What is encopresis and who is most likely to experience it?
Fecal incontinence is experienced mainly by people over the age of 50. Moreover, most of them are men. With this disease, the coordinated work of the sphincter and pelvic floor muscles is disrupted. The interaction of these systems normally prevents spontaneous bowel movement. The autonomic nervous system is responsible for the proper functioning of the muscles in this area.
During normal bowel movements, irritation of the mechanoreceptors in the rectum occurs, a urge to assume a comfortable position appears, followed by contraction of the muscles of the anterior abdominal wall, puborectal and anal sphincter. In people with encopresis, there is a failure at one of these stages, and emptying occurs spontaneously.
Mechanism and reasons for the development of encopresis
Before considering the causes of fecal incontinence, it is necessary to consider the mechanism by which this disease develops. In turn, knowledge of the mechanism will allow us to accurately characterize the reasons why encopresis progresses further.
The physiological mechanism of defecation is based on the coordinated work of the human nervous and muscular systems - the rectum contains a large number of nerve endings and muscles that are responsible for retaining or expelling feces. The sphincter is of key importance in the process of defecation. It has been established that normal pressure in the sphincter area is 50-120 mm. Hg Art., and the average value is about 80 mm. Hg Art. This indicator is higher in men than in women, and therefore, with a significant change in pressure, a number of pathologies may appear, including fecal incontinence.
The sphincter is in a state of constant tone, which is maintained by the smooth muscles inside the rectum, as well as by the autonomic nervous system - which is why it is impossible to consciously control or control this muscle.
The physiologically normal process of defecation occurs as a result of an irritating effect on the mechanoreceptors of feces, which accumulates in the ampulla after passing through the sigmoid colon. Next, the Valsalva reflex comes into play, in which simultaneous tension of the abdominal wall and glottis is observed. As a result of this reflex, the pressure in the abdominal cavity increases significantly, which, in turn, causes segmental contractions in the intestines and, as a result, the release of feces. At the same time, the muscles of the pelvic floor relax and it lowers, which allows feces to pass out of the body more easily.
Causes of fecal incontinence
Above we looked at the physiological process of defecation and how it occurs normally. Accordingly, the cause of disturbances in the fecal eruption process may be hidden behind a violation of one or more phases preceding the process itself. Let's take a closer look at the main causes of fecal incontinence:
- Physiological and functional disorders. This category includes such phenomena as constipation (70-80% of all cases of fecal incontinence), muscle weakness or damage resulting from mechanical or organic trauma to the anus, pathology of the nervous system, hemorrhoids, functional disorder of muscle tissue, in particular pelvic floor and rectal areas.
- Neurological and psychophysiological disorders. In some cases, fecal incontinence can be triggered by a problem of a neurotic nature - this could be severe fear, stress or other psychological trauma, which, in turn, provoked disorders of the nervous system. Since nervous regulation also takes part in the physiological process of feces, disruption of its functioning or the development of pathologies can also provoke the development of encopresis.
Among other reasons, it is also worth noting colectomy (intestinal surgery), decreased sensation of bowel movement, as well as diseases of various natures, in which encopresis is one of the symptoms of the clinical picture.
Fecal incontinence as a concomitant symptom
We noted above that encopresis may not be an independent disease, but a symptom that accompanies other ailments. In particular, fecal incontinence can occur as a result of hemorrhagic or ischemic stroke, due to disruption of nervous regulation and pathology of the higher nervous system, as well as dysfunction of the pelvic floor organs. In the latter case, fecal incontinence acts as a concomitant symptom of Alzheimer's disease, multiple sclerosis, encephalitis, various defects of the genitourinary system, tumors and neoplasms, uterine prolapse, prostatitis and other diseases.
Types of fecal incontinence
In medicine, there are several types of encopresis. They are classified based on the characteristics of the defecation process. Incontinence happens:
- Regular. With it, the patient does not have the urge to defecate. As a rule, this disorder is observed in elderly bedridden patients.
- With a feeling of an urge to defecate, but with the inability to delay this process.
- Partial. In this case, incontinence occurs under certain stresses (coughing, sneezing, lifting heavy objects, fear). Encopresis in this case is accompanied by joint emptying of the bladder.
