A little about vulvovaginitis
This article will discuss inflammation of the vulva and vagina in children, common causes that contribute to inflammation, diagnosis and treatment.
The disease is considered harmless and occurs, as I already said, more often in children of preschool age.
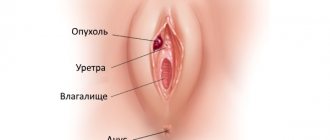
Vaginitis is an inflammation of the vagina, vulvitis is an inflammation of the vulva or external genitalia, that is, the perineum, labia majora and minora. Since these areas are nearby, the disease often occurs together, which is why the name “vulvovaginitis” exists.
Hormonal ointments
Why does vulvitis bother girls so often? In a nutshell, the functioning of the mucous membrane of the genital organs is ensured by female hormones - estrogens. They begin to be secreted in sufficient quantities by the ovaries only after the onset of regular menstruation. Until this age, the child’s perineum is exposed to various infections, irritation with washing products, sweat, etc.
Pediatric gynecologists note that almost 50% of girls under the age of 2 have synechiae, fusion of the labia minora. In most cases, this type of vulvitis goes away on its own. This disease requires treatment only if the fusion interferes with the normal flow of urine. For this purpose, an ointment containing estrogen is used.
Features of the disease
The genitals of newborns are sterile. Then certain microorganisms begin to develop on the tissues. The vaginal environment is slightly alkaline or has a neutral pH.
It does not contain lactobacilli. They appear closer to puberty. As the body grows, the environment becomes oxidized. With the advent of menstruation, it becomes similar to the microflora of sexually mature women.
Hormonal changes begin after 2 years. As girls age, they are less susceptible to the disease. In adult women, this pathology is rare.
Vulvitis is an inflammation of the mucous surface of the external female genital organs. It spreads to the labia, vaginal area, and clitoris. Sometimes the redness spreads to the anal area, pubis, and inner thighs of the girl.
In children, this disorder is common and is caused by various reasons. It is important for parents to understand that vulvitis is possible even in newborns. Many people mistake redness and swelling of the mucous membrane for ordinary diaper rash, trying to cope with the problem with creams and powders without consulting a doctor. This can aggravate the situation, and the disease becomes chronic.
Little girls are unable to complain about what is bothering them, expressing dissatisfaction by worrying and crying. Those who are older may be embarrassed to tell their parents about the problem that is tormenting them. Therefore, timely detection of vulvitis in children depends entirely on the vigilance of adult family members.
If this disease is not treated, it easily becomes chronic, periodically making itself felt. During puberty, vulvitis can cause developmental disorders of the genital organs and disruptions in the reproductive system.
Vulvitis can first develop in infancy, up to one year. However, more often it occurs between one and eight years of age. Later, when a girl begins to mature, the microflora of her vagina changes and becomes less vulnerable to vulvitis. However, other provoking factors appear: improper use of pads, wearing beautiful but uncomfortable synthetic underwear, early onset of sexual activity.
Reference! According to ICD-10, vulvitis is numbered 76.3 and 76.4.
Healing
Another group of ointments used for vulvitis are healing ones. They are used after acute symptoms of the disease have been relieved. Healing medications can relieve inflammation and irritation and regenerate damaged tissue. Medicines in this group include:
Actovegin. This ointment is prepared based on the blood of cattle. Gynecologists prescribe the drug to patients who have problems with the acid-base balance of the vagina, which occurs with vulvitis. The medicine accelerates the process of tissue restoration and improves their nutrition at the cellular level.
Any healing ointment is used for 3-4 weeks, until the soft tissues of the external genitalia are completely restored after the disease. It is important to follow the rules of personal hygiene and doctor’s recommendations.
Patients need to understand that ointments are effective only in the initial stages of the disease. If vulvitis caused by fungi or bacteria is advanced, then along with external agents it is necessary to take antibiotics and antimycotics orally. Any treatment must be carried out under the supervision of a physician.
