Measles (rubella) is an acute infectious disease widespread throughout the globe, caused by an RNA virus of the genus Morbillivirus, family of paramyxoviruses, characterized by a clinically typical course of a febrile reaction, catarrhal lesions of the mucous membranes, especially the respiratory tract, and a specific papular rash gradually spreading throughout the body and a tendency to serious complications, especially dangerous in young children and older adults. After 20 years, the measles virus is tolerated worse in adults than, for example, from five to fifteen years in children.
The causative agent of measles
The virus of the genus Morbillivirus, which is the causative agent of measles, consists of a single strand of RNA. The thread is rolled into a spiral and is located in a spherical shell.
The causative agent of measles is one of the smallest microorganisms that can pass through bacterial filters; The location of the measles virus in the body is blood and mucous membranes.
The measles virus enters the body by airborne droplets and enters the mucous membrane through the respiratory tract. The virus then spreads through the blood throughout the body, reaching the lymph nodes and spleen, after which it multiplies intensively.
In the external environment, the measles virus dies quite quickly, especially in a dry environment, when exposed to ultraviolet rays of the sun, as well as when the temperature rises to 50°C and above. In a cool, humid room temperature, the virus can live for up to two days. When frozen, it can live up to 2-3 weeks, depending on the temperature.
Typically, children develop measles much more often; they are more susceptible to the virus, but adults tolerate the disease much more easily. Measles is rare in adults, but is much more severe and can cause complications.
Routes of infection
This virus has not been seen among animals; it spreads exclusively among humans. The source is a sick person; by the way, he is capable of infecting loved ones only in the last few days of the incubation period. Infectious disease specialists note only two ways of contracting the virus:
- aerogenic path (airborne droplets). You can become infected with the virus through coughing, sneezing, or normal conversation;
- transplacental method of infection. Presumably, the disease virus can be transmitted from a pregnant woman to a child, but such cases are extremely rare.
Good to know: How and where measles is transmitted
Measles symptoms
Measles symptoms vary depending on the period of the disease. Let us consider the symptoms of the cortex in adults and children, depending on the period. A more detailed description of the symptoms and course of the disease will be in the section on the clinical course of measles.
Symptoms of measles in children
Symptoms of measles in children and adults have a number of similarities. In children aged 5 to 15 years, the measles virus usually causes the least complications and develops lifelong immunity.
Prodromal period
(duration three to five days)
- temperature increase;
- fever;
- cough;
- runny nose;
- conjunctivitis;
- swelling of the face;
- fear of bright light;
- pain in the abdomen and epigastric region;
- red spots on the mucous membrane of the palate (on the second to fourth day after the measles virus entered the body);
- Filatov-Koplik spots are white spots on the mucous membrane of the cheeks that appear on the third to fifth day.
Rash period
(duration four to five days)
- most symptoms of the prodromal period persist;
- a measles rash appears.
Pigmentation period
(duration from seven to ten days)
- measles rash spots become pigmented;
- the skin dies and peels off.
Symptoms of measles in adults
Measles symptoms in adults are similar to those in children, but there are some differences.
Prodromal period
(duration three to five days)
- temperature increase;
- fever;
- cough;
- runny nose;
- conjunctivitis;
- intoxication;
- the lymph nodes in the neck become inflamed;
- swelling of the face;
- intolerance to bright light due to eyes irritated by conjunctivitis;
- pain in the abdomen and epigastric region;
- diarrhea;
- red spots on the mucous membrane of the palate (on the second - third day of illness);
- Filatov-Koplik spots are white spots on the mucous membrane of the cheeks that appear on the second to fourth day.
Rash period
(duration four to five days)
- most symptoms of the prodromal period persist;
- a measles rash appears;
- The rash appears in stages - on the head, on the torso and arms, then on the legs;
- cardiopalmus;
- low blood pressure;
- Petechiae appear on the skin.
