Being viral in nature, the incubation period of hepatitis A is characterized as short-term and is approximately 1 month. Affecting the full functioning of the liver, the disease becomes one of the common forms of hepatitis, referred to as Botkin's disease. Remaining virulent for a long period, the virus is found on household objects, water and food.
The concept of viral infection of the gland
Initially, hepatitis was an infectious inflammation of the liver, accompanied by a characteristic yellow color of the skin and sclera of the patient. As liver diseases were studied, capital letters of the Latin alphabet began to be added to the name “hepatitis” in accordance with the sequence of discovery of the pathogen. The isolated viruses use a similar infection mechanism, affecting the human hepatobiliary system, disrupting its normal functioning, and all, without exception, are highly contagious. The differences are expressed in the complexity of the disease, its duration, and consequences for the body.
Viral hepatitis is one of the most common pathologies in the world.
Pathogens
Viruses that are pathogens continue to be discovered to this day. The following varieties have been sufficiently studied: A, B, C, D, E. Types F, G, TTV, SEN are still being studied. Some types of viruses (for example, hepatitis C) are further divided into types or subtypes. Any type of disease is highly contagious.
Peculiarities:
Viruses that lead to hepatitis are very dangerous and insidious.
Hepatitis A accounts for 40% of acute viral forms, which is associated with the mechanism of transmission of infection. In countries where access to clean water is difficult, the rate of infection by the virus can be explosive, which is why the disease is known as epidemic hepatitis.- The hepatitis B virus is the most contagious. This means that it persists for years in blood products and on instruments that have not been sterilized; its antigen is detected even after several months.
- Strain C is recognized as the most dangerous and difficult to diagnose. There are often no significant symptoms, and by the time the infection is detected, the liver has severe damage. There is no vaccine, so anyone can get infected.
Hepatitis A: symptoms, diagnosis, treatment
Home » Infectious diseases »
- 6.1 Post-exposure prophylaxis
Hepatitis A
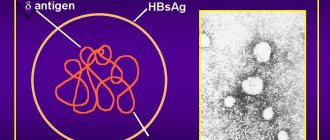
Hepatitis A virus (HAV) is an RNA virus. It is not associated with chronic liver disease.
The route of transmission is fecal-oral; therefore, it is more common in settings with poor hygiene. Most infections in adults are symptomatic, while 70% of infections in children under 6 years of age, who are also a key reservoir of transmission, are asymptomatic.
On average, the incubation period lasts 28 days.
Etiology
Hepatitis A virus (HAV) is a 27 nm non-enveloped, icosahedral RNA virus. Due to the absence of a lipid membrane, the virus is resistant to lysis in the gallbladder.
The virus is resistant to freezing, detergents and acids. It is inactivated by formalin and chlorine. The virus survives on human hands and objects through which infection can be transmitted and requires temperatures above 185°F (85°C) to inactivate it.
HAV survives for long periods in seawater, freshwater, wastewater and soil. The virus is spread through close contact with an infected person or through contact with contaminated food or water.
Pathophysiology
Following oral infection, the virus is transported across the intestinal epithelium by a poorly understood transport mechanism. After moving through the mesenteric veins to the liver, the virus enters hepatocytes, where hepatitis A virus (HAV) replication occurs exclusively in the cytoplasm using RNA-dependent polymerase. The exact mechanism of injury has not been proven, but there is evidence suggesting a role for a cell-mediated immune response, which has been shown to be mediated by LAP-restricted, HAV-specific CD8+ T lymphocytes and natural killer cells.
The role of gamma interferon in promoting the clearance of infected hepatocytes has been described. Excessive host response (clinically observed when HAV RNA levels are severely reduced during acute infection) is associated with severe hepatitis. Then HAV is released from the hepatocyte into the sinusoids and bile ducts, and then with bile into the intestine, where excretion occurs in feces.