«>
Manifestations of vulvovaginitis
Vulvovaginitis in a child always manifests itself as complaints or, scientifically, a clinical picture. The girl complains to her mother about itching, pain, burning and unpleasant sensations - “pinching there” (in the genital area).
And the mother says that the child often pulls his hands to “that very place”, some kind of discharge (leucorrhoea, cheesy, green) appeared on the panties, and the skin became bright red or pink, rashes or even scratches appeared.
There are no other manifestations, such as a violation of the general condition, loss of appetite, pain in the abdomen or lower abdomen; they can only appear when inflammation spreads to other organs and tissues.
Then the question arises, where does it come from, this vaginitis, in a small child.
Clinical picture
Primary vulvitis in children occurs without fever and deterioration in general condition. Such signs are observed only in the presence of any concomitant infection. To identify the disease in the early stages, doctors recommend that parents conduct an independent examination of the perineum. Let us list the symptoms of the development of vulvitis in girls:
- hyperemia of the external organs of the reproductive system;
- Possible scratching and small sores;
- severe discomfort, unbearable feeling of burning, itching;
- swelling of the labia and mucous membrane around the entrance to the genital opening;
- pain when walking and any movements, urination, washing, wiping after using the toilet;
- white or grayish coating;
- Sometimes mucopurulent discharge from the vagina is noted, this may indicate further spread of the infectious process.
In children at the initial stage, the symptoms of the disease are mild. However, the child loses his usual peace: he becomes tearful, irritable, and inexplicably restless. The period of sleep worsens and shortens, crying appears when urinating. Depending on the severity of the symptoms of vulvitis in children, the following forms are distinguished:
- acute, lasts up to a month, occurs with a pronounced clinical picture;
- subacute, lasts up to three months, signs of the disease are blurred;
- chronic is observed for a long time, the manifestations are recurrent in nature and are noted when exposed to any allergen or infection.
It should be mentioned that mothers can independently predict vulvitis in girls. Currently, on any specialized forum you can find a photo of what the perineum looks like with developing inflammation. But if a child becomes restless, complains of discomfort in the genital area or puts his hands there, you should consult a doctor. The fact is that the infection can spread quickly, which entails more complex treatment.
Main reasons
It is wrong to assume that a child is protected from problems in the reproductive system. The disease can occur even in infants, but is still more often observed among patients 1-9 years old. Pathology also occurs in adolescents.
The most common causes are various types of infections. Childhood vulvitis can be caused by:
- viruses;
- fungi;
- protozoan microorganisms;
- gonococci;
- chlamydia and others.
Respiratory diseases - acute respiratory infections, sore throat, tonsillitis and others - can provoke the development of pathology. The infectious form of the disease can develop due to pathogenic microflora, which often occurs with weak immunity.
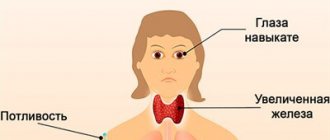
Hormonal disruptions and ovarian pathology can also provoke pathology.
Often inflammation develops due to helminthic infestation, as well as when various objects (grass, sand, insects) enter the genitals.
The fungal form of pathology can develop against the background of:
- use of antibiotics;
- endocrine disorders, in particular with diabetes mellitus;
- weak immunity.
If you are allergic to irritants - soap, foam, creams, powders - the atopic form develops.
Sometimes tissue damage occurs due to frequent washing, as a result of using too thick underwear, or the wrong choice of diapers.
Also, vulvitis in children can occur due to abnormal development of the genitals:
- in the absence of posterior commissure;
- with pathology of the development of the external genital organs;
- low location of the urethral opening.
Routes of infection
Infection can occur in different ways:
- Vulvitis in an infant can develop as a result of infection during passage through the birth canal.
- In young girls, infection most often occurs as a result of violation of hygiene rules (domestic route).
- In adolescents, infection can occur through sexual experience.
There are several types of pathology:
- primary - occurs as an independent disease;
- secondary – develops against the background of some pathology, when the infection comes from other foci (tonsillitis, caries, sore throat, acute respiratory infections and others).
As you can see, there are many options, which is why the disease is quite common.
