The essence of the problem
The color of the skin is affected by the condition of the blood vessels: their narrowing or dilation gives the skin pallor and redness. In addition to melanin, the human body contains:
- carotene is a yellow pigment;
- hemoglobin in capillaries is red;
- hemoglobin in venules is blue.
Albinos, due to a genetic mutation, completely lack the enzyme that produces melanin. They are required to constantly use sunscreen.
Melanin protects the skin from the harmful effects of ultraviolet rays. Increased melanin production leads to hyperpigmentation, which results in brown patches of skin.
This phenomenon can occur when taking certain medications, as well as during pregnancy. If there is a lack of melanin, the skin becomes discolored in areas and hypopigmentation forms. This happens when pigment-producing cells (melocanites) are weakened or absent. White spots appear on the legs, arms, and facial skin. As a rule, they do not hurt and cause only aesthetic discomfort.
Hemorrhagic spots
Pigment spots - due to the fact that they are brown - are similar to hemorrhages that occur with vascular diseases, with pathology of the coagulation system:
- Thrombocytopenic purpura. Here the rash is not only located on the legs, it occurs spontaneously, after sleep, it is asymmetrical, both dark spots and purple and yellowish-green spots are visible (like the phases of a bruise).
- Hemorrhagic vasculitis. Here, brown spots appear immediately on the legs, symmetrically on both. The shape of the rashes is different, they tend to merge. The disease also affects the joints, the stomach may hurt, and the functioning of the kidneys and brain may be impaired. This pathology requires urgent medical correction. Read more about the symptoms and treatment of vasculitis.
What is vitiligo?
The most common cause of such white spots is vitiligo. At the very beginning they have a pinkish tint, and then acquire a milky white color. The sizes of the spots vary, the boundaries have clear outlines, large lesions can increase and merge. In rare cases, the white spots may become itchy. The skin in such places loses hair, the function of the sebaceous glands is disrupted, it becomes thin and loses its sensitivity. In some cases, the pathology may be accompanied by eye diseases associated with altered pigmentation. (Fig. 1)
Vitiligo is one of the oldest (the disease has existed on earth for more than 1 century) and unstudied diseases. The pathology is referred to as skin dyschromia. To date, the main cause of this disease has not been established. The pathology is not contagious, but heredity matters. Presumably the disease is associated with the following factors:
- disorders in the immune system;
- neuroendocrine disorders, diseases of the thyroid gland, pituitary gland or adrenal glands;
- diseases of the autonomic nervous system;
- enzyme deficiency;
- autoimmune cause;
- psychological trauma, frequent stress;
- metabolic and vitamin imbalance;
- infection by parasites, past infectious disease;
- sunburn;
- accumulation of chemical compounds.
What are skin plaques
In general, plaques that appear on the surface of the skin can be described as small-sized compactions of the upper layer of the epidermis, which can have different sizes, appearance, be single and merge as the underlying disease progresses into large areas of damage. In appearance, these neoplasms may have a different shade, type of skin located on the surface of the plaque; during their development, unpleasant subjective sensations may arise or they may be absent.
The methodology for classifying the neoplasms in question on the surface of the skin is different; it assumes the presence of specific differences both in the appearance of the plaques and in the structure of the skin and tissues under the skin. With different types of dermatological lesions, the plaques on the skin are different. To draw up the most effective treatment regimen, a dermatologist first carries out a complete diagnosis of the affected areas of the skin and identifies the probable causes of the development of this pathology.
The boundaries of skin plaques can also be different: in some cases, the boundaries of the plaques are clearly defined and structured. With other skin diseases, the boundaries are less clear; plaques may be located in the form of a spot or in a place where the skin has changed color. When several plaques merge into one, a change in skin color is observed.
Damage to such neoplasms on the skin can occur due to internal negative changes within the body and under the influence of external factors. Representatives of all social groups are susceptible to this manifestation, regardless of age. Most plaques on the skin are diagnosed in childhood and adolescence, as well as during menopause and pregnancy - during the period of hormonal changes in the body.