Diagnostics
Post-exposure prophylaxis for the patient and their close contacts should not be delayed while awaiting test results if there is reasonable clinical certainty about the likelihood of infection.
Anamnesis
A careful history may indicate relatively significant risk factors, including residence in an endemic region, close personal contact with an infected person, men who have sex with men, travel to high-risk areas, use of illicit drugs, known outbreak of food poisoning and exposure with a child or a kindergarten employee.
The disease can also be acquired through direct contact with contaminated water or ice, including shellfish collected from water contaminated with waste or food contaminated by infected food workers. In approximately half of the recorded cases, the risk factor was not identified.
The history should also assess the risk or history of other liver diseases, such as hepatitis B and hepatitis C virus infections and/or cirrhosis, since concomitant hepatitis A virus (HAV) infection in such settings has a higher risk of progression to fulminant HAV .
Symptoms and signs
The incubation period lasts on average 28 days (15–49 days). The clinical course of the disease can be divided into the pre-icteric phase and the jaundice phase. The pre-icteric phase lasts 5–7 days and is characterized by the sudden development of nausea, vomiting, abdominal pain, fever, weakness, fatigue and headache. Relatively less common symptoms include arthralgias, myalgias, diarrhea, constipation, cough, itching and urticaria.
Physical signs may include splenomegaly, right upper quadrant pain with a tender enlarged liver, posterior cervical lymphadenopathy, and bradycardia. Over the course of several days to 1 week, the jaundice phase begins with dark urine, acholic stools, jaundice and itching. As jaundice develops, the symptoms of the pre-icteric phase usually weaken. Jaundice usually peaks in the 2nd week.
Fulminant disease occurs in <1% of patients and is characterized by worsening jaundice and encephalopathy associated with severe liver dysfunction or severe hepatocyte necrosis in the absence of underlying liver disease. This is due to an excessive immune response of the host.
Diagnostic tests
Determination of liver enzymes and serum bilirubin levels should be ordered immediately after the onset of clinical symptoms.
Transaminase levels can reach more than 10 thousand units/l, although the correlation between enzyme levels and the severity of the disease is insignificant. Serum alanine aminotransferase (ALT) levels are usually higher than serum aspartate aminotransferase (AST) levels. While alkaline phosphatase levels are usually minimally elevated, bilirubin levels are typically elevated to approximately 85.5–171.0 µmol/L (5–10 mg/dL).
Baseline blood urea, serum creatinine, and prothrombin time (PT) values can also be determined. Although renal failure is uncommon, it is a well-recognized fact in HAV infection. Patients with fulminant hepatitis have serum creatinine levels greater than 177 µmol/L (2 mg/dL), increased PT, and serum ALT levels less than 2600 U/L.
In parallel, it is possible to determine the determination of IgM class antibodies to HAV and IgG class antibodies to HAV. Anti-HAV IgM is positive at the time of symptom onset, peaks during the acute or early convalescent phase, and remains positive for approximately 4–6 months. Laboratory test data must be correlated with clinical signs. Some asymptomatic patients may have had previous HAV infection with prolonged presence of HAV IgM. Both false-positive results and asymptomatic infection are possible (more common in children under 6 years of age).
IgG antibodies to HAV can be detected for decades. Other diagnostic methods include detection of HAV RNA in stool, body fluids, serum, and liver tissue. Often they are not necessary and serve only as auxiliary tools in research laboratory settings.
Differential diagnosis
| Disease | Differential signs/symptoms | Differential examinations |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Treatment
Treatment strategies are individualized; if necessary, appropriate consultants are involved, which depends on certain characteristics of the patient.
Post-exposure prophylaxis
Active or passive immunization is useful for protection following exposure to hepatitis A virus (HAV) infection. Different countries may have slightly different recommendations regarding post-exposure prophylaxis, so national guidelines should be consulted.
Post-exposure prophylaxis using intramuscular immune globulin without delay for serological testing has been shown to be effective and is the standard of care.