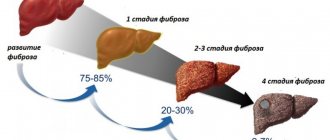
With age, degenerative processes occur in the human body, which increase the risk of encopresis.
It develops gradually, moving from one stage to another. First, a person experiences incontinence of gases, then loose stools, and only then a complete inability to control the process of defecation and gas formation.
The risks of incontinence increase with age
The doctor will be able to choose the appropriate treatment by determining the causes and type of fecal incontinence.
Regularity
Normally, the average person should defecate up to 2 times a day. However, it should not be accompanied by painful or other uncomfortable sensations. In addition, a person should not make any significant effort when straining.
The interval between acts of defecation is a purely individual indicator. For the average person, bowel movements occur in the morning. At the same time, the possibility of cleansing in the evening cannot be ruled out.
Normally, up to 0.5 kg of feces should leave the body per day. Feces should be released easily, sink immediately and not leave marks on the plumbing. The color of stool is normally brown (except on days when a person has eaten a coloring food, such as beets). The consistency of the feces should be soft but formed stool.
Causes of fecal incontinence in women
The causes of encopresis can be congenital or acquired. The first include:
- anatomical features or diseases of the rectum;
- pathologies of the anal apparatus.
The reasons for the development of an acquired disease include:
- Previous rectal surgery, hemorrhoid removal, enterocele repair, or cancer treatment.
- Psychological factors (schizophrenia, hysteria, panic, unstable psyche, dementia).
- Postpartum period.
- Injuries to the brain, pelvis or abnormalities associated with a tumor.
- Diarrhea that occurs due to infectious diseases.
- Damage to the intestinal obturator apparatus.
- Alcoholism.
- Epilepsy.
- Catatonic syndrome.
At the first suspicion of fecal incontinence, you should contact a proctologist or neurologist.
Only a specialist can determine the true causes of fecal incontinence.
Komy-za30.ru also notes that in women, the tone of the pelvic muscles and sphincter is regulated by hormones. Therefore, the onset of menopause can also cause the development of encopresis.
Causes of encopresis in men
Unlike women, older men are more likely to experience encopresis. The average sphincter pressure in the stronger sex can reach up to 125 mm/Hg/st. Moreover, the tension is constant even in sleep. The causes of encopresis in older men are as follows:
- Chronic constipation.
- Rectal cancer.
- Obesity.
- Excessive use of laxative medications.
- Previous coelenterate operations.
- Poor sensitivity of the rectal area.
- Terminal stage of hemorrhoids.
- Psychological factors (state of stress, depression, fear, etc.).
- Congenital anomalies of the pelvis.
- Prolonged diarrhea.
- Degradation of the nervous system.
- Multiple sclerosis.
- Parkinson's or Alzheimer's disease.
Men who have suffered a stroke or brain injury also face the problem of encopresis.
How is it diagnosed?
When diagnosing encopresis, the doctor interviews the patient. Knowledge of the characteristics of the course of the disease will help the specialist more accurately determine the type of disorder and prescribe individual treatment. To do this, the doctor may ask the patient the following details about the sensitive problem:
- factors under which defecation occurs;
- duration and frequency of incontinence;
- presence of urge to have a bowel movement;
- stool consistency;
- volume of stool and presence of gases.
At the appointment, the doctor will examine and interview the patient
The development of encopresis can also be influenced by psychological factors or brain damage. Therefore, the doctor will definitely ask the patient about recent emotional turmoil, head injuries, confusion or disorientation in space. The specialist must also know everything about the patient’s diet, bad habits, medications and lifestyle.
The next stage of diagnosis will be instrumental studies. These include:
- anorectal manometry to determine the sensitivity and contractility of the anal sphincter;
- endorectal sonography, which allows to identify sphincter defects, their tone or pressure in the anal canal;
- MRI of soft tissues of the pelvic area;
- defectography aimed at identifying the volume of feces held back by the intestines and the characteristics of the process of its emptying;
- electromyography, which reveals malfunctions in the nervous system;
- sigmoidoscopy and ultrasound of the rectum, calculating anatomical features or pathological neoplasms in this part of the intestine.
The range of diagnostic measures also includes blood, urine and stool tests. This information is sufficient to prescribe treatment for a patient with encopresis.
First of all, therapy will be aimed at eliminating concomitant pathologies or factors that caused this disorder.
