An infection caused by chlamydia can affect not only the genitourinary system of women, but also quickly spread to other organ systems. The main danger of this disease is that it is often present in a latent state, but despite the absence of obvious signs, it causes pathological changes in organs.
Both middle-aged people and teenagers are susceptible to infection. It is extremely difficult to determine it based only on symptoms and external manifestations, because chlamydia does not cause a specific clinical picture, resembling many other inflammatory processes of the genitourinary system.
Pathogen
Experts have only recently decided what type of microorganism the causative agent of chlamydia belongs to. The bacterium of the genus Chlamydia - Chlamydia trachomatis - exists in the body in two different forms, one of which more closely resembles bacteria, and the second behaves like a virus:
- Intracellular form . This period of the bacterium’s life takes place inside the host cells, where it actively consumes cellular energy and spends it on rapid growth and reproduction (division). Inside the cell, chlamydia divides at high speed, sometimes entire colonies are formed. Despite the active growing season, the bacterium at this stage is practically incapable of infection.
- Extracellular form . All vital processes after leaving the cell slow down and almost completely stop, but virulence (the ability to infect) at this stage becomes maximum.
There is another rare form when the bacterium lives inside the cells, but the processes of growth and reproduction do not occur. At this stage, chlamydia is almost impossible to detect using standard clinical tests, in addition, this form is very resistant to most drugs.
The entire life cycle of one chlamydia lasts about 2-3 days, so the likelihood of infection occurs very often - once every few days.
In the international classification system of diseases, chlamydia is included in the broad group “Diseases caused by chlamydia” with code A74.
Routes of infection
How the disease will develop largely depends on the route through which the infection entered the woman’s body.
The main routes of infection with chlamydia:
- Sexual path. This method of infection is the main one, and the vast majority of transmissions occur through this mechanism. If sexual intercourse occurs without using a condom, the likelihood of infection increases many times over. The pathogen enters the cylindrical epithelium of the external genitalia or the vagina and penetrates through the membranes deep into the cells. In addition, the infection easily penetrates the body during oral or anal sex.
- Contact and household path. A rather rare route of transmission, but it cannot be completely excluded. Chlamydia retains the ability to infect for 2 days at a temperature of about 20°C, so the disease can spread from dirty hands, toilet lids or handrails in public transport, from towels or bathrobes.
- During pregnancy from mother to child. Such transmission occurs during intrauterine development, when the fetal fluid becomes infected with chlamydia. If a child swallows them, there is a high probability that infection will occur. In addition, bacteria can enter his body through unformed thin skin.
- Airborne path. A very rare method that is observed only in the pulmonary form of chlamydia.
After the successful introduction of infection, only a part of the sick women may notice symptoms in themselves, the rest will not be aware of the presence of the disease in the body.
Reasons for the prevalence of chlamydia
Chlamydia is characterized by an asymptomatic or mild course and high contagiousness. After one unprotected sexual intercourse, the risk of infection for women is 35-50%, for men 50-75%. However, not everyone gets sick, but only a quarter of those infected. About half develop chlamydia carriage; people with good immunity remain in good health. As a result, we get a figure according to which about 1/2 of the world's population either suffers from chlamydia or are carriers - hidden spreaders of the infection.
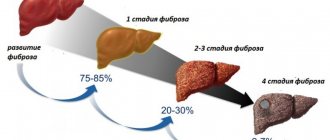
Mild symptoms and disguised manifestations as other ailments also contribute to the prevalence of chlamydia. Chlamydia – causes inflammation of the joints (arthritis), conjunctivitis and pneumonia; chlamydial prostatitis accounts for about 50% of all diagnosed inflammations of the prostate gland.
Up to 85% of identified chlamydia is combined with other sexually transmitted infections (gonorrhea, syphilis, trichomoniasis, ureaplasmosis and mycoplasmosis).
Combined diseases are more difficult to treat and are less tolerated by patients: higher intoxication, more often complications in the form of infertility and purulent processes in the genitourinary system.
The route of infection with chlamydia is predominantly sexual , through genital or anal contact; the infection is also transmitted orally. In children, infection is possible during childbirth from a sick mother or through contact and household contact - through dirty hands, common hygiene items, dishes and towels. The pathogen survives in the external environment for up to 48 hours under conditions of normal or high humidity and temperatures up to 19 degrees. The incubation period averages 14-30 days; in patients with HIV, cases of acute onset of the disease are known, within 24 hours after sexual contact with an infected partner.
Symptoms of chlamydia in women
The duration of the incubation period varies from woman to woman depending on the state of health and lasts a maximum of a month. The development of infection occurs in three stages:
- Bacteria secrete special substances that destroy cell membranes and help penetrate its structure. At the same time, the cell continues to live and supply chlamydia with all the necessary nutrients. The body reacts to such penetration by increasing the release of leukocytes.
- After sufficient reproduction of chlamydia, the cell dies and chlamydia begins to migrate through the intercellular space. In response to this, the immune system is activated and begins to fight.
