Hepatitis C is an anthroponotic infectious liver disease of an acute or chronic nature caused by the hepatitis C virus.
According to the World Health Organization, there are currently 130–150 million people (according to other sources – up to 200 million) infected with the hepatitis C virus (HCV, Hepatitis C Virus). The annual mortality rate for this disease and associated pathologies is approximately 700,000 cases.
Consequences of hepatitis C
After the determination of the viral nature of hepatitis in the 70s of the 20th century and the isolation of pathogens of types A and B, the question arose about the classification of other hepatitis, the presence of which was confirmed, but it was not possible to identify the type of virus. The name “non-A, non-B hepatitis” (NANBH) has been proposed for such diseases. Only in 1994 was the presence of the hepatitis C virus, which provokes the corresponding disease, reliably confirmed (hepatitis D and E are also designated hereinafter). At the same time, mandatory screening of donor blood for the presence of antibodies to HCV was introduced.
There is no specific immunoprophylaxis (vaccination) for hepatitis C due to the high variability of the virus.
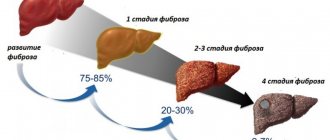
The acute disease is often asymptomatic and resolves spontaneously within 3–6 months in 15–35% of infected individuals, even in the absence of specific treatment. The remaining 45–85% of patients who have had acute hepatitis C experience a chronic inflammatory process, which in approximately a third of cases is complicated by cirrhosis or liver cancer.
The main features of this type of hepatitis, which determine its severity, are:
- high percentage of disease chronicity;
- life-threatening long-term consequences (cirrhosis and liver cancer);
- lack of effective etiotropic (aimed at destroying the pathogen) treatment;
- impossibility of effective immunization due to the high mutability of the virus.
Synonyms: viral hepatitis C.
Causes and risk factors
The causative agent of hepatitis C is an RNA virus of the Flaviviridae family, which has at least 6 genetic types and about 90 subtypes, which are widespread in different regions and determine the severity of the disease.
Subtype 1a predominates in Northern Europe and America, 1b – in Japan, Southern and Eastern Europe, Asia; subtypes 2a and 2b are most widespread in Europe, North America, and Japan; type 3 is widely represented in Southeast Asia and the Indo-Pakistan region. Subtype 3a ranks second in frequency in developed countries; As a rule, people under 20 years of age who use injecting drugs are infected with it. Genotypes 4 and 5 are most common in African countries.
In Russia, genotype 1 and subtypes 2a and 3a are more common.
The only source of infection is a sick person. The main route of transmission of the virus is parenteral:
- transfusion of infected blood and its preparations;
- therapeutic, diagnostic and cosmetic (aesthetic) manipulations in conditions of non-sterility (if the instruments are contaminated with infected blood);
- injecting drugs with the same needle together with a carrier of the hepatitis C virus (according to statistics, every second injection drug addict is infected with HCV).
In addition to the parenteral route of infection, vertical transmission of HCV from a sick mother to a child during pregnancy and infection through unprotected sexual contact are possible. These methods of infection account for no more than 10–14% of cases in total.
Methods of transmission of hepatitis C
You cannot become infected with hepatitis C:
- when using some household appliances (with the exception of razors, manicures and other accessories that may contain traces of blood);
- when shaking hands, hugging;
- when kissing;
- when eating together.
Main risk factors:
- donor blood transfusion;
- performing tattooing, manicure, injection procedures, dental procedures in unreliable institutions;
- unprotected sex with a casual partner;
- joint injection of drugs;
- professional contact with blood (we are talking about medical workers, military personnel, emergency services personnel).
Other possible threats
Your risk of developing a liver C infection increases if you:
- After blood transfusion or organ transplant before 1992. Since 1992, all blood and organ donors have been screened for liver disease C.
- Have been exposed to unsafe injection practices such as needle recycling. This is happening in some developing countries.
- It is necessary to have your blood filtered by a machine (hemodialysis) because your kidneys cannot filter your blood.
- Being born to a mother with liver disease C. The risk of passing the infection to the baby is higher if the mother is also infected with HIV.
- Ever injected or inhaled illegal drugs.
- You have HIV.
- Laryngeal concentrates for blood clotting before 1987.
- Born from a woman with hepatitis C infection.
- We were in prison.
- People born between 1945 and 1965 are 5 times more likely to become infected with hepatitis C than people born in other years.
The risk of getting hepatitis C through sexual contact is very small. The risk is higher if you are sexually promiscuous.