Some important numbers
The amount of stool that will make you want to go to the toilet: from 25 milliliters and above. This indicator is usually called the threshold of rectal sensitivity.
But your internal anal sphincter can relax even if 10 milliliters of feces press on it.
A constant urge to defecate will occur if there is at least 220 milliliters of contents in your intestines.
But your intestines can withstand amounts up to 280 milliliters. Although for some this threshold is slightly lower: from 110 ml.
If during anorectal manometry any deviations from the above norms are observed, then this is a sign of a pathological condition.
In addition, each person expels up to half a liter of gas during bowel movements. But in patients with flatulence - up to 3 liters or even more.
This gas mixture consists of 90% nitrogen, and the rest of its components are oxygen, hydrogen, carbon dioxide, ammonia, hydrogen sulfide, etc.
The desire to visit the toilet arises at the moment when feces from the sigmoid colon pass into the rectum.
A person can consciously control this process starting from one and a half to two years. It is worth mentioning that depending on age, the normal frequency of bowel movements may vary.
An infant up to 3 months old, feeding only on breast milk, can defecate from 5 to 40 times a week; in artificial babies, this number is reduced to 20 times. A child under one year old can poop up to 28 times, up to 3 years old - up to 21 times. Children over 4 years old may have bowel movements from 3 to 14 times.
The most common and well-known postures for defecation are squatting and sitting. More often than not, the choice of position will depend on the type of toilet and mentality.
What to do first: lifestyle changes
Comprehensive treatment of fecal incontinence in the elderly always begins with changes in the patient's lifestyle. Before drug therapy, exercise therapy and dietary changes, to cope with the complexities of this disorder, the following tips will help the patient:
- Empty your bowels before each time you leave the house.
- It is better to leave the house 1-2 hours after eating.
- The patient's bag should always contain wet wipes and a change of underwear.
- It is recommended to replace regular underwear with disposable underwear.
- You should always plan your route outside the house in advance, inquiring about the location of the toilet rooms.
Also, to get rid of the unpleasant odor of gases or feces, you can purchase special medications at pharmacies.
How is fecal incontinence treated with medications?
Medicines are prescribed mainly to patients suffering from fecal incontinence due to diarrhea. Drugs of 3 groups can be used:
- Anticholinergic. They contain atropine and belladonna, which slow down peristalsis and reduce intestinal secretion.
- With opium derivatives (Codeine, anesthetics, Diphenoxylate, Lomotil, Atropine). They improve the tone of the rectal muscles, reduce peristalsis and block pain.
- Absorbent (Kaopectan, Metamucil, Polysorb, etc.). They reduce the amount of water in the stool.
The specialist will prescribe medications suitable for each individual case of encopresis.
More classic remedies in tablets, suppositories and injections (Loperamide, Imodium, Furazolidone, Proserin, Strychin) also help treat diarrhea. B vitamins or ATP may also be included in therapy.
If you have encopresis, you should not take antacids or medications that cause diarrhea.
If incontinence appears during the development of psychological problems, the patient is prescribed sedatives or tranquilizers, which are dispensed upon presentation of a prescription.
Nutrition
Diet is the basis of encopresis therapy. Without it, treatment of the disease will be ineffective. Proper nutrition allows you to normalize stool, eliminating constipation and diarrhea, reduce the volume of feces, and also normalize intestinal motility.
The diet for encopresis is based on the following rules:
- Products that soften stool (sweeteners, dairy products, nutmeg, alcohol, coffee, ice cream) are excluded from the patient’s diet.
- The consumption of hot spices, lard, fatty meats, citrus fruits, carbonated drinks and smoked foods should be minimized.
- I'll have to give up smoking.
- The basis of nutrition should include cereals, fresh vegetables and fruits, whole grain bread, wholemeal products, fermented milk drinks without additives, wheat flakes, bran.
With this diet, you should eat 5-6 times a day in small portions, keeping equal intervals between meals. Don't forget about maintaining water balance. You should drink at least 2 liters of water per day.
The patient needs to keep a food diary, which records information about the time of meals and the foods consumed. It also includes each case of incontinence. Thanks to this information, the doctor will be able to accurately identify foods that irritate the intestines and identify deficiencies in the patient’s diet.
Treatment methods
It is based on certain principles:
- adjustment of regime and diet;
- medicines;
- training the muscles of the intestinal systems;
- stimulation of work using electrical equipment;
- operational activities.