Cholesterol plaques on the eyelid (photo)
Treatment of the disease
At the moment, the disease is considered incurable, but medical practice has recorded cases where patients managed to achieve noticeable improvements. It is better to start treatment at an early stage of the disease. As soon as you notice the first white spots on your body, get examined. There are several ways to treat vitiligo:
- The PUVA therapy method uses ultraviolet radiation of a certain length and intensity to restore pigmentation.
- Glucocorticosteroid drugs in the form of cream and ointment. Hormonal ointments stop the destruction of melanocytes.
- Laser and monochromatic light procedures.
- Selective phototherapy is a spectrum of specific radiation that uses the positive effects of ultraviolet radiation and eliminates its negative properties.
- In case of extensive lesions, donor skin transplantation is practiced, having previously treated the transplanted skin area with the PUVA method.
- Vitamin therapy includes vitamins B, A, C, and injection of the affected skin.
- Diet. The mandatory menu includes seafood, lamb, rice, oats, tomatoes and apples.
- Phytotherapy. A decoction of medicinal infusions should be used externally and internally.
- The skin whitening procedure is aimed at smoothing the skin through injections.
- Transferring your healthy pigment cells to damaged areas of the skin.
The patient should restore normal metabolism; a sufficient amount of copper, zinc, iron, iodine and the entire complex of vitamins should be present in the body. The condition of the liver and intestines should also be improved. Limit consumption of food allergens. Currently, scientists are working to create a vaccine that neutralizes the autoimmune reaction that triggers the onset of the disease.
Treatment with folk remedies
Sometimes, when treating fungal infections, you can completely do without medications. Foot fungus can be cured using traditional methods yourself at home. How to get rid of fungus on the feet and heels? The tools that are available in every home are suitable for this.
Vinegar
Vinegar. Clean cotton socks should be soaked generously in vinegar and put on cleanly washed and dry feet. Leave the socks on all night, and take them off and wash them in the morning. Feet should be washed after using vinegar.
Laundry soap. This remedy helps get rid of many problems, including foot fungus. First, you should take a warm bath with added saline solution. Then the feet should be thoroughly washed with soap and rubbed with a special brush or pumice stone. This will help soften and remove dead skin. After rinsing your feet with clean water, wipe them dry. It is recommended to repeat the procedure every night.
Tea tree oil. Among the traditional medicine recipes there is a way to get rid of foot fungus using tea tree oil, which must be mixed with aloe juice. The healing mixture should be rubbed into the affected skin of the heels twice a day. Before the procedure, feet should be washed with laundry soap.
Another way to get rid of foot fungus is a rosehip decoction, as well as a mixture of 1 drop of garlic juice, 1 drop of alcohol and 10 drops of water. It is used as a compress, which is applied to the affected areas.
Signs of white lichen
Another reason for the appearance of spots is pityriasis alba. This is a skin disease of unknown origin. It is believed that the main causative agent of this disease is a fungus. People with skin pathologies are at risk. The main symptom of the disease is whitish spots with blurry shapes.
The spot can be from 1 to 4 cm in size and does not cause physical discomfort. They form more often on the lateral surfaces of the arms and legs. The spots are especially noticeable on dark or tanned skin. Adults are very rarely susceptible to this dermatosis; pityriasis alba mainly affects children and adolescents. Lichen alba should be differentiated from vitiligo and pityriasis versicolor. New studies have linked the disease to a lack of copper in the patient’s body. This mineral is essential for the creation of healthy skin cells. Treatment of lichen will be required if a large area of skin is covered in spots and the patient’s condition worsens. Lichen alba is treated with topical medications: creams, ointments, solutions.
Treatment methods
Treatment is based on the causes of white spots on the skin. Therapy is carried out using medications intended for topical use: lotions, creams and ointments. The main active substance in them is the adrenal hormone – cortisone.
If the cause of discolored spots on the legs is a skin disease or pathology of internal organs, diagnosis and subsequent therapy will be aimed at eliminating the underlying disease.
For lenticular hypopigmentation, your doctor may prescribe sunscreens that contain vitamin A.
Treatment with liquid nitrogen is popular. The mechanism of action of the procedure is to destroy affected melanocytes and stimulate the appearance of healthy cells in the discolored area of the skin. However, its effectiveness has not been fully proven.