Pigmentation period
(duration from seven to ten days)
- the rash gradually fades away;
- rash spots become pigmented;
- the skin is peeling;
- the patient's condition improves, the symptoms of measles gradually disappear.
List of sources
- Yushchuk N.D.; ed. Vengerov Yu.Ya. Infectious diseases: National manual / ed. M.: GEOTAR-Media, 2009
- Timchenko V. N., Levanovich V. V., Mikhailov I. B. Diagnosis, differential diagnosis and treatment of childhood infections (handbook). Ed. 3rd add. and re-ed. SPb.: ELBI-SPb. 2000;
- Children's infections. Handbook of a practicing physician. Ed. L.N. Mazankova. M 2009;
- Pokrovsky V. I., Onishchenko G. G. Cherkassky B. L. Evolution of infectious diseases in Russia in the 20th century. - M.: Medicine, 2003.
Clinical course of measles
Prodromal period
Measles rash develops after a prodromal period. In the prodromal period of measles, signs of exanthema specific to this process are not yet observed. Usually, when the measles virus enters the body, the measles patient becomes ill with catarrh of the mucous membranes of the respiratory tract, which provides a complete analogy with the clinical picture of influenza. A runny nose, conjunctivitis appear, the edges of the lower and upper eyelids swell - which is especially typical - and feverish temperature fluctuations appear.
The prodromal period of measles in the sense of catarrhal symptoms and febrile fluctuations usually lasts on average 3 days, but in rare cases it can last up to 8 days. From the moment of contact with a measles patient to the moment of the rash, exactly 13 days pass. The temperature course during the prodrome has a certain typical pattern.
On the first day of the prodromal period of measles, the temperature rises to 38°, on the second day it drops, and on the third day the temperature again sharply rises. A rise in temperature on the first day is usually associated with great concern on the part of others - they assume that some serious illness is developing. But the next day the temperature drops, and this reassures the parents, who believe that this is the end of the flu. Suddenly, by the evening of the 3rd day, the temperature rises again, and at the same time or the next day a rash characteristic of measles appears on the body.
During the prodrome of measles, there are certain typical phenomena on the basis of which, before the appearance of the rash, it can be predicted that a given patient will develop measles.
In addition to the signs described above, a typical symptom of measles is the presence of Filatov-Koplik spots on the oral mucosa. Filatov-Koplik spots in measles are usually localized on the mucous membrane of the cheeks in the area of the small molars. They are roundish white formations, with an uneven surface, located on a sharply hyperemic surface. These round formations range from 1 to 2 mm in diameter and tend to coalesce, which is a characteristic sign of measles.
If you look flatly at the mucous membrane of the cheek, you can see that in places it is covered with small white silvery elevations, and the cheek in this place gives the impression of being sprinkled with bran - this is also a symptom of measles. Filatov-Koplik spots often appear on the first day of the prodrome, develop more strongly on the second day of the prodrome, exist on the third and usually disappear when exanthema appears. Based on the presence of Filatov-Koplik spots, catarrhal phenomena and swelling of the edges of the eyelids, a diagnosis of measles can be made even before the appearance of a rash on the skin. Filatov-Koplik spots depend on the fact that the enanthema appears very early on the mucous membrane of the cheeks, and peeling of the fatty degenerated epithelium begins there.
This peeling of the epithelium with fatty degeneration creates the appearance of bran. Similar formations on the mucous membrane of the lips and gums can be found in some other rash diseases, and on the mucous membrane of the cheeks there are only one Filatov-Koplik spots and only one measles.
If you tilt the patient’s head back so that you can examine the mucous membrane of the hard palate, you will be able to see special irregularly shaped red spots of various sizes - primary measles enanthema, which appears on the mucous membrane of the hard palate a day before the measles rash appears on the skin. After 12 hours, you can see the same spots on the mucous membrane of the soft palate, on the arches, on the tonsils and on the back wall of the pharynx.
