgery, the breast adenoma is removed - however, doctors note that after this there is a considerable likelihood of relapses, especially in patients with intolerance to medications to correct elevated lactogenic hormone.
Causes of elevated levels of lactotropic hormone
An increase in the concentration of mammotropin is called hyperprolactinemia. Scientists distinguish between pathological and physiological increases in hormonal levels. With physiology, a female representative requires only periodic medical observations over time - no therapy is needed.
Physiological causes of abnormal prolactin production:
- Gestation, breastfeeding;
- Having sex;
- Frequent stressful situations, psychological trauma;
- Neonatal period (first 28 days after birth);
- Adverse habits – alcohol and tobacco abuse;
- Intense physical activity and sports;
- Strict hypoglycemic diet;
- Nipple stimulation;
- Massaging the cervical-collar area;
- Chronic lack of sleep;
- Malnutrition, poor nutritional diet.
In addition, lactotropic hormone increases when:
- Visiting a bathhouse, sauna, solarium;
- Sharp pain of various localization and etiology;
- Taking strong medications: narcotic and psychotropic drugs, oral contraceptives, antibiotics, sleeping pills.
If the reason for the increase in the concentration of a hormonal substance is not determined, it is called idiopathic hyperprolactinemia. In pathology, hyperfunction of pituitary cells occurs without changing their number.
Pathological causes of hyperprolactinemia:
- Tumors on the brain appendages - the hypothalamus, pituitary gland, most often - prolactinoma;
- Diseases of the hypothalamus;
- Hypothyroidism – weakening of thyroid function;
- Polycystic disease;
- Chest injury;
- Surgical intervention on the organs of the chest cavity;
- Herpes zoster (shingles);
- Autoimmune pathologies – systemic lupus erythematosus;
- Weakness of the cerebral diaphragm – intussusception of the subarachnoid space;
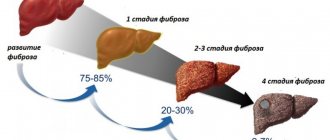
- Chronic liver failure;
- Brain infections;
- Acute renal failure, hypocortisolism;
- Cirrhosis of the liver.
Pathological hyperprolactinemia is divided into two subtypes:
- Functional – does not produce organic changes. This type includes complications and severe consequences of diseases;
- Organic – emerging ailments lead to morphological changes in tissues.
Forms of hyperprolactinemia
Depending on the cause, hyperprolactinemia occurs:
- primary – caused by pathological processes in the hypothalamus or pituitary gland;
- secondary – develops against the background of other diseases;
- idiopathic – the mechanism of development cannot be determined.
In addition, the following forms of pathology are distinguished by origin:
- asymptomatic hyperprolactinemia;
- hyperprolactinemic hypogonadism (prolactin-secreting pituitary adenomas, idiopathic forms);
- symptomatic hyperprolactinemia (alcohol, drug, psychogenic, neuro-reflex);
- extrapituitary secretion of prolactin;
- hyperprolactinemia due to other hypothalamic-pituitary diseases (empty sella syndrome, hormonally inactive sellar and parasellar neoplasms, cerebrovascular accident, syphilis, tuberculosis);
- combined forms of hyperprolactinemia.
Traditional methods of treatment
Currently, several methods have been developed for the treatment of elevated prolactin in the blood. The choice of method will depend on the suspected cause that led to the development of this condition, as well as the state of the reproductive system and plans for further childbearing.
Treatment includes the use of medications, the use of surgical methods, as well as lifestyle changes and the inclusion of traditional methods of therapy.
Among the components of drug therapy, drugs are used aimed at reducing the level of prolactin in the blood.
These are drugs from the group of dopamine agonists, which are also classified as dopaminomimetics. This substance is a neurohormone with high biological activity that regulates prolactin not only in the blood, but also in the cells responsible for their production.
Dopamine is the main active ingredient in many drugs.
Since prolactin is currently classified as a stress hormone, therefore, the use of non-drug methods in the treatment of this pathological condition should limit the impact of stress on the body:
- To limit their effect on the body, it is recommended to include aromatherapy, which has a relaxing effect, in your lifestyle.
- Be sure to normalize sleep, as well as physical activity and increase rest time.
- Eliminate exposure to bad habits.