To eliminate the fungus, ointments or creams that contain antifungal agents are used.
Folk remedies for combating fungal infections on the feet are effective as an additional method of treatment. A well-known home recipe for fighting fungus is lotions with a solution of apple cider vinegar. To prepare it you need to add a few drops of vinegar to the water. It is necessary to wash problem areas 2 times a day.
Guttate hypomelanosis
Guttate hypomelanosis is a benign leukoderma of idiopathic origin. Occurs in fair-skinned, middle-aged women. There is a hereditary predisposition. It is possible that immediate relatives suffered from a similar pathology. The main symptom of the disease is the formation of depigmented round spots. Their sizes range from 1 to 10 mm in diameter. White spots appear on the legs and can then spread to the back and forearm. The facial skin remains untouched. Hair follicles remain intact.
Hypemelanosis does not have a negative impact on health and is a cosmetic defect. The disease develops as a result of prolonged exposure to sunlight. Excessive exposure to ultraviolet rays changes the structure of the skin for the worse. This phenomenon is called skin photoaging. The skin thickens unevenly, elasticity is lost and capillary blood flow is disrupted. The disease can be triggered by taking tetracycline antibiotics and birth control pills.
Hypermelanosis is diagnosed based on examination and histological examination. Other types of skin pathologies should be excluded.
Hypomelanosis differs from vitiligo in the clear outlines of the spots.
The disease is chronic and cannot be permanently cured. To prevent new spots and treat existing ones, you can try hormonal corticosteroid medications. For external use, retinoids and dermotropic drugs are used. Cryomassage of the skin of the affected areas gives positive treatment results. Preventive measures for skin photoaging include the use of photoprotectors and products that protect against ultraviolet rays. There are 2 types of impact:
- Endogenous protectors. Serve to strengthen the immune system and strengthen the body's antioxidant and antiviral defenses. Preparations containing ascorbic acid, beta carotene, flavonoids and selenium are used.
- Exogenous protectors. Protect the outer layers of the skin from exposure to ultraviolet rays: oils, ointments, emulsions and other cosmetic products.
Treatment and prevention of skin photoaging involves an integrated approach, including the use of photoprotectors, medical and cosmetic procedures.
Each person has his own skin color, which is determined by race. Changes in the color of the outer integument carry not only physiological symptoms, but can also cause psychological discomfort.
Drug treatment
Treatment of heel fungus involves the use of inexpensive but effective drugs for external use.
Softening bath
To quickly and efficiently cure heel fungus, you must follow some recommendations:
- wash your feet with warm water and soap
- make a bath to soften the stratum corneum of the skin
- remove dead cells using special brushes
And only after that apply the medicine to the affected surface. Traditionally, to treat foot and heel fungus, doctors prescribe tablets and capsules for internal use, as well as topical antifungal agents. These include:
- Lamisil
- Miconazole cream or ointment
- Clotrimazole
- ointment cream Tolnaftat
- Nomidol
- Tinedol
All these drugs have shown their effectiveness in the fight against foot fungus. However, they also have a number of side effects. That is why it is recommended that treatment be carried out under the strict supervision of a dermatologist. You should refrain from using topical products if:
- individual intolerance
- tendency to allergic manifestations
- sensitivity to individual components
It is necessary for women to avoid the use of drugs during pregnancy and breastfeeding, as well as for children under 6 years of age. If there are cracks in the heels or blisters, the doctor may prescribe salicylic ointment. In the case of an advanced form of the disease, topical medications are not enough.
To increase the effectiveness of therapy, the doctor may prescribe drugs to be taken orally. They are available in tablet form and are prescribed for chronic or particularly severe fungal infections. The most effective are:
- Fluconazole
- Ketoconazole
- Terbinafine
- Itraconazole
The essence of the problem
Skin color is affected by:
- state of the circulatory system - narrowing or dilation of blood vessels, which gives paleness or redness;
- the amount of melanin and carotene.
When the coloring enzyme increases, the spots on the skin become brown, and when there is a deficiency, they turn white.
Some genetic disorders cause a person to not produce melanin. People with very fair skin, or albinos, are susceptible to sun damage and should wear special protective products in the summer.