This enanthema in measles differs from scarlet fever in that the place of its first appearance is the mucous membrane of the hard palate and, secondly, in the fact that with measles the spots are large, irregular in shape, and with scarlet fever they are usually round, small - the size of a printed dot - and are placed in the center of the soft palate.
The period of enanthem with measles is often associated with a number of complications. One of them is nosebleeds. These bleedings are strong and persistent and depend on the duration of the prodromal period, sometimes lasting 7-8 days.
Starting long before the rash, they can lead the patient to a state of anemia and can be life-threatening. In addition, during the prodrome of measles, diarrhea often develops. Phenomena from the intestines and from the mucous membranes of the nose indicate that measles enanthema affects not only the mucous membranes of the respiratory tract, but also the mucous membranes of the digestive tract, creating their particular instability against the microbes growing there.
Period of rash and pigmentation
The period of measles rash is accompanied by an increase in temperature, which becomes even higher the next day, but from the 3rd day of rash the temperature begins to drop almost critically, becoming normal or subnormal on the 4th day. Thus, the disease itself usually does not last long: 3 days - the prodrome period, 3 days - exanthema, and then, with a normal course, the case ends happily.
In its usual form, measles exanthema occurs in the following sequence: first of all, it affects the center of the face - cheekbones, nose and forehead. Then this rash spreads to the cheeks and scalp. Thus, on the first day, the rash occupies prominent points and the center of the face and the scalp and cheeks. On the second day, the rash spreads to the rear surface of the body, spreads to the hands, partly to the forearms, slightly affecting the skin of the shoulders, by the end of the second day it occupies the front part of the body, stomach and sides. On the third day it affects the rest of the body, upper and lower extremities. During the period of a rash on the face, similar to smallpox, a rash also appears on the hands. The gradual spread of the rash and the merging of spots is one of the characteristic symptoms of measles.
Measles rash can come in many different forms. A typical measles exanthema is a roseolous-papular rash, initially small and then quite large, with a tendency to merge and, depending on this, forming more or less picturesque arabesque-like figures. It is usually bright red in color. In the spaces between the elements of the rash there are areas of completely normal skin, and not erythematous, as is the case with scarlet fever. The rash with measles is especially pronounced on the cheeks and on the back of the body. In these places and in the groin area, the rash merges into continuous spaces; in these areas you can see what appear to be spills or cracks - areas of completely normal skin.
Histological changes in measles exanthema consist of damage to the smallest capillaries of the skin and serous exudation from them with vacuolization of the surface epithelium of the skin. Measles rash spots become pigmented, the cells subsequently become necrotic, resulting in pityriasis-like peeling.
Then the condition improves, the cough and runny nose decrease, the measles virus dies from the antibodies that the body has produced.
General information
Measles is a viral disease that is infectious in nature and has an acute course. The disease is characterized by high temperature, which can reach up to 40.5 °C, as well as inflammation of the mucous membranes of the respiratory tract and mouth. Another characteristic sign of this disease is conjunctivitis and a maculopapular rash on the skin.
The first descriptions of measles appeared in ancient times. The disease is widespread in the world today, but it usually affects children. Previously, measles was also called measles rubella, but now this designation is not used so as not to confuse this disease with rubella. This disease is most serious in weakened children. Therefore, to this day, measles often causes child deaths in developing countries.
Complications of measles
Normal measles does not pose any danger, but its complications that cause a high mortality rate are dangerous. These complications of measles are concentrated in certain organs - some of them occur very often, others more rarely.
One of the rarest complications of measles is the so-called noma, or water cancer. Noma is usually formed in measles malnourished children, whose age does not exceed 3-5 years, and arises from a small, initially innocent-looking, white or gray spot on the mucous membrane of the cheek, approximately at the level of the canines or at the level of the first small molar.