- If you have increased nervous tension, it is recommended to include gymnastics and massage in your regimen.
https://www.youtube.com/watch?v=-1AzeHBs9IU
Indications for surgical intervention are:
- Ineffectiveness of conservative treatment;
- Progression of the pathological condition;
- Complications from the visual or nervous system.
Surgical intervention in the presence of pituitary adenoma is a minimally invasive method. It is produced through the nasal passage. This removes the pathological tissue from the pituitary gland.
There are several types of access for surgical treatment:
- Subfrontal – effective for suprasellar adenoma, which is prone to rapid growth.
- Rhinoseptal - used in case of compression of the optic chiasm by adenoma.
A few days before removal of the prolactinoma, the patient should stop taking bromocriptine. The drug is resumed immediately after surgery if the tumor is large and only part of it was excised.
Treatment is considered successful if, 2 hours after the operation, a normal prolactin level in the blood is recorded, and after 40 days the operated woman ovulates. However, the risk of relapse of the disease some time after a successful operation cannot be excluded.
It is important to remember that traditional medicine serves only as an addition to therapy, and not as a treatment for prolactinoma in women. In addition, before using this or that product, you should consult your doctor. Let's look at a few recipes:
- Camomile tea. Pour 1 tablespoon of chamomile into a glass of boiling water and let it brew for an hour. Take half a glass of the chilled drink before bed.
- Motherwort infusion. Pour 1 tablespoon of herb into 2 cups of boiling water and leave for an hour. Drink chilled, three times a day, half an hour before meals. Decoctions of lemon balm and valerian have a similar effect.
To prevent relapse of the disease, as well as to more quickly and maximize the effect of conservative therapy, it is necessary to adjust your lifestyle, and folk remedies for the treatment of prolactinoma have mainly additional functions. It is important for such patients to get a good night's sleep, eliminate stressful situations, and it is useful to introduce physical activity into their daily routine. This could be swimming, aerobics, yoga - sports that do not require excessive stress and have a relaxing effect.
In women suffering from hyperprolactinemia, the positive effect of the treatment is manifested in the form of restoration of normal levels of sex hormones, menstrual cycle and reproductive function. The sooner a patient with suspected hyperprolactinemia consults a specialist, the higher her chances of a complete cure. Lifestyle with prolactinoma has some restrictions.
How to treat hyperprolactinemia? Treatment of such a pathological condition as galactorrhea-amenorrhea syndrome is carried out with the help of drug therapy. The doctor who treats this pathology is an endocrinologist. But observation by a gynecologist is also necessary.
The most effective remedy in the fight against this disease is parlodel. It is prescribed both in the presence of pituitary adenoma and in its absence in hyperprolactinemia. In any case, treatment with this remedy is effective. Parlodel is aimed at inhibiting the growth of prolactin and preventing its entry into the bloodstream, as well as inhibiting the processes of its synthesis.
Parlodel for galactorrhea-amenorrhea syndrome normalizes the secretion of prolactin. And this in turn gives the following consequences:
- restoration of activity of the sexual centers of the hypothalamus;
- an increase in the production of gonadotropic hormones several times;
- normalization of the menstrual cycle;
- restoration of reproductive function.
The effectiveness of this drug in the fight against illness has been confirmed by many examples of recovery. To treat a severe form of the disease, an additional drug may be added to Parlodel.
Usually the drug is prescribed in the following dosage: 2.5 – 5 mg per day. In case of severe condition of the patient, the dose may be increased to 10–20 mg.
The drug is usually not prescribed to pregnant women. But during pregnancy and lactation, prolactin synthesis increases several times. This fact forced doctors to reconsider their decision to take the drug.
If a woman was treated with Parlodel before pregnancy, the tumor did not grow. But if it is discontinued, a relapse of the disease may occur. This once again confirms the need to take the drug for pregnant women with galactorrhea-amenorrhea syndrome. Moreover, it has no effect on the fetus, and children born to women taking Parlodel are absolutely healthy.
If the disease is caused by macro- and microprolactinomas that are resistant to parlodel, surgical intervention will be required. If a woman is not planning a pregnancy, she can take her time with the operation and monitor the course of the disease. Surgery will only be required if the tumor is clearly growing. Radiation therapy, which was previously often prescribed for the treatment of galactorrhea-amenorrhea syndrome, does not guarantee complete recovery.