Red rash in children
Spots on a child’s legs most often appear due to:
- Allergies: to new laundry detergent, to diapers or diaper products, new bath products, after an insect bite, in response to cold or sudden alternation of heat and cold. In this case, the spots rise above the skin and almost always itch, which disrupts sleep and nutrition. Following a hypoallergenic diet, taking sorbents (Atoxil, Smecta, Activated Carbon) and antihistamines (Fenistil, Suprastin, Erius) helps.
- Enterovirus infection. In this case, the rash is most often located not only on the legs, but also on the arms, mainly on the fingers. It looks like blisters surrounded by a red border, almost always very itchy. In this case, there may be an increase in temperature, similar blistering rashes on the oral mucosa, there may be nausea, vomiting, cough, loose stools (the set of symptoms depends on the type of virus acquired through food, water, or airborne droplets).
- Rubella. In this case, red spots are located all over the body, not just on the legs. At the same time, the temperature increased, nasal congestion appeared, and the eyes turned red. The rash does not itch or flake off.
- Corey. Here, red spots on the legs appear last: first, the rash appears on the face, and then goes down, merging with each other. In addition, the temperature rises, snot begins to flow from the nose, conjunctivitis and swelling of the eyelids are noted.
- Scarlet fever. This is a disease that is caused by the same bacterium that causes tonsillitis. Red spots, when pressed on, they appear better, appear on the 1st-3rd day of the disease, are located on the cheeks, on the sides of the body, and not on the legs, but in the groin.
- Meningococcal infection. This is a life-threatening condition that can begin with the fact that after 1-2 days of a runny nose (or even without it), spots appear on the legs and buttocks, the temperature rises, and the spots spread to other parts of the body. At first they may be red, without pustules or blisters. Then they darken, acquire a star-shaped shape, and merge. Dark spots on the legs that do not disappear when a clear glass is pressed on the skin may appear immediately, without a stage of red rashes. The sooner an ambulance is called, the greater the child’s chances of survival.
- Pityriasis rosea. Its manifestations are described above.
- Pityriasis versicolor. There are several similar spots, they are brown-red, cover different parts of the body, do not merge, and the skin above them peels off. The shape of the spots is different, they tend to merge, do not itch or hurt. When the rash disappears, whitish areas remain in these areas.
Children may develop spots due to ringworm and other mycoses, but these causes are more rare than those described above.
Causes of white spots
White spots on the skin of the legs occur under the influence of several factors:
- Liver disorders. This organ produces melanin in the amount necessary for the body. When any disease occurs, the color of the skin changes.
- Insufficient secretion of the pancreas, blockage of the bile ducts.
- Problems with the thyroid gland - the amount of hormones produced affects the skin.
- Parasitic infestations.
- Poisoning.
- The period of bearing a child.
- Frequent exposure to the sun.
- Immunodeficiency states.
- Stressful situations.
Why do red spots appear?
First, let's figure out why red spots appear on the lower extremities and how they form? Dark spots on the legs occur due to weakening of the vascular wall and small hemorrhages.
The appearance of pigmentation on the lower extremities is one of the symptoms of varicose veins.
The venous wall cannot withstand the load, especially in people who are obese or during excessive physical activity. Tissue trophism, which is affected by chronic venous insufficiency, is also disrupted. Hyperpigmentation worsens as the disease progresses. In the last stages of varicose veins, scarlet spots turn into trophic ulcers that practically do not heal. Sometimes this leads to amputation of the limb. At the first manifestations of vascular spots on the legs (see photo), you need to consult a specialist. Self-medication can cost you dearly - for example, by losing a leg.
In the fourth stage, the appearance of dark spots on the legs with varicose veins (shown in the photo) is provoked by thrombosis of deep and superficial veins. This is a complex pathology that is difficult to treat.
The main reasons for the formation of red spots on the legs with varicose veins are considered to be: problems with the cardiovascular system, diabetes, excess weight, injured lower limbs, pregnancy, and infectious diseases.
Vasculitis on the legs
Diagnostics
White spots on the calves and feet require careful examination.