Measures to prevent vulvitis in girls and young women
Let's talk about how to treat vulvitis in a girl. The main thing in the treatment of vulvitis in children is to eliminate inflammation and suppress the cause of this inflammation.
The therapy is complex and includes:
- anti-inflammatory baths with the addition of decoctions of chamomile, calendula, St. John's wort. To do this, pour 1 - 2 tablespoons of dry grass with 1 liter of boiling water, infuse, cool, express and perform sitz baths for 3 - 5 minutes;
- washing the external genitalia with antiseptic solutions (Furacilin, Miramistin);
- symptomatic therapy aimed at eliminating itching and burning (antihistamines, anti-inflammatory ointments);
- in the case of bacterial vulvitis, antibacterial drugs are prescribed. If vulvitis is of a fungal nature, then antifungal drugs (Itraconazole, Fluconazole or topically Pimafucin cream, Clotrimazole). If the cause of Trichomonas is Metronidazole, Tinidazole. If vulvitis has developed as a result of a foreign body, then it is removed, and for helminthic vulvitis, accordingly, antihelminthic therapy is carried out;
- for allergic vulvitis, limit the consumption of foods that cause allergies (citrus fruits, sweets, chocolate).
In addition, the complex treatment of vulvitis must include:
- multivitamins (synthetic) or products enriched with vitamins;
- preparations containing lactobacilli (Linex, Bifiform) to restore vaginal microflora;
- increasing the body’s immune forces (walking in the fresh air, physical exercise).
Linex
Linex is a drug containing live strains of lactobacilli, easy to use in children over 1 year of age. Available in the form of capsules and powder.
100 grams of powder contains at least 1*10*8 CFU. But it should be noted that the drug is widely prescribed by pediatricians and in infancy.
Newborns and children under 7 years old are prescribed 1 sachet per day, children over 7 years old - 2 sachets per day, possibly in one dose. The duration of therapy is 30 days, the course is repeated if necessary.
The drug is freely available in pharmacies without a doctor's prescription. The price of the drug ranges from 400 to 600 rubles per package.
Bifiform
Bifiform (baby, toddler, complex) is a complex probiotic that has various release forms for different age categories - from newborns to adults.
- Bifiform baby is available in the form of a suspension (1 dose once a day for 20 - 21 days).
- Bifiform baby (release form - sachet). It is prescribed for children from 1 to 3 years old, 1 sachet 2-3 times a day, over 3 years old - 2 sachets 2-3 times a day.
The drug can be freely purchased in city pharmacies, without a doctor’s prescription. Its price is, on average, 350 rubles per package.
Bifidumbacterin Forte is a 4th generation probiotic. One dose of the drug contains at least 1*10*7 CFU. The release form of the drug is powder. Children under 6 months of age are prescribed 2.5 doses 2 - 6 times a day, children aged 6 months to 3 years 5 doses 1 - 2 times a day, children over 3 years old 10 doses 1 - 2 times a day. day. The course of taking the drug is 2-3 weeks, repeated 2-3 times a year.
The drug is dispensed without a doctor's prescription. The price is about 130 rubles for 10 pieces.
Currently, there is a huge amount of information for young parents on how to properly carry out hygiene for newborns and older girls.
Yes, yes, you understood correctly, baby hygiene comes first! The girl needs to be washed properly with warm running water after each bowel movement and before bedtime! Water procedures after each trip to the toilet completely wash away the entire microflora of the vagina, making it sterile, and therefore defenseless against pathogenic flora.
It is necessary to wash from top to bottom, that is, in the direction from the vulva, perineum to the anus. Use toilet soap no more than 2 times a week. In addition, girls should have separate hygiene items (towel, washcloth).
You can also reduce the risk of developing vulvitis in girls and young women if you stop wearing synthetic and tight-fitting underwear, promptly change sanitary pads, diapers and diapers as they become dirty or every 4 hours.
In addition, a balanced and nutritious diet for children, prevention and timely treatment of concomitant and chronic diseases, as well as vitamin supplementation are of great importance in preventing the development of inflammation of the external genital organs, and not only.