Complications
Virus C liver disease that continues for several years can cause significant complications, such as:
- Scarring of the liver (cirrhosis). Cirrhosis can occur within 20 to 30 years of liver C virus infection. Scarring in the liver makes it difficult for the liver to function.
- Liver cancer. A small number of people with liver C infection may develop liver cancer.
- Liver failure. Advanced cirrhosis can cause your liver to stop functioning.
Good luck! Good weekend! We wish you not to get sick!
Chronic hepatitis
– an inflammatory disease characterized by fibrotic and necrotic changes in liver tissue and cells without disruption of the structure of the lobules and signs of portal hypertension. In most cases, patients complain of discomfort in the right hypochondrium, nausea, vomiting, loss of appetite and stool, weakness, decreased performance, weight loss, jaundice, and itchy skin. Diagnostic measures include conducting a biochemical blood test, ultrasound of the abdominal organs, and liver biopsy. Therapy is aimed at neutralizing the cause of the pathology, improving the patient's condition and achieving stable remission.
Forms of the disease
The main forms of viral hepatitis C:
- acute (manifest icteric, manifest anicteric, subclinical);
- HCV past infection (acute outcome, recovery);
- chronic HCV [latent (inapparent or subclinical), manifest].
Outcomes of chronic hepatitis C:
- HCV cirrhosis of the liver (compensated or decompensated);
- hepatocellular carcinoma.
Chronic hepatitis C leads to liver cirrhosis and hepatocellular carcinoma
Depending on the severity, hepatitis C is:
- light;
- moderate severity;
- heavy;
- fulminant (severe malignant).
Classification of chronic hepatitis
By origin:
- chronic viral hepatitis (B, C, delta);
- autoimmune chronic hepatitis;
- drug-induced;
- alcoholic liver disease;
- cryptogenic (reason unknown).
By activity:
- minimum;
- mild;
- moderate;
- expressed.
According to the stage of fibrosis (connective tissue degeneration) of the liver:
- absent;
- mild;
- moderate;
- expressed.
Symptoms
The incubation period of the disease lasts from 1.5 to 6 months (on average 2–3).
Acute hepatitis C is characterized by a benign course, the condition quickly normalizes, the manifestations of the disease are mild or moderate:
- unexpressed dyspeptic symptoms (1-2 times vomiting, heaviness or dull arching pain in the right hypochondrium, unstable stool, nausea, loss of appetite, feeling of bitterness in the mouth);
- a rise in body temperature to subfebrile levels (noted by about a third of patients), high fever is uncharacteristic;
- liver enlargement;
- icteric staining of the skin and visible mucous membranes, icterus of the sclera;
- dark coloration of urine, discoloration of feces.
It is characteristic that the severity of the disease in acute hepatitis C is less pronounced than in other forms of viral hepatitis.
Yellowness of the sclera in a patient with hepatitis C
Recovery from an acute process occurs in 15–35% of infected individuals; in other cases, the disease becomes chronic and continues for many years and even decades.
Most often (in approximately 70% of cases), there are no symptoms of either acute or (subsequently) chronic hepatitis for many years; the infected person is bothered by increased fatigue, periodic heaviness in the right hypochondrium, and intolerance to intense physical activity. In this case, carriage of the virus is determined by chance during preventive examinations, during hospitalization or an attempt to donate blood as a donor.
Causes
If the inflammation in the liver has become chronic and lasts for at least 6 months, then suspicion falls on hepatitis of unknown etiology. This diagnosis means that the cause of development is unclear, and the exact disease cannot be determined under these conditions. In another way, such hepatitis is called “cryptogenic”.
There are a number of reasons that can provoke the appearance of such hepatitis:
- Use of medications. Many potent drugs negatively affect internal organs, especially the liver, which can cause the disease. However, the drugs must be taken for quite a long time for the liver to be damaged.
- Alcohol abuse. The body perceives ethyl alcohol as poison, so when alcohol enters the bloodstream, the liver begins to produce neutralizing enzymes. If you drink frequently, the organ will wear out.
- Poor nutrition. The liver responds by producing bile, which breaks down food in the intestines. A person who prefers to eat heavy and unhealthy foods (fried food, fast food) prevents the liver from removing all toxins from the body, which subsequently leads to inflammation.
- Hepatitis virus. The pathogen can be difficult to identify, but symptoms and inflammatory processes in the liver are already beginning.
- Other viruses (eg, Epstein-Barr pathogen or herpes). They weaken the body's defenses.
- Autoimmune diseases. In this case, the patient’s body fights with its own cells, so the immune system is weakened and the liver is destroyed.