Before making a diagnosis and determining a treatment regimen, the doctor collects an anamnesis of the disease and conducts a visual examination and palpation of the rash area.
Basic research methods:
- blood for general analysis and biochemistry;
- immunogram;
- hormone testing;
- Ultrasound of the liver, kidneys, pancreas and thyroid glands;
- feces on worm eggs;
- dermoscopy;
- scraping from stains if crusts are present;
- blood culture.
Types and descriptions of spots on the legs
The spots can appear on the lower legs, ankles and even feet. Their localization depends on where the vascular problems arose. At first, small reddish spots do not show themselves, but over time, alarming symptoms appear. The spots become painful, itch, and their structure may change. Dense pigmented areas are dangerous.
Inflammation or thrombosis of large vessels leads to the appearance of large red spots on the legs. If small arteries are affected, small spots, dots, or bruises may occur.
During diagnosis, it is important to consider not only the size, but also the shade of the spots on the legs. They are:
- blue, purple - are often mistaken for a hematoma;
- red, bloody - look like a bruise, can be bright or dark;
- black ones are the most harmless, in most cases they are cosmetic defects or benign formations, but some can transform into malignant ones.
They are often round in shape, with clear contours.
Types according to origin:
- Vascular spots on the legs. They are violet, burgundy, lilac, and are often painful to the touch. The appearance of vascular spots on the legs is always caused by poor circulation.
- Hemorrhagic spots on the legs. This is a consequence of vascular damage. More often they are dark red, blue or purple. The cause of stagnant spots on the legs is a blow or other mechanical impact on the skin. Essentially it's a bruise.
Treatment
Therapy for the disease should be comprehensive and include not only treatment with medications, but also physical procedures and dietary nutrition.
Conservative
If rashes in the form of white spots appear on the legs, then apply local treatment to the affected areas. It is not possible to completely get rid of the defect, but many cosmetic procedures help to visually reduce the size of the formations.
One of the treatment methods is exposure to UV rays. To stimulate pigmentation processes, rubbing melagenin lotion into problem areas before the procedure is recommended. The result is noticeable after some time: the spots on the skin initially acquire a reddish tint, and later darken and do not differ in color from the surrounding tissues.
Medicines
The treatment regimen and selection of drugs should be carried out by the attending physician after establishing the cause of the disease.
Systemic treatment includes taking the following medications:
- Short course hormonal drugs. The use of the drug is prescribed both in tablets and topically in the form of creams or ointments.
- Immunostimulants to strengthen the body's defenses.
- Medicines that improve the functioning of the digestive system.
- Agents that restore metabolic processes in the liver and pancreas.
- Vitamins and minerals.
- For frequent stress - soothing teas, antidepressants.
- Antifungal creams.
- Antihistamines.
- Antibiotics, antiparasitic drugs.
Folk remedies
Alternative medicine methods are suitable for people who have hypersensitivity to pharmaceutical drugs. Traditional medicines cannot completely cure the disease, but they alleviate the physical condition of the patient and remove visible cosmetic defects.
Lotions and decoctions of medicinal herbs will help mask spots on the skin:
- Melanin synthesis is improved by parsley, dill, and flax. After applying the product, it is necessary that the affected area be exposed to sunlight.
- Brew linden in a glass of boiling water, let cool, add honey and lubricate problem areas of the skin daily.
- Mix lemon juice with honey and apply to gauze. Apply the product to the stains and leave for 15-20 minutes, then rinse with water.
Exposure to the sun should be carried out with a gradual increase in exposure time, as there is a risk of developing burns.
Surgery
If conservative therapy methods do not bring results, and the formations are large, then surgery is performed to transfer healthy cells to the damaged areas.
A more gentle procedure involves injections to produce melanin in the affected area.
Treatment of vitiligo
Since it is still not known exactly why white spots appear on the legs and body, doctors decide on a therapeutic regimen depending on the patient’s condition:
- a comprehensive examination is carried out;
- the main problems in the body are identified.
They treat helminthic infestations, try to stabilize the functioning of the liver, gallbladder and endocrine system, and prescribe sedatives to stabilize the nervous system.
Traditional medicine offers its own methods for treating the disease. It is proposed to prepare one of the mixtures according to the following recipe.