Each principle will be analyzed by a specialist. Treatment of encopresis is aimed at eliminating the problem - the cause that caused the disruption of the bowel movement.
Medicines
Among medications that help normalize the functioning of the digestive system, Imodium tablets are considered one of the most popular. In medical language they are called Loperamide.
Drug groups:
- antacids;
- laxatives;
- therapeutic.
Other anti-diarrhea drugs intervene in the disease and produce additional healing effects:
- Atropine, Belladonna. Anticholinergic drugs, they reduce the development of secretion and increase peristalsis. Motility of the intestinal walls returns to normal. Can be used at various stages.
- Codeine. The drug relieves pain, as it is one of the derivatives of the opium group of drugs. More often it happens that it is included in the group of dangerous contraindications. Prescribed only on the recommendations of a doctor.
- Lomotil. A medicine with this name reduces the movement of feces and creates conditions for its hardening.
The most common are activated carbon tablets. The substance is named after the active element of its composition. Coal absorbs liquid and expands feces in volume. In addition, the medicine removes toxic substances from the body.
Home treatments
The problem may arise when it is impossible to go to a medical facility.
Then you have to turn to the advice of healers, healers from the people. At home, the disease has been eliminated for many centuries. Treatment of fecal incontinence was carried out in villages, where grandmothers selected medicinal herbs and created miraculous tinctures. You can use folk remedies, but such an action should not be permanent. What reasons led to loose stools, what caused intestinal malfunctions? Answers to questions can be obtained after a full examination and diagnostic procedure.
- Enemas. Chamomile decoctions are used to carry them out. Take 50 g of medicinal herb and place it in a liter of boiling water. Over low heat, wait for the chamomile components to completely dissolve. Then cool to room temperature and insert into the rectum. You need to hold the medicine inside for a very long time, you can help with the help of medical devices or hands.
- Infusions for internal use. The base is calamus grass. It is steamed in boiling water, the proportions are 20 g of herb, 200 ml of liquid. You can’t make a lot of water compositions. A liter of healing infusion is sufficient for a course of 7 days. Drink 1 spoon after meals.
- Rowan juice. The fruits of the tree help when eaten fresh and pressed into a drink. Dosage rate: one spoon no more than 3 times a day.
- Honey products. Honey, 1 tablespoon per day, will be both a therapeutic and preventive method of eliminating the disease.
Exercise therapy: exercises for fecal incontinence in women
Kegel exercises can help strengthen the pelvic floor muscles and prevent fecal incontinence in women. These include:
- squeezing and relaxing the anal sphincter 50-100 times a day;
- retraction and protrusion of the abdomen 50-80 times a day;
- tension of the pelvic muscles in a sitting position with legs crossed inward and upward.
You can perform these exercises either by holding the tension for 5-15 seconds, or with accelerated alternation of positions. In this case, breaks between approaches should last 5-7 seconds.
Exercises to strengthen muscles for urinary and fecal incontinence
At first, when performing a set of exercises, the patient may need sensors connected to the body and recording the work of certain muscles. The devices make it possible to identify violations during gymnastics, helping the patient correct his mistakes.
Patients experiencing encopresis after a stroke are advised not only to perform Kegel exercises, but also to pay attention to the development of fine motor skills. To do this, you can squeeze or roll special balls in your palms, do modeling, assemble puzzles or put together a mosaic.
Such exercises will allow the patient to quickly establish neural connections and get rid of the inconveniences that arose after a stroke.
Only regular performance of a set of exercises allows patients with encopresis to achieve visible progress in treating the disorder. As a rule, the result is consolidated after 3-6 months of daily training.
Treatment methods for female diseases
Your doctor will tell you what to do to eliminate unpleasant symptoms.
The methods were developed by specialists based on the experience of doctors in studying the causes of fecal incontinence.
- Operations to introduce a special gel into the canal. This type of therapy is used to strengthen the walls of the anus. The method does not promise a complete cure; relapse may occur.
- Fixation of internal organs. Operations are rarely used. Surgeons secure the fluid emission channel, cervix, and bladder. After the intervention, a long recovery period will be required.
- Loop method. One of the most frequently performed methods of surgical intervention. To eliminate urinary and fecal incontinence, a support is created from a loop of special medical material.