Weak immunity
In case of cryptogenic hepatitis, the patient is registered and constantly monitored. Even before determining the exact diagnosis, the doctor prescribes therapy so as not to delay the start of treatment. Statistics show that in 40% of patients this hepatitis was never attributed to a specific etiological factor.
Diagnostics
The diagnosis is made based on:
- the presence of epidemiological data on the possible method of infection - the so-called starting point (it is typical that in approximately half of those infected the cause of the disease cannot be identified);
- the presence of specific clinical manifestations (in the icteric form of the disease);
- determination of IgM and IgG to HCV;
- detection of HCV RNA (HCV-RNA) by polymerase chain reaction;
- changes in biochemical blood test [increased levels of liver enzymes (ALT, AST), hyperbilirubinemia];
- positive thymol test.
To detect the hepatitis C virus, you need to take a blood test
Is infection possible during prophylaxis and the use of drugs?
The measures taken are aimed at preventing the spread of infection among the population. If all requirements are strictly followed, the risk of spreading the infectious process is minimized.
However, it should be noted that compliance with all recommended rules does not guarantee complete protection against pathogen penetration into the body. Therefore, it is recommended to periodically examine the body for the presence of antibodies to the pathogen for timely detection of the pathological process, as well as taking adequate measures aimed at stopping the negative consequences of infection.
One of the most effective preventive measures is currently considered to be the use of special vaccinations against hepatitis A and B. The use of the vaccine allows for liver protection and immune support. There is currently no specific vaccine against hepatitis C.
Some institutes located abroad and dealing with the problem of combating viral infections have developed drugs against viral hepatitis C, but they are at the testing stage and currently do not have clinical confirmation of their effectiveness in combating the infectious disease.
Dystrophic liver damage, inflammatory in nature, characterized by a long course.
Causes of chronic hepatitis
The cause of the development of the chronic form of hepatitis, in half of all cases, is improper treatment of acute viral hepatitis, most often hepatitis C. At risk are people who have alcohol and drug addiction, people who have been taking medications for a long time, for example, antibiotics, cytostatics, anti-tuberculosis drugs. Negative effects of toxic substances, autoimmune processes, metabolic disorders, all this can also affect the development of the pathological process.
Symptoms of chronic hepatitis
The patient has an increase in the size of the liver; upon palpation, it is clearly palpable. A dull pain occurs in the liver area, bradycardia occurs, the general psychological state worsens, and the person becomes irritable. Insomnia, nausea, indigestion, belching, flatulence, increased fatigue, decreased appetite, the appearance of dilated capillaries on the face, the appearance of the characteristic sign “liver palms”, nosebleeds, pain in muscles and joints occur.
Diagnosis of chronic hepatitis
An analysis of the patient's medical history and life is carried out; in order to make a diagnosis, the following is performed: a biochemical blood test, a liver biopsy, a blood test to determine antibodies to hepatitis viruses, virological and immunological studies.
Treatment of chronic hepatitis
The patient should follow a strict diet (table No. 5), exclude alcohol, coffee drinks and tea, reduce physical activity as much as possible, and have enough time to rest. During drug therapy, the patient is prescribed immunomodulators, antiviral drugs (interferon-α, lamivudine), hepatoprotectors (Essentiale, Hepabene, Heptal). There is a high probability of developing complications, especially with incorrect treatment, such as: liver cirrhosis, hepatocellular carcinoma.
Treatment
The main goals of treatment are to prevent complications from developing and to slow or stop progression. For this purpose the following are assigned:
- direct acting antivirals (DAAs);
- interferons (including PEG-interferon);
- immunomodulators;
- hepatoprotectors;
- detoxification therapy;
- desensitizing agents;
- vitamin therapy;
- enzyme preparations.
Treatment of hepatitis C is complex using immunomodulators and interferons
According to some data, complex pharmacotherapy of acute hepatitis C using DAAs and PEG-interferon for 6 months led to the cure of patients in 98% of cases and excluded the transformation of the disease into a chronic form.
Possible complications of the disease
The most common complications of chronic hepatitis are cirrhosis (replacement of normal liver tissue with connective tissue) and cancer, namely hepatocellular carcinoma, which is considered an extremely malignant and rapidly progressive neoplasm. Moreover, the development of the consequences of the disease directly depends on the etiological factor that provoked it. The above pathologies in 70-80% of cases occur against the background of type B and C viral infections.
In a third of patients, the course of the disease ends with organ failure and toxic hepatic encephalopathy, which, if they seek medical help late, lead to coma.