I would like to repeat the words of the famous adult obstetrician-gynecologist V.E. Radzinsky: “We treat a woman, not an analysis!” In our case, a girl.
So, you should not treat the so-called vaginitis in a girl if she has no clinical manifestations of the disease, and in the analysis, which was taken just for show, a lot of leukocytes and other sundry things were suddenly discovered.
Have pity on the child, you start stuffing him with everything you can, just to cure the analysis, but in fact there is a human factor. For example, the laboratory assistant who was doing the analysis sneezed nearby or took a not entirely clean glass slide.
Well, now to the treatment of vulvovaginitis!
Treatment for vaginitis depends on the cause that caused it. If it is a helminthic infestation, then antihelminthic therapy (Pyrantel, Vermox) is prescribed.
If there is severe unbearable itching in the perineal area, sedatives and antihistamines (Tavegil, Diazolin) are prescribed. If, during a laboratory examination, yeast-like fungi Candida are detected in a smear analysis, antifungal drugs are prescribed in the form of ointments and creams (Nystatin).
For viral vulvovaginitis, treatment is carried out with antiviral drugs to destroy the viruses that cause the disease. In such cases, Acyclovir is more often prescribed.
There is such a thing as specific vulvovaginitis, that is, vaginitis caused by pathogenic microorganisms (gonococci, trichomonas, chlamydia). This disease requires the prescription of antibiotics (Ampicillin or Cephalexime); it is possible to prescribe vaginal sticks and ointments (Levomekol, Furazolidone).
Vulvitis is a dangerous disease that can lead to dire consequences. If you notice the first signs, you should immediately consult a doctor. Otherwise, the pathology can become chronic and cause a number of complications.
How to treat vulvitis in girls? It is worth noting that treating the patient yourself is strictly prohibited. In many cases, outpatient treatment is necessary. Treatment at home is possible if the disease is mild, but only under the supervision of a doctor.
Treatment of any form of pathology (chronic, acute vulvitis, subacute vulvitis) is carried out comprehensively. In many situations, bed rest is prescribed. The choice of certain measures directly depends on the reason that caused the problem.
Treatment includes a set of measures:
- Nutrition correction. In acute cases, it is necessary to change the diet. It is necessary to reduce the intake of foods that contribute to the formation of acids (fried, fatty, smoked, sour foods). The diet should consist of alkalizing foods: milk, boiled, fresh vegetables. If the pathology has developed as a result of an allergy, it is necessary to exclude eggs, citrus fruits, honey, and chocolate. At the end of the acute period, you can gradually add fermented milk products to the menu.
- Local treatment. The therapy is designed to remove swelling, hyperemia of the genital organs, and alleviate the patient’s condition. Disinfectants are used in the form of ointments, baths, and herbal infusions.
- Systemic therapy. Drug treatment is prescribed taking into account the type of pathogen. For each of them there is a specific drug.
- Normalization of the patient's condition. To relieve unpleasant symptoms, desensitizing agents, drugs to normalize digestion, immunomodulators, vitamin complexes and others are used.
Treatment of candidiasis (infection of the genital organs with fungi) is carried out with oral and local antifungal agents. For specific forms of pathology, it is necessary to take antibacterial drugs. For allergic forms, antihistamines are prescribed. Antihistamines are also prescribed for severe itching and swelling to alleviate the condition.
Treatment of patients over 4 years of age must be carried out very carefully, without embarrassing them. You cannot use ointments or decoctions of medicinal herbs on your own. All actions must be coordinated with specialists. Dry yourself with a towel very carefully, without irritating the skin. You can blot your genitals with a napkin, then apply ointment.
The disease is detected by a pediatric specialist. Further diagnosis and therapy is carried out by a pediatric gynecologist. The doctor reviews your medical history, performs a physical examination, and orders additional tests. The child may undergo: vulvoscopy, vaginoscopy, polymerase chain reaction of scraping, bacterial culture of vaginal discharge, OAM, UAC, bacterial urine culture, coprogram and allergen-specific IgE blood test. After identifying the cause of the disease, consultations with an endocrinologist, allergist and gastroenterologist are possible.