Treatment with Parlodel may not give a positive result if the patient has severe hyperprolactinemia and very low concentrations of gonadotropic hormones and estrogens in the blood. To treat such patients, the drug clostilbegit is used, which stimulates the release of FSH and LH into the blood. Also effective is the introduction of gonadotropic hormones into the blood, which contain FSH and LH in a 1:1 ratio.
With proper and timely treatment of galactorrhea-amenorrhea syndrome, the patient has a good chance of a healthy life and preservation of reproductive function.
Hyperprolactinemia syndrome is a hormonal disease that can affect both female and male bodies. In women, the level of prolactin in the blood changes much more often. This is due to changes in hormonal levels during menstruation, pregnancy or breastfeeding a newborn baby. In fact, prolactin is a sex hormone, so successful conception, a favorable course of pregnancy, childbirth and breastfeeding of a newborn depend on it.
During pregnancy, in many women the amount of prolactin in the blood exceeds medical indicators. Doctors call this the physiological norm. An increase in the concentration of this hormone occurs from the 2nd to the 6th months of pregnancy. Then the level of prolactin decreases somewhat, and the new levels are maintained until childbirth.
There are cases when, against the background of pathology of the pituitary gland (for example, the development of an adenoma in this gland), the amount of prolactin remains high. This leads to an unfavorable course of pregnancy in the later stages. The task of medical specialists in such a situation is to identify the reasons for the increased concentration of lactation hormone and adequate treatment (which will help stabilize the condition of the expectant mother).
It should be noted that drug therapy at high concentrations of prolactin in the blood of a pregnant woman is contraindicated. Hormonal medications cannot be taken, because they will cause a malfunction of the hormonal system, and the consequence of this will be spontaneous termination of pregnancy. If the cause of the pathology is a pituitary adenoma, therapy using antitumor drugs is also prohibited.
Medicines against tumors are highly toxic, so taking them during pregnancy often leads to disruption of the baby’s intrauterine development. The only way out that will help reduce prolactin is folk medicines with a general strengthening and sedative effect, which are used for symptomatic therapy.
Treatment of hyperprolactinemia with folk remedies is well suited for those whose increase in prolactin is not associated with a somatic disease and occurs due to stress or physical overload. The main herbs that are used for this pathology are sage and elecampane. An effective course of herbal medicine made from several herbs is also common: motherwort, peony root, hops, adonis, mint, and mother liquor.
Hyperprolactinemia and pregnancy are concepts that are interconnected. After conceiving a child, the level of the hormone prolactin increases, and as a result hyperprolactinemia develops. The pathology, in which the activity of eggs is suppressed and sexual desire is significantly reduced, occurs due to the “blocking” of the production of progesterone (pregnancy hormone). An unfavorable situation develops due to excess prolactin in the body and is often accompanied by the following symptoms:
- there is insufficiency of the 2nd menstrual phase;
- no ovulation;
- The endometrium (uterine lining) grows very slowly, so problems arise with conceiving a baby and bearing a fetus.
Prevention
In order to avoid the development of elevated prolactin levels, several basic rules should be followed, which are mainly used to eliminate provoking factors.
Among them:
- Maintaining a healthy lifestyle, monitoring proper nutrition, including physical activity.
- Eliminate bad habits from your diet.
- Eliminating the possible impact of stressful situations, as well as emotional stress.
- Regularly visit a specialist, in particular a gynecologist, to monitor the condition of the reproductive system.
- If pathological conditions are identified, treat them in a timely manner.
- It is these rules that will prevent the development of complications and the possible appearance of signs of increased prolactin in the blood.
It is based on all of the above that you should regularly visit specialists and not self-medicate.
There is no specific prevention of hyperprolactinemia, since it can be caused by various factors and diseases. Measures to prevent it consist of prevention, timely identification and elimination of the cause.
Nonspecific preventive measures are general health measures:
- rejection of bad habits;
- balanced diet;
- regular physical activity;
- avoiding excessive physical and mental stress;
- normalization of sexual life, prevention of artificial termination of pregnancy, effective contraception;
- regular preventive examinations.
Prolactin: functions not related to fertility
Prolactin and the immune system.
- Prolactin promotes the growth, differentiation, and survival of lymphocytes. But its deviation from the physiological norm in the blood plasma leads to a decrease in the immune response.
- Enhances the formation of immunoactive substances M and G.
- Affects the increase in the formation of interferon gamma.
- After organ transplantation, an increase in prolactin concentration is an early sign of graft failure.