- In an organ in which numerous cell damage has been observed, an inflammatory process occurs, and new bacteria settle in other cells.
The development of the process can be acute with pronounced symptoms, or it can occur in the form of a chronic course.
Acute stage
In acute cases, all symptoms resemble manifestations of many urogenital infections, so they must be considered in combination:
- At first, your body temperature may rise. Usually it does not exceed readings above 37.5 ° C, and after a week it can drop to normal limits. The general condition is reminiscent of the onset of a viral infection: weakness, fatigue and general loss of strength appear.
- Pain is observed in the genital area, abdomen and lower lumbar region. They vary in strength, from minor to severe.
- Urinary disorders. The urge to go to the toilet often becomes more frequent, and the volume of urine decreases noticeably. In this case, the outflow of urine occurs painfully, especially at the beginning and end of the process. A painful burning and stinging sensation is felt in the urethra.
- Changed selections. Usually their volume increases, their consistency is close to greenish or yellowish mucus with a pungent odor. In the case of a fishy odor, a parallel development of bacterial vaginosis can be assumed.
- Burning, swelling and severe discomfort of the external genitalia. This symptom is observed in women whose body exhibits an allergic reaction to the presence of a pathogenic microbe on the genital mucosa.
If treatment is not started, then after a while the symptoms will subside and disappear. But since an independent cure for chlamydia is impossible, the disappearance of symptoms means that the disease has passed from an acute form to a chronic one.
Chronic course
In a chronic course, all the symptoms that arise in the acute phase will recur every time the body’s defenses weaken. This can occur after serious illnesses, operations, periods of severe physical or mental fatigue, hypovitaminosis, etc.
In addition to the general ones, the following symptoms often develop:
- Erosion and swelling on the surface of the cervical epithelium. This symptom can only be detected by a doctor during a gynecological examination. There will also be a noticeable scanty bloody discharge from the erosion, where chlamydia is actively multiplying.
- After sexual intercourse, slight bleeding is observed. With the mechanical impact of the penis on the cervix, erosions are damaged and bleed for some time.
- Menstruation may be more painful than before the onset of the disease. The timing of the monthly cycle sometimes shifts due to delays.
The prolonged presence of infection in the body can promote the movement of bacteria up the genital or urinary tract and cause the following disorders:
- Endometritis is an inflammatory process of the inner mucous layer of the uterus.
- Salpingo-oophoritis is inflammation of the fallopian tubes or ovaries, sometimes present simultaneously.
- Colpitis is an inflammation of the glands located at the base of the vagina (preputial glands). It manifests itself most acutely with a lack of estrogen: during pregnancy, in girls during puberty, during menopause.
- Cervicitis is a lesion of the cervical canal, which increases due to swelling and inflammation. In its advanced form, it leads to local desquamation of the epithelium.
In addition, the chronic form contributes to frequent colds, which take a long time to treat and are fraught with complications.
Treatment of chlamydia
Treatment is aimed at destroying the pathogen, eliminating inflammation, preventing and combating complications of chlamydia. The first number is a treatment regimen with antibiotics that are able to penetrate the cell membrane. The drugs of choice are tablets for chlamydia, antibiotics azithromycin and doxycycline.
- Azithromycin is prescribed to adults (including pregnant women) once, 2 tablets (1 g). The dosage for children is specially calculated, but the antibiotic can only be used with a body weight of at least 10 kg. On the first day, take 10 mg/kg, then 5 mg/kg, the total course is 5 days. For a three-day course, a single dosage is 10 mg/kg, total dosage is 30 mg/kg.
- Doxycycline is absolutely contraindicated during pregnancy; it is prescribed to children from the age of 8 or with a body weight of more than 50 kg. Daily dosage for children: 1 day 4 mg/kg, then 2-4 mg/kg, course from 10 days to two weeks. Adults are prescribed 200 mg on the first day, then 100 mg per day, course 10-14 days. Doxycycline has an irritating effect on the mucous membrane of the digestive tract, so it is recommended to take the tablets after meals and drink plenty of water.
Antifungal medications will help prevent or treat candidiasis that may develop after a course of antibiotic treatment. Fluconazole is used, usually in capsule or syrup form. Mucosal candidiasis is treated with dosages of 50-100 mg/day, vaginal candidiasis 150 mg/day. Treatment can be long, up to 30 days, with an average of 1 to two weeks.
Local remedies are used to destroy infections in the urethra, cervix, conjunctivitis and stomatitis. Protargol is used: 1-5% solution for lubricating the oral mucosa and the external opening of the cervical canal, for instillation into the urethra 1-3%, for chlamydial conjunctivitis - eye drops with protargol. Hexicon vaginal suppositories, 1 x 2 per day, course from 7 to 20 days. They are also used to prevent chlamydia within 2 hours after unprotected intercourse.
Immunomodulators – aloe, cycloferon (injections); echinacea, lycopid – oral medications. Strengthen the immune response, reduce treatment time.