The main goal of therapy is to get rid of the cause that caused the formation of the disease. Symptomatic treatment is also carried out, which includes: herbal baths, treating the genitals with antiseptic agents, sanitizing the vagina, treating affected areas with anti-inflammatory ointments, applying pharmaceutical suppositories, as well as taking sedatives and antihistamines.
Depending on the cause of the disease, antibiotics, antimycotic and antiviral drugs are prescribed. Additionally, they strengthen local immunity with multivitamin complexes, immunomodulators and eubiotics.
Principles of drug therapy
In most cases, topical application is sufficient to treat vulvitis in girls. For physiological reasons, suppositories are not used in young children. The doctor prescribes baths, ointment applications and lotions with antiseptic solutions. Depending on the cause, treatment of vulvitis in girls is carried out with the following medications:
- Levomekol ointment contains the antibacterial component chloramphenicol, effective against staphylococci, Escherichia coli, and methyluracil, which accelerates tissue regeneration processes;
- Sintomycin liniment has a similar effect to Levomekol due to the same composition (with the exception of methyluracil);
- Sangviritin solution has a bacteriostatic effect and can be used in parallel with ointments;
- Citeal, the drug contains chlorhexidine, hexamidine and chlorocresol, due to this the product has a bactericidal and fungicidal effect, and also has an antipruritic effect. Used instead of soap for washing. When used in small children, it must first be diluted with water in a concentration of 1:10. After use, the solution should be washed off.
- A solution with Miramistin is prescribed when trichomonas, gonococci and chlamydia are detected; the drug also fights fungal pathogenic flora;
- Pimafucin ointment is used to treat vulvitis in children caused by candidiasis;
- Citeal.
It is necessary to emphasize that when identifying specific pathogens, the use of antibiotics is necessary. Children are prescribed a suspension of Augmentin in a daily dosage of 40 mg/kg, divided into three doses, for 5–10 days. For persistent infection, Azithromycin (Sumamed) in the same release form is indicated.
For non-bacterial childhood vulvitis, accompanied by fusion of the labia, Ovestin ointment with estrogen is prescribed. It is used 1 – 2 times a day for 3 – 4 weeks. If an allergic reaction develops, hydrocortisone ointment is prescribed. It effectively eliminates itching and other symptoms of inflammation.
Symptoms
The symptoms of vulvitis in girls are very similar to the signs of other sexually transmitted infections:
- Itching, pain, burning in the genital area.
- Swelling, redness of the mucous membrane, clitoris, lips.
- The tissue may become covered with erosions and ulcers.
Unpleasant sensations increase when walking or visiting the toilet. The pathology is often accompanied by vaginal discharge. By intensity, color and smell, you can determine the form of the disease and the cause that provoked it.
Most often, the discharge is transparent, but purulent and bloody discharge is also found. Discharges, as a rule, occur with a bacterial form of pathology. In this case, immediate treatment is required to prevent further spread of the infection and the development of complications.
If the pathology is caused by E. coli, the discharge is characterized by an unpleasant fecal odor and a greenish tint.
With staphylococcus they are viscous, yellowish, with a fungal infection - white, curd-like.
In some situations, the symptoms of vulvitis are as follows:
- temperature increase;
- inflammation of the lymph nodes;
- nervousness, sleep disturbance.
Bad mood is often observed in young children who cannot clearly explain what exactly is bothering them.
Older patients are embarrassed to talk about it.
In the chronic form, swelling and hyperemia are not very pronounced. However, the itching and discharge remain. Acute vulvitis is characterized by more severe symptoms. Frequent relapses, chronic vulvitis, lack of timely treatment can lead to complications - cystitis, urethritis, vaginal atresia, cervical erosion and others.
Unfortunately, even caring parents often confuse redness and swelling with heat rash and diaper rash. They begin active treatment with drying agents, but this can only lead to aggravation of the situation. If the symptoms described above occur, it is worth showing the patient to a specialist as soon as possible in order to promptly begin treatment for vulvitis in girls.