Treatment after injury to the sphincter region or damage to the pelvic muscle tissue consists of the method of modern technologies - sphincteroplasty. The surgeon stitches torn, stretched muscles. Another way is an artificial organ, which can be controlled by the person himself. The surgical cuff is inflated and deflated. Fecal incontinence after surgery can be hidden by simple measures: clean, changeable clothes, taking medications that reduce the smell of stool accompanied by gases.
Psychotherapy
If the cause of encopresis lies in psychological pathologies, then psychotherapy is included in the complex of treatment measures. The purpose of these visits is to train and establish a conditioned reflex to the situation, events or place in which defecation will take place. In addition, the patient is recommended to follow a routine of going to the toilet after eating or waking up.
Psychotherapy also allows you to keep under control the psychological diseases that caused the development of encopresis.
Surgical intervention
In rare cases, when the above treatment for fecal incontinence in older women and men does not help, the patient may undergo surgery. It gives tangible results in cases where the causes of encopresis were previous operations, malignant neoplasms or the postpartum period in women.
To eliminate this problem in the elderly, the following is used:
- sphincteroplasty aimed at reconstructing the sphincter;
- “direct sphincter”, in which the sphincter muscles are positioned more tightly to the anus;
- installation of an artificial sphincter, which allows you to control the process of defecation using a cuff that covers the anus and a pump that supplies air to the cuff;
- colostomy, during which the large intestine is cut off and brought to the anterior abdominal wall, which allows stool to be collected in a special bag (colostomy).
Special sanitary pads
It is worth noting again that surgery is a last resort for treating encopresis. You will not be able to sign up for such an operation on your own. It can only be prescribed by the attending physician, based on the causes of the disease and the characteristics of its course.
Diagnosis of incontinence
The doctor diagnoses fecal incontinence by studying the patient's medical history, conducting a complete examination and the necessary diagnostic tests. Diagnostics helps to correctly determine treatment tactics. For patients who have problems with stool incontinence, the doctor asks the following questions:
- How long has the patient been incontinent?
- How often does the patient experience incontinence, and at what time of day?
- Do you pass a lot of feces: is it large amounts of stool or just dirty laundry? What is the consistency of spontaneously passed stool?
- Does the patient feel the desire to have a bowel movement, or is there no urge?
- Do you have hemorrhoids, and if so, do they fall out?
- How has the quality of life changed with the advent of spontaneous fecal excretion?
- Has the patient observed a connection between the consumption of certain foods and incontinence?
- Does the patient have control over the release of gases from the intestines?
Examination of the patient
Based on the answers of the patient with incontinence, the doctor makes a referral to a specific specialist, for example, a proctologist, gastroenterologist or rectal surgeon. The specialized doctor conducts an additional examination of the patient and prescribes one or more studies from the following list:
- Anorectal manometry. The examination is carried out using a mechanically sensitive tube. This allows you to determine intestinal function and sensitivity of the rectum. Manometry also reveals the ability of the sphincter muscle fibers to contract to the desired level and respond to nerve impulses;
- MRI - this examination uses electromagnetic waves to obtain detailed visualization of the patient's internal organs without the use of x-rays. Tomography allows you to examine the sphincter muscles;
- Rectal ultrasound. Ultrasound examination of the lower intestine and anus is carried out using a probe inserted through the anus. This device is called a "transducer". The ultrasound procedure does not pose a health hazard and is not accompanied by pain. It is used to study the condition of the patient's sphincters and anus;
- Proctography is an examination of the patient using an X-ray machine, demonstrating the amount of feces that can be retained in the intestines, the distribution of feces in it, as well as the effectiveness of the act of defecation;
- Sigmoidoscopy. During this examination, an elastic tube with a hole is passed through the anus into the rectum and into the following lower parts of the patient's large intestine. With its help, the intestines are examined from the inside to detect probable causes of incontinence: scars, inflamed lesions, tumor growths;
- Electrical myography of the muscular system of the pelvic floor and intestinal muscles, which helps determine the correct functioning of the nerves that control these muscles.
What gaskets to use
If earlier encopresis meant constant wearing of diapers, today these products have been replaced by specialized pads with a ureteral catheter. They are conveniently fixed and placed in shorts, which makes life much easier for older people. Also, the positive features of such gaskets include:
- absorption of unpleasant odors using an absorbent layer;
- preventing the proliferation of pathogenic microorganisms due to the antibacterial layer;
- hypoallergenic due to the absence of latex;
- breathability due to the “breathable” component.