In 2007, the CDC guidelines were revised to allow the vaccine to be used to prevent hepatitis A in healthy individuals 1 to 40 years of age who have been exposed to HAV infection. This recommendation is based on the results of a randomized, double-blind, noninferiority trial comparing the vaccine and immune globulin. After recent exposure (<2 weeks), CDC recommendations for persons who deny prior vaccination include administration of a single antigen hepatitis A vaccine at an age-appropriate dose or immune globulin as soon as possible after exposure. Guidance regarding vaccine or immune globulin administration includes the following.
- Healthy people aged 12 months to 40 years: Single antigen vaccine is preferred to prevent hepatitis A.
- People over 40 years of age: Immune globulin is preferred, although a vaccine can be used if immune globulin is not available.
- Children younger than 12 months, immunocompromised individuals, individuals with chronic liver disease, and individuals allergic to the vaccine: Immune globulin should be given.
The CDC recommends post-exposure prophylaxis in the following situations.
- All previously unvaccinated members of the same household that contains a person who has been serologically confirmed to have hepatitis A.
- Sexual contacts of a person with serologically confirmed hepatitis A.
- Persons who use illicit drugs with another person who is serologically confirmed to have hepatitis A.
- All previously unvaccinated staff members and visitors to child care facilities in which: One or more cases of hepatitis A infection have been identified in children or staff, or
- Cases have been confirmed in 2 or more households of center visitors.
Confirmed infection: supportive care
Treatment for CAA is primarily supportive, including appropriate rest if necessary. Avoiding excessive use of paracetamol and alcohol, as well as a balanced diet are important.
There is no specific antiviral treatment. The study indicated the practicality of using bile acids in viral hepatitis. Although it has been noted that they may improve liver biochemistry in patients with hepatitis B or C, there are no studies evaluating the use of bile acids in patients with HAV.
After the development of an acute infection, treatment is mainly outpatient. Rarely, hospitalization may be necessary due to dehydration, coagulopathy, or encephalopathy. Contact precautions are taken during the infectious period, especially in the group of patients with urinary or fecal incontinence or in patients with diaper requirements. In healthy individuals, the period of contagion lasts approximately 2 weeks after the onset of the disease. Certain groups of patients remain infectious for up to 6 months. These include children and immunocompromised patients.
Confirmed infection: referral for liver transplantation
<1% of patients develop fulminant disease, which is characterized by worsening jaundice and encephalopathy. In such cases, surgical referral to a center that performs liver transplantation is indicated. This plays a particularly important role in patients with concomitant infections caused by hepatitis C or hepatitis B virus or cirrhosis of any etiology. In such conditions, HAV infection has a higher risk of developing fulminant disease. A prognostic index that consists of 4 clinical and laboratory signs (serum alanine aminotransferase (ALT) <2600 U/L, creatinine >177 µmol/L [>2 mg/dL], intubation, blood pressure medications) predicts the likelihood of transplantation/death significantly better than other published models.
Lower ALT levels, which were found to be one of the indicators of poor prognosis, were considered associated with widespread necrosis at admission.
List of sources
- Kim DK, Riley LE, Harriman KH, et al. Advisory Committee on Immunization Practices recommended immunization schedule for adults aged 19 years or older - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020 Feb 10;66(5):136-8.
- Robinson CL, Romero JR, Kempe A, et al. Advisory Committee on Immunization Practices recommended immunization schedule for children and adolescents aged 18 years or younger - United States, 2017. MMWR Morb Mortal Wkly Rep. 2020 Feb 10;66(5):134-5.
- Taylor RM, Davern T, Munoz S, et al. Fulminant hepatitis A virus infection in the United States: incidence, prognosis, and outcomes. Hepatology. 2006 Dec;44(6):1589-97.
- Fujiwara K, Kojima H, Yasui S, et al. Hepatitis A viral load in relation to severity of the infection. J Med Virol. 2011 Feb;83(2):201-7.