This spot, which is nothing more than a nest of necrosis of the mucous membrane (often always one-sided), begins to deepen, and the cheek begins to swell. The process deepens into the thickness of the cheek, the cheek swells more and more and takes on a waxy color. This deathly, waxy color is so typical that without even knowing that the patient has an ulceration on the mucous membrane, we can say that he is beginning to have a noma. Gradually, the ulcer deepens, a sharp, fetid, sweetish gangrenous odor appears from the mouth, and a perforation of the cheek occurs. This ulcer, which is a wet gangrene, is often fatal. In malnourished girls, noma can develop in the genital area. With noma, as with other necrosis, spirochetes and bacteria fusiformis are almost always found.
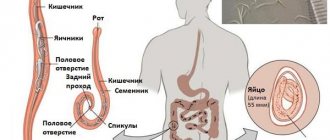
The second complication of measles is a catarrhal condition of the intestines. The mechanism of the disease is that measles poison affects the lymphatic apparatus, and the follicular apparatus of the intestine, especially in those suffering from exudative diathesis and in lymphatic patients, is so affected that a sharp swelling of the follicles and Peyer's patches results. Due to hyperemia, serous exudation and decreased resistance of the intestinal mucosa, enteritis begins. Those microbes that habitually vegetate on the intestinal mucosa begin to multiply, as the reactive forces of the body, which restrained their development within a certain framework and neutralized the products of their vital activity, weaken. The onset of measles is sometimes accompanied by vomiting and diarrhea, which can last the entire period of exanthema and has the character of enterocolitis. During the recovery period, after the end of the feverish state, the diarrhea disappears.
The worst prediction is given by the late form of enterocolitis, when during the recovery period the temperature rises again and frequent mucous stools begin. The amount of water in the stool increases sharply and quickly, flatulence appears, severe pain in the solar plexus area, and the picture turns into cholera infantum - dehydrating gastroenteritis; the temperature drops, and the child often dies due to uncontrollable diarrhea and vomiting. In other cases, the process turns into a picture of dysentery, and mucous-bloody stool appears due to infection with dysentery and paradysentery bacilli.
Diphtheria is also a fairly common complication of measles. The measles virus affects the body, weakening it, the person becomes susceptible to all infections and intoxications, therefore, of course, the diphtheria bacillus, which is a frequent guest of the nasal mucosa in children, begins to multiply in a child with measles and stimulates the fibrinous process.
The antitoxin that was in the blood and restrained its pathogenic effect loses its concentration in the blood. Due to the weakening of local and general immunity, those forms of diphtheria that complicate the course of measles are terrible; films with diphtheria in a measles patient can occupy not only the lumen of the larynx, trachea and large bronchi, but even all their branches down to the smallest bronchi, so that a cast of the bronchial tree is obtained. The film spreads with such speed that usually a child who has diphtheria plaque on the mucous membrane of the tonsils is affected by croup within a day, which, having become descending, quickly spreads to the small bronchi; Asphyxia occurs before the doctor’s eyes, because with such lightning-fast descending croup, neither intubation nor tracheotomy helps, and the anti-diphtheria serum has a weak effect.
Therefore, it is necessary to carefully ensure that a carrier of diphtheria does not get into the measles department, especially carefully monitor the throat and nose in patients suffering from measles, since the nose is the place where the diphtheria bacillus most often settles. Therefore, all patients arriving with measles have cultures taken from the mucus of the throat and nose, and all carriers are isolated. They are administered anti-diphtheria serum for prophylactic purposes.
The most common form of complications that occurs with measles is measles damage to the respiratory tract. Already a cough with a specific hue in a measles patient indicates that measles enanthema affects the mucous membrane of the larynx and trachea. This laryngo-tracheal cough in young children, up to 3-5 years old, very easily turns into the phenomenon of so-called false measles croup.