Gaskets will help avoid awkward situations
In pharmacies you can find Seni V brand products from a Polish manufacturer. Encopresis is always accompanied by urinary incontinence. Regular diapers are not able to cope with two problems at the same time. Therefore, pad manufacturers advise placing their inserts in a diaper, thereby providing reliable protection from awkward situations. Products of this brand with a catheter are used separately from diapers, facilitating the patient’s movements.
Read more about the treatment of urinary incontinence in adults >>
Products come in two sizes - maxi and normal. They differ in the volume of absorbent surface. The principle of putting them on is similar to regular diapers. But when using them, it is necessary to provide the presence of fixing panties or a urinary catheter.
These products also have their drawbacks. The pads do not have an insulating layer that prevents moisture from reaching the extremities.
Prognosis for encopresis in adults
If encopresis is an independent disease, and not a consequence of other diseases, then with timely treatment and compliance with all doctor’s recommendations, patients manage to recover quite quickly.
But, unfortunately, if the causes of fecal incontinence in adults are hemorrhagic or ischemic stroke, oncology, mental disorders or spinal injury, then the prognosis is likely to be unfavorable, and encopresis is unlikely to be cured.
Fecal incontinence in older adults can be a barrier to a comfortable life and self-confidence. But, fortunately, today there are many ways to treat this problem, which are determined by the doctor after diagnosis.
Author: Nadezhda Putilova. The article was checked by an expert - practicing family doctor Elizaveta Anatolyevna Krizhanovskaya, 5 years of experience
Clinical description of the pathology and the principle of the defecation process
Fecal incontinence in adults is an unpleasant and dangerous phenomenon. A person loses the ability to control internal processes; bowel cleansing is not controlled by the brain.
Feces can be of different consistencies - solid and liquid. The emptying process itself does not change. Fecal incontinence in women is diagnosed less frequently than in the stronger half of humanity. Statistics give figures - one and a half times less. But this does not allow women to be calm and confident that they are not afraid of such a pathology. The disease is nearby, waits for favorable conditions and manifests itself, disrupting the usual way of life.
There is an opinion that the pathological disorder is characteristic of old age. Fecal incontinence in the elderly is an optional sign of age; doctors have proven that this opinion is wrong. Statistics provide figures that explain the emergence of such opinions. Half of the patients are people over 45 years of age. Age is only one of the reasons that leads to illness.
To understand why fecal incontinence occurs, you need to understand the process of managing bowel movements. Who controls at what level of physiology this is laid down. Several systems control the output of feces. Their coordination leads to the normal functioning of the body.
- The rectum contains a large number of nerve endings that are responsible for the functioning of muscle structures. The same cells are located in the anus. The muscles hold the feces and push them out.
- The rectum is located inside the intestine so as to hold feces and send it in the right direction. Feces, once in the rectum, already acquire their final state. It is dense, compressed into voluminous ribbons. The anus closes its exit without control.
- The compressed state of bowel movement is maintained until it is released, when the person is ready for the act of defecation and understands that it has occurred. In a normal state, a person can restrain the process until he can go to the toilet. The delay time can be hours.
The sphincter plays an important role in the process.
More precisely, the pressure in his area. Normally, it varies from 50 to 120 mmHg. For men, the norm is higher. The anal organ in a healthy state should be in good shape; a decrease in its functionality leads to worsening bowel movements. Its activity is controlled by the autonomic nervous system. It will not be possible to consciously influence the sphincter. Stimulation of fecal output occurs at the level of irritation of receptors in the walls of the rectum. Scientific explanation for passing stool:
- simultaneous vibration of the peritoneal muscles and closure of the main opening (slit passage);
- increased pressure on the sphincter;
- delayed compression of intestinal segments;
All processes lead to advancement, pushing feces towards the anus. The process is slow and cannot be accelerated. The pelvic muscles enter a relaxed state, the muscles open the rectal outlet. The internal and external sphincter relaxes. When a person cannot get into the sanitary room, he strains the internal receptors, the anorectal opening remains closed and tight. The degree of tissue tension stops the urge to go to the toilet.