- Ajmera V, Xia G, Vaughan G, et al; the Acute Liver Failure Study Group. What factors determine the severity of hepatitis A-related acute liver failure? J Viral Hepat. 2011 Jul;18(7):e167-74.
- Shin SJ, Kim JH. The characteristics of acute kidney injury complicated in acute hepatitis A. Scand J Infect Dis. 2009;41(11-12):869-72.
- Centers for Disease Control and Prevention. Positive test results for acute hepatitis A virus infection among persons with no recent history of acute hepatitis: United States, 2002-2004. MMWR Morb Mortal Wkly Rep. 2005 May 13;54(18):453-6.
- BMJ
Connect with
I authorize you to create an account for me
When you first log in using social networks, we receive public information from your account provided by the social network service provider as part of your privacy settings. We also automatically receive your email address to create your account on our website. When it is created, you will be authorized under this account.
DisagreeAgree
Connect with
I authorize you to create an account for me
When you first log in using social networks, we receive public information from your account provided by the social network service provider as part of your privacy settings. We also automatically receive your email address to create your account on our website. When it is created, you will be authorized under this account.
DisagreeAgree
Subscribe
Transmission mechanism
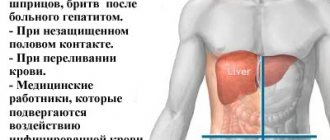
Depending on the transmission mechanism used, the disease is divided into two groups:
- Fecal-oral (types A and E). Carriers of infection are dirty hands, unwashed vegetables and fruits, and drinking water. Failure to comply with personal hygiene rules and lack of heat treatment of food are guaranteed to ensure transmission of the virus.
- Parenteral (strains B, C, D). The source of infection is blood and other biological fluids, which become infectious after the virus spreads in the body. Methods of transmission are associated with the use of undisinfected instruments and unprotected sexual contact. A specific source of viral hepatitis B is amniotic fluid, which reaches the child through the placenta or during passage through the birth canal (vertical transmission).
You should not give up breastfeeding, since the causative agent of hepatitis B and C is not transmitted through breast milk, but it is important to monitor the integrity of the skin of the mammary glands.
The main route of transmission of hepatitis C is through blood. A small amount of the virus cannot cause infection through unprotected sex or vertical transmission. But there are factors that contribute to infection, in particular bacteria and viruses (including HIV). They reduce immunity or cause skin damage. A carrier of hepatitis C is not contagious in everyday interactions.
Duration of the period
Many people are concerned about the question - how long is the incubation period of hepatitis A? It can vary from fifteen to fifty days, but the average is twenty-eight days. This disease differs from other types of viral hepatitis in the shortest incubation period. Knowing its duration is very important, since during such a period of time it is necessary to monitor the contact person, be it an adult or a child. This will make it possible not to miss the onset of Botkin’s disease and notice its minimal manifestations.
There are several factors that influence the duration of this period, including:
- extensive viral load - this means that at the time of infection a large amount of the pathogen entered the body at once. It is worth noting that the hepatitis A pathogen can be transmitted in such ways as close contact with an infected person, using the same household items, consuming contaminated foods and liquids;
- the ability of the immune system to resist the HAV virus. The duration of incubation may decrease due to lack of sleep, stress, severe physical fatigue, malnutrition, hypothermia or overheating of the body;
- age category of the infected person - the shortest interval between infection and the appearance of the first signs is observed in children and the elderly. In the first case, this is explained by not fully formed immunity, and in the second, by a significant deterioration in the body’s ability to resist infectious processes.
Mechanism of transmission and incubation period of hepatitis A
Disease development and symptoms
Influenza is the manifestation of the disease in most cases.