False measles croup is characterized by the fact that the child develops a barking cough and at the same time the phenomenon of laryngeal stenosis is detected against the background of measles. In general, each croup is divided into three periods - the dysphonic period, when the timbre of the voice changes, the dyspnoic period, when breathing becomes difficult, and the asphyxial period, when suffocation begins. Measles croup can quickly progress through all three stages and can become so severe that intubation and sometimes tracheotomy are necessary.
Measles croup especially often affects spasmophilic children who suffer from both exudative diathesis and lymphatism. In the latter, during measles, swelling of the bronchial glands is pronounced; bronchial glands compress the adductor bronchi, compress the lower end of the trachea and cause spasms of the laryngeal muscles due to compression of the nervus laryngeus recurrens (recurrent laryngeal nerve). The swelling of the mucous membrane also plays an important role in the narrowing of the larynx, which further narrows the laryngeal opening. In addition, periodic convulsive compression of the laryngeal fissure is observed, accompanied by symptoms of dyspnea. Measles false croup is more often observed in cold winter times and in patients in cold rooms.
Measles poison can also affect the lower respiratory tract - it affects the bronchi, down to the smallest branches, as a result of which the phenomena of deep bronchitis develop. Measles bronchitis is a common occurrence in children with measles, even in cases where the small bronchi are not affected. The cough worsens at night, and therefore children sleep poorly during the day and even worse at night; at the same time, their blood circulation in the area of the small circle becomes difficult. This bronchitis tends to develop into bronchopneumonia against the background of measles.
The usual course of measles bronchopneumonia, if it ends favorably, lasts from 8 days to 2 weeks. The mechanism of development of this bronchopneumonia is typical. The measles virus causes hyperemia of the lung tissue and affects the mucous membrane of the respiratory tract down to the smallest branches of the bronchi, resulting in swelling of the mucous membrane. In connection with this swelling, the activity of the mucous glands changes, an increased secretion of mucus results, and as a result, such mucus plugs clog some of the smallest adductor bronchus.
Further complications of measles are complications of pneumonia. Pneumonia can be complicated by purulent pleurisy, causing suppurative fever. These pleurisy occur on the 8-10th day of the course of pneumonia. You should always remember about their possibility and take into account not only the results of percussion, but also vocal tremors.
Involvement of the middle ear is far from uncommon with measles, and in some epidemics, serous-purulent inflammation of the middle ear was observed in a higher percentage of cases than with scarlet fever, also affecting adults. The course is similar to the course of the same disease with scarlet fever; sometimes the mastoid process is also affected.
Kidney damage due to measles is rarely observed: as a rule, with toxic hemorrhagic measles, in the form of acute glomerulo-nephrito-nephrosis. Due to the severity of the hemorrhagic toxic form, this nephritis flows parallel to the main process.
The nervous system is affected by measles in spasmophilics and rickets. During the onset of the rash, they may develop convulsions, with loss of consciousness, and the phenomenon of meningism. They often experience the phenomenon of spasm of the glottis. These spasms of the glottis are especially pronounced when whooping cough is complicated by measles. Of course, bronchopneumonia with these combinations is observed almost as a rule. Measles encephalitis may also occur; their course is favorable.
Prevention
The measles vaccine was created in 1963. There are currently several live measles vaccines available.[12]
The measles vaccine is very effective[31]. After one dose, 85% of nine-month-old children and 95% of twelve-month-old children are immune[32]. Almost everyone who does not develop immunity after the first dose becomes immune after the second dose.[31] The World Health Organization recommends that children receive their first vaccination at nine months of age in areas where the disease is common, and at twelve months of age in areas where the disease is rare[31], previously in developed countries vaccination was carried out between 12 and 18 month of the child's life; In the event of an epidemic, it is possible to vaccinate children from the age of six months [11] (in this case, the vaccination cannot be counted as the first of two doses of vaccination).
Since the 1980s, to ensure the highest possible level of immunity, and due to the shift in the vaccination age in many countries from 12-15 months to 9 months, vaccination with two doses of the vaccine has been recommended[33].