Signs of pathology
Vulvitis is accompanied by the following symptoms:
- itching and burning in the genital area;
- pain that becomes stronger when urinating;
- swelling, redness of the mucous membrane, labia, clitoris;
- rarely - ulcers and erosions;
- vaginal discharge.
The last symptom depends on the origin of the disease. Vulvitis of a non-infectious nature is manifested by transparent, odorless leucorrhoea. When an infection occurs, they are purulent, and when the mucous membrane is damaged, they become bloody. The fungus causes a white, cheesy discharge to appear. Staphylococcus makes them thick and yellow in color. And E. coli are greenish with a specific “fecal” odor.
Important! The development of the inflammatory process may be accompanied by a deterioration in the girl’s general well-being.
A breastfeeding baby will cry often, sleep and eat poorly. Older girls become lethargic and try to run and play less, as movement increases discomfort. You may notice that they often touch the genitals, and often scratch them into blood.
Just yesterday, a cheerful and energetic baby becomes depressed, irritable, whiny, and sleeps poorly. With severe exacerbation, the temperature rises and the lymph nodes become inflamed.
If the cause of vulvitis lies in helminths, then the disease is accompanied by nausea, abdominal pain, and loss of appetite. In this case, the redness extends to the anus area. The anal folds become inflamed and thicker.
As the disease progresses to the chronic stage, it becomes less pronounced. Redness and swelling subside somewhat, but itching and discharge persist to varying degrees. Periodically, the disease makes itself felt with a new exacerbation. Vulvitis should not be allowed to become chronic, because it can provoke cystitis, urethritis, erosion and other pathologies of the genital and urinary organs.
These are lactobacilli that convert various compounds into lactic acid. Thus, a low pH level is constantly maintained in the vagina and in the area of the external genitalia. Such an environment prevents the proliferation of pathogenic microflora. However, children have practically no these lactobacilli, so vulvitis in girls develops under the influence of pathogenic microflora, frequent exposure to soap and other irritants.
About vitamins
In addition to drug therapy aimed at destroying the infectious agent, it is worth noting that the treatment complex necessarily includes vitamins in the form of synthetic forms or products enriched with vitamins (fruits, vegetables, legumes). And, of course, the disease is considered cured when the vaginal microbiocenosis is restored.
Restoration of microflora is carried out by taking probiotics (1st, 2nd, 3rd, 4th generations), prebiotics (Hilak-Forte), eubiotics or fermented milk products (yogurt, kefir of the Activia line).
Probiotics are prescribed depending on age. It is advisable for children under 6 years of age to take liquid forms. Probiotics include Bifidumbactrin, Lactobacterin, Bifiform, Linex, Kipacid. It is preferable to give newborn babies the probiotic Biogaia in drops (5 drops once a day, it can be mixed with milk or water).
Older children are prescribed Linnex:
- children under one year old, 1 capsule 3 times a day;
- children from 2 to 12 years old, 1-2 capsules 3 times a day;
- children over 12 years old: 2 capsules 3 times a day.
Hilak-Forte is also allowed for infants. The drug is prescribed 5-10 drops diluted in breast milk or boiled water for infants and 20-30 drops are approved for use in children over 2 years of age.
Hormonal
In girls, hormonal changes occur in the body during puberty. Changes in hormonal levels are also observed in women who have entered menopause. In both cases, the functioning of the Bartholin glands is disrupted, which leads to vaginal dryness and changes in microflora. Against this background, vulvitis often develops. If the patient goes to a medical facility, the doctor will prescribe her a hormonal ointment with corticosteroids. These medications include ointments:
- Antibacterial
Before prescribing an ointment, the doctor identifies the causative agent of the disease. Depending on this, the drug is selected.For antibacterial ointments:
Vulvitis of bacterial origin, like any infectious disease, requires complex treatment. Before using the ointment, it is necessary to treat the genitals with antiseptics. Along with external agents, medications for oral administration are also prescribed. The patient is recommended to take vitamins, minerals, and bifidobacteria.