Without proper therapy, hepatitis B will cause many negative consequences. Typically, patients are faced with cirrhosis of the liver, which entails the death of liver cells and replacement of scar tissue. Large and small nodes gradually form from it, changing the structure of the organ.
Pathological processes in cells during hepatitis disease provoke liver failure, a symptom complex that combines changes in basic functions. The disease is often accompanied by: accumulation of fluid in the abdominal cavity, inflammation of the peritoneum (peritonitis), hepatic colopathy (impaired functioning of the large intestine due to problems with the liver and blood supply), infertility.
Manifestations of gastric or intestinal bleeding (blackening of stool, low blood pressure, vomiting blood, increased heart rate) indicate varicose veins located in the esophagus. Some patients experience confusion and hepatic encephalopathy.
Peritonitis
Patients diagnosed with liver cirrhosis suffer from hepatorenal and hepatopulmonary syndromes. There is a high risk of developing malignant tumors, including hepatocellular carcinoma.
The positive outcome of therapy for chronic viral hepatitis B depends on various factors: the advanced stage of the disease, the age and lifestyle of the patient, concomitant pathologies, and individual characteristics of the body. With proper implementation of medical recommendations, the chances of achieving stable remission are very high. To prevent the disease from returning, you need to follow a diet and periodically take a course of hepatoprotectors to maintain the liver.
Most often, chronic hepatitis B has a generally favorable course, with no obvious signs of liver damage. Slow progression of the disease reduces the likelihood of cirrhosis to 10%.
Actively progressing disease with the threat of cirrhosis is less common, but in this case the risk is higher - from 20%. One in ten patients is diagnosed with primary liver cancer.
Further evidence in favor of quitting alcohol: Ethanol abuse increases the likelihood that a person will suffer from severe consequences of hepatitis.
With timely treatment of hepatitis, even before it enters the chronic stage, doctors often give patients a good prognosis. But if the viral pathology is ignored, the patient may face irreversible consequences such as liver cancer or cirrhosis within a few months.
In addition, during the period of exacerbation, the disease also causes serious harm to the body, causing disruptions in many of its systems, including the immune system. And this, in turn, makes a person an easy target for other diseases, including non-viral ones.
Forecast
In 25–35% of patients diagnosed with chronic hepatitis C, between 10 and 40 years, connective tissue degeneration of liver tissue (cirrhosis) occurs, with possible death. In 30–40% of patients with a chronic form of the disease, liver cirrhosis will eventually undergo malignant degeneration.
According to the World Health Organization, there are currently 130–150 million people (according to other sources – up to 200 million) infected with the hepatitis C virus (HCV, Hepatitis C Virus).
If hepatitis C virus RNA remains in the blood of an infected person for more than 6 months, spontaneous resolution of the HCV infection is extremely unlikely.
How to determine the cause of the disease?
The doctor's verdict often comes as a surprise. And many do not quite understand what hepatitis of unknown origin is. This means that moderate or severe inflammation in the liver has been detected, but doctors themselves cannot understand why it arose.
According to statistics, the most common causes include alcohol consumption, long-term use of medications, and viral infections. But quite often it happens that the patient leads a healthy lifestyle, does not drink, does not smoke, and is diagnosed with a disease.
At the initial stage, it is easier to cure the disease. If the inflammatory reaction is sluggish and lasts a long time, then it transforms into a chronic form. Thus, idiopathic hepatitis is diagnosed when the disease is “older” than 6 months.
The absence of antibodies in the patient’s blood helps differentiate hepatitis of unknown origin from other liver pathologies. They are always found in biliary cirrhosis or an autoimmune form of inflammation.
Prevention
There is no specific immunoprophylaxis (vaccination) for hepatitis C due to the high variability of the virus.
Basic preventive measures:
- compliance with personal hygiene measures;
- hand treatment and use of gloves when working with blood;
- refusal of casual unprotected sexual relations;
- refusal to take narcotic drugs;
- receiving medical and cosmetology services in official licensed institutions;
- Carrying out regular preventive examinations in case of possible professional contact with blood.
Video from YouTube on the topic of the article:
Methods for treating hepatitis of unknown origin
When the causes of the disease are unknown, doctors prescribe a therapeutic regimen that is typical for any inflammatory and destructive pathologies of the liver. The goals of therapy are to prevent intoxication, improve the functionality of the gland, and support the immune system.
Additionally, it is recommended to use medications to normalize the functioning of the digestive tract. Simultaneously with treatment, other diagnostic methods are prescribed to ensure the effectiveness of the prescribed regimen.