Because measles is only transmitted between people, can be reliably diagnosed, and existing vaccines are quite effective at reducing the spread of the disease, measles could in principle be completely eradicated[11]. According to modern ideas, to completely eradicate measles in the country, the coverage level with two doses of the vaccine in each of its districts must be at least 95%[12].
The vaccine's protective effect lasts for many years, and it can protect against disease when administered within a few days of infection. It remains unclear whether the vaccine becomes less effective over time without the natural booster provided by exposure to live virus.[31]
Some studies show that 10 years or more after the last vaccination, 30-40% of those examined do not have protective levels of antibodies; thus, complete eradication of measles may require booster vaccination in adults every 10 years.[34]
In case of illness, all unvaccinated contact persons over 1 year of age are given emergency vaccine prophylaxis; if there are contraindications, immunoglobulin is administered.
In order to create active immunity, routine vaccination with live measles vaccine (LMV) is carried out in accordance with the vaccination calendar, as well as for children and adults in the absence of measles antibodies. The complex of anti-epidemic measures in the outbreak of infection includes identifying the source of infection, contacts who had the fact of unconditional or probable communication with the patient, to establish the boundaries of the outbreak.
The source of infection is isolated for the entire infectious period (until the 4th day of the rash). Children who were in contact with him and adults working with children (with the exception of persons who have previously had measles, who have been vaccinated, who are seropositive with a titer of anti-measles antibodies of 1:5 or higher) are subject to separation from other children for 17 days (with the introduction of immunoglobulin - 21 days ).
Emergency prophylaxis with normal human immunoglobulin is carried out in the first 5 days after exposure to children from 3 to 12 months. and pregnant women.
A differentiated serological examination is desirable to identify seronegative individuals followed by vaccination with LCV or other measles vaccines.
Dosage form of the vaccine
Live measles vaccine is used either as a monovalent vaccine or as a measles-containing vaccine (MCV), in combination with rubella, mumps and varicella vaccines, as part of the MMR and MMRV combination vaccines, or other combination vaccines. The vaccine works equally well in all dosage forms. The vaccine is produced in the form of a powder, which must be mixed immediately before administration subcutaneously or intramuscularly. The effectiveness of the vaccine is checked using a blood test.[31][12]
Vaccine safety
The vaccine is generally safe, including for patients with HIV infection. Side effects are usually mild and go away quickly. These include pain at the injection site or mild fever. Within 7-12 days after vaccination, 5% of vaccine recipients develop a temperature above 39.4 °C for 1-2 days, 2% develop a rash, and 1 in 3,000 develop febrile seizures (English febrile seizure), one in 30,000 has thrombocytopenic purpura. One case of anaphylaxis has been reported in approximately one hundred thousand vaccinations. There has been no increase in the incidence of Guillain-Barré syndrome, autism, or inflammatory bowel disease.[12]
Although measles vaccination is performed with a live virus, transmission of the vaccine strain of measles virus among humans has not been documented[12].
In Russia
In accordance with the Russian national vaccination calendar, which was approved by order of the Ministry of Health of the Russian Federation No. 125n dated March 21, 2014[35], vaccination against measles is carried out with a combined live vaccine against measles, rubella and mumps simultaneously at the age of 12 months, revaccination - at 6 years .
In accordance with the same order, vaccination against measles and revaccination against measles are indicated for all children and adults aged 1 to 35 years if they have not been sick, are not vaccinated, have been vaccinated once against measles, or do not have information about vaccinations against measles . In the age category of 36-55 years, under the same conditions, measles vaccination is indicated for representatives of certain professions - doctors and teachers, employees of trade, transport, public utilities and social spheres[36].
In 2002, Russia adopted the National Measles Elimination Program by 2007-2010[37].
Coverage of two doses of measles vaccine in Russia has corresponded to the WHO recommended level (over 95%) since 2003[38].