Diagnosis of the disease
Diagnosis is carried out by a pediatrician or pediatric gynecologist. Only a gynecologist should treat vulvitis in girls.
Diagnostics consists of the following manipulations:
- Thorough examination, instrumental vaginoscopy, vulvoscopy. At this stage, objective changes are detected - redness, swelling, discharge.
- Vaginoscopy is used if there is a suspicion of a foreign object in the vagina. A special instrument is inserted into the vagina without touching the hymen.
- A general blood and urine test to rule out the possibility of infection spreading.
- Bacterial inoculation, microbiological study of the microflora of secretions.
- PCR scraping.
- Analysis for helminthic infestations.
- Scraping for enterobiasis.
- Allergy tests and others.
All diagnostic operations are aimed at identifying the true cause of the disease.
Self-medication of vulvitis can lead to its transition to a chronic form. The girl’s mother will think that everything has passed, however, this is not so. Sluggish or hidden progression of the disease can cause serious harm to children's health. That is why it is important to recognize it in time and distinguish it from ordinary diaper rash and irritation in infants, from cystitis and other diseases. Only a doctor can make an accurate diagnosis.
At the first symptoms, you should show the child to the pediatrician. During an external examination, he may suspect vulvitis and refer him to a pediatric gynecologist, who will confirm or refute these guesses. Here are the examinations and tests that show vulvitis in girls:
- bacterial culture and microbiological study of smears;
- scraping using PCR method;
- general blood and urine analysis;
- stool analysis for worm eggs and dysbacteriosis;
- scraping for enterobiasis;
- allergy tests;
- vulvoscopy;
- vaginoscopy.
The latter method allows not only to examine organs, but also to remove a foreign object from them when inflammation is caused by it. To establish the exact causes, the child may need to visit doctors other than a gynecologist. This is an allergist, endocrinologist, gastroenterologist. Based on research results, doctors determine how and with what to treat vulvitis in girls.
In most cases, when the above complaints appear, mother and girl turn to pediatricians.
The diagnosis of vulvitis can be made by a local pediatrician, but further observation and treatment should be carried out by a pediatric gynecologist in order to avoid complications!
Diagnosis is based on examination of the little patient, study of her life history and onset of the disease, and laboratory examination.
The main research method that allows us to identify the causative agent of inflammation is microscopic examination and bacteriological culture of vaginal secretions for flora and sensitivity to antibiotics.
If there is a suspicion that the nature of vulvitis is specific, then the scraping is examined using the polymerase chain reaction method. In addition, it is mandatory to undergo a general blood test, urine test, urine culture for flora and many other tests that the pediatric gynecologist will prescribe for you.
Therapy methods
Typically, treatment of the disease with prescribed medications is carried out at home. Hospitalization is indicated in severe cases or vulvitis is diagnosed in an infant. Inflammation at an early age is fraught with the development of complications, so the child should be under constant supervision of medical staff. If you follow all the doctor’s recommendations, the inflammation goes away completely in less than 10 days. Simple preventive measures, which Dr. E.O. described in detail in his video, will allow you to shorten the duration of treatment. Komarovsky:
- washing with plain water after each bowel movement;
- soap should be used for perineal hygiene no more than twice a day (sometimes for vulvitis, Citeal is used instead);
- put on the child loose cotton underwear, preferably white (to prevent allergies to fabric dyes);
- after washing the perineum, blot it with a tampon;
- Hygienic procedures must be carried out with movements from the navel to the buttocks.
Alternative medicine can help cure vulvitis in a child. Children can prepare sitz baths or lotions with decoctions of medicinal plants. You need to do the procedure 3 – 4 times a day. To do this, you can use recipes such as:
- prepare an infusion of chamomile at the rate of 2 tablespoons per liter of water;
- combine chamomile flowers, nettle leaves and string grass in equal quantities, pour 20 grams of the mixture into four glasses of boiling water, leave and strain;
- take a tablespoon of oak bark, add a liter of hot water and leave for several hours, the decoction can be used for baths or washing;
- take 10 grams of oak bark and chamomile flowers, 30 grams of nettle leaves and 50 grams of knotweed herb, prepare and use in the same way as oak bark decoction.