The clinical picture varies for all forms of the disease, but the same stages of progression are distinguished for all:
- Incubation. The period from the virus entering the body to the first symptoms. The shortest is for hepatitis A (from 15 to 30 days); a carrier of hepatitis B or C may not be aware of infection for up to six months. Depends on the amount of virus that has entered the body, the type of virus, and the state of the person’s immunity.
- Preicteric. Hepatitis A is characterized by a rapid (5-7 days) and acute course of this stage, with an increase in body temperature to 38-39 ° C. In parenteral hepatitis, the duration is 7-12 days, the symptoms are mild:
- weakness,
- sleep disturbance,
- fever or chills,
- sweating,
- itching, rash.
- Jaundice. Duration can be 7-15 days (hepatitis type A), 1-3 weeks (type B). Hepatitis C is characterized by a mild manifestation of this stage. Symptoms:
- yellowing of the mucous membranes, sclera, skin;
- darkening of urine;
- stool lightening.
- Recovery stage. The period from the beginning of a reduction in symptoms to their complete disappearance and normalization of blood counts. It is important to continue the prescribed therapy, otherwise a relapse may occur or a virus carrier may develop.
Main risk groups
There are several groups of people who are most susceptible to infection with this virus. The main risk categories are:
- workers of medical and children's institutions - due to the fact that hepatitis A is transmitted through contact with blood or the use of shared cutlery;
- food service employees - the danger of infection lies in the fact that such people are forced to come into contact with products grown in contaminated areas;
- military personnel who may end up in countries of Asia and Africa, where the incidence of Botkin's disease reaches high levels;
- drug addicts - viruses are transmitted through a contaminated needle used by an infected person;
- persons who had direct contact with the patient’s household items;
- homosexual men;
- patients suffering from other severe liver diseases;
- tourists and travelers visiting countries with a high incidence of hepatitis A;
- family members who have a patient with a similar diagnosis.
It is these factors of transmission of the hepatitis A virus that require vaccination against such a disease, which must be carried out for both adults and children. This measure is mandatory, despite the fact that the disease often has a favorable prognosis and quite rarely leads to the development of complications.
It is worth noting that the main difference between Botkin’s disease and other viral liver lesions is that after recovery the patient develops lifelong immunity. However, this is not a reason to refuse vaccination. In addition, today there are a large number of preventive recommendations, compliance with which minimizes the likelihood of infection with this virus.
Diagnostics
A person’s attention to the signals of his body plays a huge role in diagnosis. It is dangerous to ignore the appearance of seemingly harmless ailments: weakness, lack of appetite, fatigue, nausea. A timely visit to a doctor will allow you to begin treatment, preventing the disease from becoming severe and becoming chronic.
Laboratory tests for the presence of pathology or its carriage:
- Blood tests: general - reveals the inflammatory process);
- biochemical - shows a disturbance in the functioning of the liver);
- enzyme immunoassay - identifies the pathogen using markers).
Symptoms of the disease
Basic hygiene rules will help reduce the risk of contracting hepatitis A.
Hepatitis A infection is widespread. The infection is considered a disease of “dirty hands” and spreads more often in the warm season. This virus often affects children due to fragile immunity. Manifests itself in the form of fever, photophobia, cough, runny nose, lacrimation, headache, nausea, loss of appetite, as well as jaundice.
Hepatitis B enters the body through blood transfusion, through contaminated medical instruments, through manicure accessories, through tattooing, piercing and sexual intercourse. Primary signs are blurred. The disease is difficult to treat. Symptoms manifest themselves in the form of joint pain, fatigue, weakness, and indigestion.
Virus C is detected accidentally during preventive examinations and when blood is collected for clinical studies. If the disease is diagnosed at an early stage, there is a chance of complete recovery. Viral hepatitis causes pathologies of the liver and pancreas. Symptoms are similar to type B virus.
Virus D is a parasitic virus that develops only in the presence of virus B. The effects of two types of infection on the liver have a detrimental effect on the human body. The symptoms are similar to those of hepatitis B, but with the addition of signs of indigestion, temperature variability, and malaise.