Required ingredients:
- 30 g each take - parsley, aloe, plantain, yarrow, pine buds, flowers and peony root, lingonberries, hare cabbage, Chernobyl, calamus root, St. John's wort, nettle, dried grass, oregano and lemon balm;
- 15 g each - cloves, wormwood, lovage flowers, crushed pine nuts - with shells, dandelion, juniper fruits;
- lemon zest – medium size.
All these herbs are mixed, 300 g are measured, 2 liters of vodka are poured in warm form, and infused in a warm place in the dark. It is advisable to stir at least occasionally.
Further, the opinions of traditional healers differ. One half suggests taking a teaspoon of the mixture diluted in 50 ml of water, the other half suggests applying lotions directly to the affected areas with a medicine diluted half with water.
There is another method of treatment proposed by traditional medicine. Since spots can appear at any minute, you need to constantly examine yourself. As soon as they begin to form, pink dots will appear; they should immediately be treated with your own urine.
If vitiligo occurs during pregnancy, you should never experiment. Changes in skin pigmentation do not affect the child’s condition, and it is very likely that after childbirth, vitiligo will disappear on its own.
Prevention
To prevent the development of unwanted pigmentation, you should adhere to the following rules:
- Maintaining proper nutrition: introducing vegetables, fruits, and herbs into the diet.
- Eliminate unhealthy foods - smoked foods, fatty foods, fried foods, salted fish, fast food.
- To refuse from bad habits.
- When visiting public places, baths or saunas, use only personal items and hygiene products.
- Daily moderate physical activity or a long walk in the fresh air.
- Strengthening the immune system: hardening, walking barefoot on grass or pebbles.
- Timely consultation with a doctor at the first signs of illness.
Prevention methods
Let us highlight the main ones:
- When sitting or standing for a long time, you periodically need to get up, warm up, or change your supporting leg.
- Wear comfortable shoes with low heels.
- Play sports, but avoid strenuous physical activity, especially for people with a genetic predisposition.
- Lose weight if you are already overweight.
- Pregnant women should pay special attention to preventive methods.
Photo from youtube.com
Causes and mechanisms
The appearance of white spots on the skin is mainly due to a change in normal pigmentation. Areas where there is less melanin appear lighter than the surrounding areas. And among the causes of such hypopigmentation you can most often find:
- Vitiligo.
- Pityriasis versicolor.
- Guttate hypomelanosis.
Weakening of color in certain areas occurs after inflammatory pathology (psoriasis, lupus erythematosus, neurodermatitis, scleroderma), as a result of burns, injuries or exposure to chemicals. Hypopigmentation sometimes turns out to be syphilitic or leprosy leukoderma, a consequence of genetic abnormalities or helminthic infestation. As you can see, there are many reasons for the appearance of white spots on the lower extremities and each case should be considered individually.
Why does heel fungus occur?
Fungus on the heels can appear due to:
- presence in public places (sauna, swimming pool, bathhouse, etc.) without special shoes
- wearing someone else's underwear (shoes, socks), as well as using bed linen and towels
- the presence of cracks in the heels, facilitating the penetration of microbes
- poor foot care
- weakening of the body's protective functions
- hormonal disorders
- getting injured
To confirm the correct diagnosis and find out how to treat heel fungus, you need to contact a dermatologist by appointment. Based on the diagnosis, which includes examining the patient, collecting anamnesis and conducting laboratory tests, he will be able to make the correct diagnosis and develop a treatment regimen for heel fungus.
To correctly determine how to treat foot fungus, it is necessary to determine the form of the disease and the stage of its development. In many ways, methods of treating fungus depend on the type of parasite and the degree of infection. In any case, therapy should be aimed at eliminating the provoking factor, relieving inflammation, as well as eliminating associated symptoms. Among the frequently asked questions is the question of how long therapy can last?
This depends on the individual characteristics of the body, the effectiveness of medications, as well as the form and stage of the disease. Taking into account the latest advances in medicine, we can confidently speak about the effectiveness of therapeutic treatment and shortening its duration, without surgical intervention.
The appearance of white spots on the feet indicates the occurrence of disorders in the human body. Externally, they can take different forms.