Additionally, the child needs strengthening therapy. For this purpose, multivitamins are prescribed in the form of syrups or chewable tablets. Immunostimulants (Echinacea preparations, Proteflazid, etc.) are also recommended. Allergenic foods (chocolate, strawberries, citrus fruits, eggs, nuts) should be excluded from the diet.
Treatment of vulvitis in girls is aimed at eliminating the causes of the disease and getting rid of unpleasant symptoms. So, if the inflammatory process is provoked by a foreign body, it is removed. Injuries and burns are treated with special ointments that promote rapid healing of the skin.
In the case of helminths, complete cleansing of the body is necessary. Endocrine disorders lead to problems throughout the body, and their treatment can be lengthy. Therapy for allergic vulvitis includes eliminating the source and using antihistamines.
Other types of vulvitis in children are treated with appropriate remedies. So, candidiasis is eliminated with antifungal agents, bacterial - with antibiotics. Tetracycline and Syntomycin ointments have proven themselves to be excellent for vulvitis in children.
Antibiotics must also be taken in tablet form in some cases. Their use disrupts the intestinal microflora, so taking probiotics is mandatory. To strengthen the body's defenses, vitamin complexes and immunomodulatory drugs can be prescribed.
Inflammation is well relieved with special ointments and suppositories. Folk remedies can also alleviate the condition, reduce itching and irritation. These include baths with infusions of calendula, chamomile, string, and oak bark. They are also carried out with potassium permanganate or furatsilin.
The main thing is that treatment at home should be carried out only with the permission and under the supervision of the attending physician. Different reasons, different means. By choosing an ointment at random, you can cause even more harm to the child. You shouldn’t rely on folk methods alone either. Treatment of most infectious vulvitis is impossible without the use of antibiotics.
Attention! During treatment, the girl is prescribed rest, proper and varied nutrition.
Foods that aggravate the inflammatory process should be avoided. These include fatty, spicy, smoked, salty dishes. In the case of an infant, nutrition should be adjusted to her mother.
And don't forget about the herbs!
In addition, many mothers willingly believe in herbal therapy. This is, of course, commendable! However, it should be noted that treatment with herbs alone in children is not allowed; plants must be used in addition to the main treatment with drugs.
It is believed that chamomile, sage, mint, and St. John's wort have beneficial properties in the treatment of vulvovaginitis in children. Herbs can be used both internally and externally, washing the child.
The procedures are recommended to be used daily. You can use decoctions and herbal infusions to wash the child. To do this, pour 2 filter bags with one liter of boiling water, leave, cool and wash the baby, without wiping it dry, but lightly wetting it with a towel.
It's easier to prevent than to treat!
There are measures to prevent vulvovaginitis in children. These include:
- hygiene of the girl, however, you should not wash the girl until she “shines”, so as not to wash away the beneficial microorganisms-defenders;
- You can bathe your child every day, but do not overuse cosmetic soap, especially antibacterial soap;
- daily change of underwear and the use of underwear made from natural fabrics, since synthetic ones do not allow air to pass through, thereby creating a “greenhouse effect”, and these are favorable conditions for the growth and reproduction of pathogenic microorganisms;
- increase the child’s immunity through hardening, daily walks in the fresh air, sports, balanced and nutritious nutrition.
In conclusion, I would like to appeal to all mothers: do not let the problem take its course, be sure to contact a specialist.
Possible complications
It is very important to detect the problem in time and begin proper treatment.
Otherwise, the following complications may develop:
- Cystitis is inflammation of the bladder.
- Synechia, vaginal atresia - gluing of the labia, vagina and their fusion.
- The appearance of scars, which may lead to problems in sexual life in the future.
- Imbibition is a bluish coloration of the mucous membrane that can persist for a long time or even for life.
- Kraurosis of the vulva and others.
If there is even the slightest suspicion that a girl is developing pathology, it is important to immediately seek medical help and not self-medicate.