Hepatitis E is transmitted by the fecal-oral route, through contaminated water, and through household contact. This type of virus is found in tropical countries and the Central Asian region. The main symptoms of the disease are similar to other types of hepatitis. It has a severe course, which in some cases leads to hepatic coma. It affects teenagers more often.
Treatment: what is important to know?
Treatment is individual, comprehensive and long-term.
Antiviral, pathogenetic and symptomatic agents are used. Therapeutic measures are aimed at starting recovery processes and removing damaged cells from the liver. Treatment is carried out based on the results of examination of the patient, taking into account the following:
- A minimum of drugs is used, reducing the load on the liver, the structure of which is already damaged by the virus.
- Treatment of concomitant chronic pathologies occurs after normalization of liver function, if they are not life-threatening.
- Bed rest.
- Dieting. Without it, the disease cannot be treated.
Prevention
Hepatitis is a serious pathology, often becoming chronic and causing complications. Prevention is not commensurate with measures to restore health. These are the rules of personal hygiene known from childhood, heat treatment of food, and thorough washing of food. It is dangerous to use other people's personal hygiene products. When undergoing cosmetic procedures in a salon, be sure to inquire about disinfection methods and ask for a health certificate. A carrier of the virus can become infected through the slightest cut with an unsterile instrument. Avoid sex without a condom and find the opportunity to get vaccinated against viruses A and B, they are the most reliable protection.
Determining the source of infection
Any system to prevent any disease must always determine the source of infection. This step is a priority and very important for localizing the source of the virus in order to prevent its further spread.
Isolation of patients from the moment the first signs appear can significantly reduce the incidence of disease in the epidemic area. But in the case of hepatitis A, these anti-epidemic measures are not effective enough, since not only patients with severe symptoms are infectious, but also people with subtle signs of the disease and even without symptoms at all.
The fact that they may be carriers of the hepatitis virus can only be determined through modern laboratory tests. It is also important that a person becomes infectious when the incubation period has not yet ended and there are no signs of illness.
From the above, we can conclude that at the moment there is no complete identification of the localization of the source of the disease, however, examination of all adults and children who have come into contact with a patient with hepatitis A is mandatory.
Medical workers are required to report each case of disease (or suspicion of hepatitis A) by telephone within two hours, and then in writing, no later than 12 hours later, provide a written report to the authorities carrying out state sanitary and epidemiological surveillance at the place where the disease was registered.
After each change and clarification of the diagnosis, the provision of all data within a twelve-hour period is also required.
Kindergartens are quarantined and no new children are transferred or accepted until the end of the incubation period. The same goes for the staff. Any violation of the regime can lead to the spread of infection.
If it is necessary to accept new children into such groups, the following activities are required:
- Epidemiologist's conclusion.
- Preliminary administration of immunoglobulin.
- It is advisable that these children have at least one vaccination against hepatitis A (using drugs such as Havrix, Avaxim, HEP-A-in-VAK, etc.).
Quarantine lasts 35 days from the first recorded disease. If someone else in the group gets sick, then the countdown of quarantine time starts from that sick person. This cycle is repeated until a full 35 days have passed since the last patient was identified. After this, the group can be removed from quarantine.
During the incubation period, everyone who had contact with the sick person undergoes a thorough examination of the skin, mucous membranes, and whites of the eyes every day. During the initial examination, the size of the liver and spleen, as well as the appearance of feces and urine, are necessarily recorded.
To identify hidden and atypical forms of hepatitis A in the identified location of the spread of the disease, it is recommended that everyone take blood samples for research. To carry out this analysis, capillary blood is used, in which ALT activity and a specific marker - anti-HAV IgM class are determined.
To effectively identify all sick people, such tests should be carried out at least once every 10-15 days. This procedure allows us to identify all sick people in the early stages and prevent the spread of the virus.