A) Large flat spots or corns:
- as a result of wearing uncomfortable shoes;
- due to flat feet and excessive pressure on the foot;
- due to dry skin of the feet and insufficient elasticity.
B) A spot in the form of a callus - from uncomfortable shoes.
C) Formations in the form of tubercles on the heel of the foot, usually white in color:
- may protrude above the skin;
- have a flat shape and do not protrude outward;
- in the form of small dots-nodules;
- gray or brown flat plaques are “senile” plaques.
D) White plaque on the feet as a change in skin pigmentation.
E) White spots with holes or dots are another subtype of skin disease.
E) Cracks in the heel or other part of the sole.
All of them are related to cosmetic phenomena, but the causes of their occurrence should be sought with the help of a dermatologist.
The presence of external manifestations on the skin often indicates the papilloma virus, which makes it unpleasant and painful to move. The virus is transmitted through contact of carrier objects with damaged areas of the skin (cracks). Activation of activity occurs against the background of a general weakening of the immune system or as a result of a nervous shock experienced.
The spots, called white, may also have other colors. They are divided into vascular - their appearance is caused by various inflammatory processes, and pigmentary - due to a reaction to ultraviolet rays. Or due to changes occurring within the body.
The same banned issue for which Ernst fired Malakhov!
Joints and cartilage will be cured in 14 days with the help of ordinary...
Have you been trying to heal your JOINTS for many years?
Head of the Institute for Joint Treatment: “You will be amazed at how easy it is to heal your joints by taking every day...
Symptoms
It is difficult to say why lesions with reduced pigmentation appear on the legs without examination. But by consulting a doctor, the patient can be confident that he will receive an answer to his question. First, anamnestic information is obtained, and then the affected areas are examined. A preliminary diagnosis is based on the results obtained.
Vitiligo
Spots completely devoid of melanin are characteristic of vitiligo. The nature of the disease is not fully understood, but autoimmune, hormonal, hereditary and external factors are assumed to be involved in its development. First, a single white spot of various shapes forms on the soles of the feet or another area of skin. It can maintain its size for a long time - then they speak of a stable phase of the disease. If its diameter increases and new foci of depigmentation appear, then progressive vitiligo is confirmed.
The spots that appear do not cause any subjective sensations. They lack melanin, so they are prone to redness when exposed to sunlight. As a rule, vitiligo is only a cosmetic defect, but if it develops, the patient should be examined for possible abnormalities in the functioning of the body.
With vitiligo, depigmented lesions form, which can cover large areas of the skin.
Pityriasis versicolor
White spots on the feet can appear with pityriasis versicolor (lichen versicolor). This is a pathology caused by a fungal infection of the stratum corneum of the epidermis (keratomycosis). The spots with lichen initially have a pink-yellow-brown color, but under the sun they do not tan, so they become lighter. They tend to merge and form large lesions with scalloped edges.
The favorite localization of spots is the skin of the torso, but elements of the rash can also be located on the lower extremities (especially in children). Lichen versicolor does not bring any subjective discomfort; only slight itching is possible. The spots are accompanied by fine-plate peeling, which can be revealed by light scraping. Without treatment, the disease can last for a long time, causing relapses.
Guttate hypomelanosis
Another condition that causes white patches to appear on the skin of the legs is guttate hypomelanosis. Light dots, not exceeding 10 mm in diameter, are localized mainly on the flexor surfaces of the knee or elbow joints. Mostly middle-aged women suffer from this type of pigmentation disorder. The spots have smooth outlines, never merge with each other and are not accompanied by subjective symptoms.
Psoriasis
The consequences of various dermatoses of inflammatory origin can also look like hypopigmentation. Lighter areas, including on the feet, can form during the period of resolution of psoriatic plaques. The latter first look like flat, bright red papules with a scaly surface. But in the progressive stage, the elements increase in size and cover increasingly larger areas of the skin.
Psoriatic lesions most often resolve with the formation of hypopigmented spots that disappear over time.
Causes
The most likely cause of dark spots on the legs that are not caused by mechanical stress is varicose veins. However, along with hematomas, other signs appear:
- swelling of the skin at the site of the vein;
- pain;
- bulging vein;
- cramps, numbness.