Proteolytic enzymes, preferably of plant origin (papain, bromelain), are taken 1-1.5 hours after meals. The goal is the prevention of adhesions after chlamydia, anti-inflammatory effect. Karsil and lecithin will help restore liver cells. Preparations with lactobacilli, including vaginal suppositories, normalize the microflora of the vagina and small intestine.
Traditional treatment as a mono-method is absolutely unacceptable. After a basic course of antibiotics, you can use horsetail and juniper tea, which will have a diuretic and disinfectant effect. This cannot be done while taking antibiotics: due to the diuretic effect, the concentration of drugs in the body will become insufficient, and the load on the kidneys will increase.
Treatment of chlamydia is necessary for everyone who has had sexual contact with a sick or infected person. Efficiency control: repeat PCR 6-8 weeks after the end of treatment. Upon recovery, the PCR test is negative.
Chlamydia in women during pregnancy
This disease belongs to TORCH infections, as it can have a negative impact on the course of pregnancy.
The main perinatal complications of chlamydia:
- threat of miscarriage;
- infection of the amniotic sac and polyhydramnios;
- development of pyelonephritis in a pregnant woman;
- Reiter's syndrome;
- urethral stricture, causing stagnation of urine in a pregnant woman;
- prolonged contraction of the uterus after childbirth.
The consequences of chlamydia for the embryo are determined by the moment when the infection occurred. If the disease begins in the first trimester, then there is a high probability of fetal death, and if the pathology appears later, the child may experience deviations in formation and development.
Children born to infected women may be underdeveloped, anemic or severely underweight, and their central nervous system is often affected. In the first months of life, such children often develop bacterial infections in the eyes, ears, throat, and encephalitis or pneumonia occurs. It is rare for a child to die suddenly.
When to see a doctor
A gynecologist diagnoses and treats chlamydia in women. Considering the source of the disease and the patient’s condition, additional consultation with other specialized specialists (venereologist, dermatovenereologist, ophthalmologist, infectious disease specialist, arthrologist, urologist, therapist, immunologist) may be necessary.
It is important to consult a doctor when the first signs appear that indicate the presence of an inflammatory process. The specialist will prescribe a diagnosis and select treatment, taking into account the information received.
Diagnostics
Chlamydia can be accurately diagnosed only through laboratory tests.
For diagnosis, women are most often prescribed the following tests:
- Smear for bacterioscopy . This test is performed by a gynecologist. Smears are taken from three places at once: from the vagina, cervical canal and urethra. Chlamydia may be detected in all smears, or may be present in only one. After selection, the material is stained with microbiological dyes and examined under a microscope. The method is attractive for its painlessness and speed, but is characterized by low reliability.
- Research using the ELISA method . To do this, take blood from the cubital vein or vaginal discharge. The analysis is based on the detection of antibodies, which can be used to determine not only the presence of bacteria, but also the type of process (acute or chronic).
- Bacteriological inoculation in a Petri dish on agar (nutrient medium). After sowing, the sample is kept in a thermostat at the ideal temperature for the development of bacterial colonies, and then their species composition is studied. The technique is accurate and reliable, but requires a lot of time to obtain results.
- PCR examination . Fragments of DNA or RNA of the causative bacterium are found in biomaterial taken from the external or internal genital organs, as well as in blood serum. This method is capable of detecting chlamydia both at the stage of intracellular development and after leaving the cell structure.
For effective diagnosis, the doctor orders several types of tests at the same time, since chlamydia may be present in only one type of sample and absent in others.
Possible complications
The inflammatory process due to chlamydia entails serious consequences if you do not go to the hospital in a timely manner:
| Name | Description |
| Endometritis | The mucous membrane in the uterine area becomes inflamed. There is no pregnancy because the fertilized egg cannot implant in the uterus. The risk of spontaneous abortion after conception also increases. |
| Endocervicitis | Pathological processes affect the cervix. The disease increases the chances of malignant changes. |
| Salpingitis | The inflammatory process affects the fallopian tubes or uterine appendages. For a woman, this pathological condition is dangerous due to infertility. Scar tissue forms in the lumen of the fallopian tubes, which forms adhesions and leads to obstruction of the organ. |
| Reiter's syndrome | The disease is characterized by a complex of symptoms that occur against the background of various diseases. Pathological processes affect the joints, cervix, and urethra. |
| Hemorrhagic cystitis | Pathology occurs as a result of damage to the walls of the bladder by pathogenic microflora. |
Infertility and various inflammatory diseases of the pelvic organs are also complications of chlamydia. The same goes for blocked fallopian tubes, chronic pain and inflammation in the liver. Advanced forms of the disease provoke not only infertility, but also the development of malignant processes.
The prognosis for a woman infected with chlamydia is favorable if she consults a gynecologist in a timely manner. She underwent adequate therapy, which was selected for her by a specialist based on the results after diagnosis. Otherwise, pathological processes will progress, as indicated by characteristic symptoms. The risk of serious complications increases.
Article design: Vladimir the Great