Diagnosis of measles
The diagnosis of measles can be difficult only before the rash and in cases of rudimentary measles in adults - during the rash.
For diagnosis during the prodromal period, essential symptoms are: catarrh of the mucous membranes of the respiratory tract, swelling of the edges of the eyelids, Filatov-Koplik spots and enanthema.
Early diagnosis of measles is of particular importance in view of the most highly infectious nature of measles during the prodrome and at the end of incubation.
During the period of rash, the diagnosis is based on the typical sequence of stages of the rash, the papularity of individual elements, their softness to the touch, their tendency to merge and form figures, and a sharp increase in temperature at the onset of the rash.
Characteristics of measles rash
Characteristic signs of measles rash are Koplik-Filatov spots and measles enanthema. Their presence helps to make a diagnosis and prescribe timely treatment.
Laboratory diagnostics
When the first symptoms appear, you should consult an infectious disease doctor. After a thorough examination, laboratory tests will be ordered to confirm infection with the measles virus.
Laboratory tests include: general blood test, urine test and enzyme immunoassay.
| Analysis | results |
| General blood analysis | Decrease in the number of leukocytes: neutrophils, monocytes and lymphocytes, moderate increase in erythrocyte sedimentation rate |
| General urine analysis | Increased white blood cells, protein precipitation |
| Linked immunosorbent assay | Detection of the amount of immunoglobulin M (IgM). The test is positive if the amount of IgM is ≥ 0.18 IU/ml |
Other tests are not helpful in making a diagnosis of measles and are used to determine the extent of complications.
Treatment of measles
There is no specific treatment for measles, so they are limited to the use of symptomatic remedies aimed at alleviating the patient’s condition. The basis of symptomatic therapy is mucolytic and anti-inflammatory drugs.
It is also recommended to use vitamin A, and to reduce skin itching - rinsing it with a solution containing delaxin powder. The oral cavity is rinsed with chamomile infusion.
When measles is complicated by bacterial pneumonia, antibiotics are used; in severe cases of croup, corticosteroids are used.
Often, to treat measles and prevent infecting others, the patient is hospitalized.
Treatment tactics
Measles treatment is carried out at home. After visiting an infectious disease specialist, the patient is recommended: bed rest, diet, therapy. The doctor should visit the patient several times a week.
In case of severe disease, severe intoxication syndrome, or the presence of serious complications, treatment is carried out in a hospital setting.
The diet for measles should consist of high-calorie foods and plenty of vitamins. You need to drink about 2-3 liters of fluid per day.
Attention! There is no etiological treatment for measles. Treatment of measles with medications consists of symptomatic treatment.
Cytokines serve to restore the functions of the immune system. They are characterized by an antiviral effect and suppression of viral replication.
Cytokines include:
- “Leukinferon” – 1000 IU intramuscularly for 5 days,
- anti-measles gamma globulin – 5.0 intramuscularly.
Antihistamines will help eliminate the allergic reaction. They reduce the size of the rash and normalize the general condition. These include:
- loratodine – adults 1 tablet once a day, children syrup – 5 ml once a day,
- tavegil – 1 tablet 3-4 times a day,
- Diphenhydramine – 2 ml IM once every 24 hours.
Non-steroidal anti-inflammatory drugs are used to reduce high body temperature. They have antipyretic, analgesic and anti-inflammatory effects. These include:
- ibuprofen – 1 tablet 1-2 times every 24 hours,
- paracetamol – 1 tablet 1-2 times a day,
- baralgin – 5.0 intramuscularly 1 time per day.
For expectorant purposes, it is recommended to take: ambroxol and bromhexine.
To combat conjunctivitis, eye drops are recommended - Albucid (course of therapy for 5-8 days).
As vitamin therapy - undevit, vitamin B-complex.
To prevent the development of a bacterial infection, broad-spectrum antibiotics are prescribed - augmentin, ceftriaxone, clarithromycin.