Why does the skin on the legs become covered with spider veins? This is a consequence of capillary expansion, one of the stages of varicose veins. Blood spots appear at the sites of hemorrhage. If the integrity of the vessels is not broken, then they are dark brown or brown. Their appearance is associated with the accumulation of blood in the veins. Without treatment, trophic ulcers may appear and varicose eczema may develop.
With thrombophlebitis, the skin acquires a bluish tint, and purple or burgundy spots on the legs are likely.
Changes in pigmentation may be associated with other vascular diseases:
- chronic venous insufficiency;
- varicose dermatitis;
- vasculitis, or inflammation of blood vessels;
- trophic disorders - a dark spot may appear, which will gradually darken even more;
- deep vein thrombosis – the spot hurts , reaches an impressive size, swelling appears, and the temperature rises;
- vascular atherosclerosis;
- Erythema nodosum - characterized by the formation of brown spots in the ankle joint;
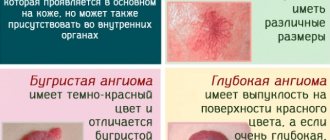
- A hemangioma is a round, dense vascular formation that can be varied in appearance.
In all these cases, dark spots may appear on the legs. A hemangioma may look like a wart or a blood spot. Sometimes it appears as a black spot , first flat and then convex.
With varicose dermatitis, severe itching appears, the spots itch and flake, but they cannot be scratched.
If itchy red spots appear on the calves of the legs, you should be examined for an allergic reaction. The cause can also be a fungus or lichen.
Spots on the ankles can appear due to uncomfortable tight shoes. The cause may be joint diseases. But spots on the feet and calves are often the result of diabetes mellitus, a complication of which is diabetic angiopathy. Without treatment, tissue necrosis is likely.
Red spots on the feet can also appear with flat feet, but they never change their color or become bluish or black.
Very often, bruises and hematomas remain after surgery on the veins of the legs. At the end of the postoperative period they disappear.
Additional diagnostics
It will be possible to understand why white spots appear on the sole or other parts of the lower extremities after a comprehensive examination. Based on the probable causes and results of the medical examination, a diagnostic program is formed, which may include:
- General and biochemical blood tests.
- Serological tests (presence of antibodies).
- Study under a mercury-quartz Wood lamp.
- Iodine test.
- Microscopy and seeding of particles taken during scraping.
- Histological analysis, etc.
Sometimes it is necessary to exclude disorders of the internal organs, which instrumental studies will help with. Some patients need consultation not only from a dermatologist, but also from an immunologist, endocrinologist or geneticist. And only the results of a comprehensive diagnosis will give grounds to assert the reasons for which white spots appeared on the legs. And this, in turn, opens up the possibility of adequate therapy.
Hygiene rules and prevention
Treatment of age spots on the heels caused by excessive physical impact on these parts of the body is carried out by making changes in foot care (massage, medicinal baths, medicated ointments, timely pedicures). Changing shoes to ones that are comfortable for walking, regularly performing gymnastic exercises for the feet, and daily hygiene procedures will help. Important proactive actions will be maintaining a comfortable neuropsychological state and restraint in nutrition to maintain a physiologically normal body weight.
White spots on the feet require careful diagnosis and examination of the body. If it becomes painful to step on for no reason, or formations appear on the skin, consult a doctor to rule out the presence of pathologies.
White spots on the legs are a symptom of pathology of internal organs or a sign of the appearance of a skin disease. The cause may be ultraviolet radiation or chemical burns. How to remove white spots? What methods can prevent their occurrence?
Useful video about spots on legs
List of sources:
- Grishin I. N., Podgaisky V. N., Starosvetskaya I. S. Varicose veins and varicose veins of the lower extremities. M., 2005.
- Russian clinical guidelines for the diagnosis, treatment and prevention of venous thromboembolic complications // Phlebology (add.). 2010. T. 4. Issue. 2. No. 1. 37 p.
- Phlebology: A Guide for Doctors / ed. V. S. Savelyeva. M.: Medicine, 2001.
>
Comment
0