Androgen levels in the blood of pregnant women
During normal pregnancy, serum concentrations of some, but not all, androgens increase.
Testosterone during pregnancy (“Male” hormone during pregnancy)
Total testosterone levels gradually increase during pregnancy. This effect is explained primarily by a gradual estrogen-induced increase in serum concentrations of sex hormone binding protein (SHBG). An increase in testosterone concentrations during normal pregnancy occurs as early as 15 days after the LH peak, probably due to its production to a greater extent by the ovaries than the adrenal glands.
There are several studies examining androgen production and breakdown in healthy pregnant women. In one of them, when examining five pregnant women, it was revealed that the rates of production of testosterone and dihydrotestosterone in pregnant and non-pregnant women were the same. However, the conversion of testosterone to dihydrotestosterone and the metabolic clearance of these hormones were lower during pregnancy, as would be expected with elevated serum concentrations of SHBG.
Another study, which included an examination of 1,343 women with singleton pregnancies, found lower androgen levels in women over 30 years of age, as well as multiparous women (two or more births). While smoking was associated with higher androgen levels in the first half of pregnancy compared to younger women, nulliparous women and non-smokers, respectively.
During pregnancy, testosterone concentrations in serum are three to four times higher than in umbilical cord blood serum. The concentration of testosterone in the blood of a pregnant woman can range from 100 to 140 ng/dL (3.5 to 4.8 nmol/L), and in umbilical cord blood the average value is 33.5 ng/ml (1.2 nmol/L).
Free testosterone during pregnancy
The serum concentration of free testosterone changes slightly during pregnancy until the third trimester, when it approximately doubles. This increase in free testosterone concentrations cannot be explained by changes in SHBG concentrations and may most likely be a consequence of increased testosterone production. The source of increased testosterone production in this situation is unknown. One possible reason may be that human chorionic gonadotropin (hCG) can stimulate the theca-interstitial cells of the ovary to synthesize testosterone, however, the concentration of hCG in the blood serum reaches its peak at the end of the first trimester of pregnancy and then gradually decreases, and the concentration of free testosterone increases . As studies have shown in great apes, one of the possible sources of testosterone is the corpus luteum. Finally, testosterone may be produced in the adrenal cortex of pregnant women, paralleling an increase in maternal cortisol secretion late in pregnancy.
DEA-S during pregnancy
The concentration of dehydroepiandrosterone sulfate (DHEA-S) in the mother's blood decreases during pregnancy, despite an increase in its production in the fetal blood. The greatest decrease occurs at the beginning of the second trimester, when the metabolic clearance of DHEA-S increases sharply. In pregnant women, DHEA-S is metabolized in the liver, by conversion to 16-alpha-hydroxy-DHEA, and in the placenta, by conversion to estrogens.
Androstenedione during pregnancy
The concentration of androstenedione in the mother's blood increases in the second half of pregnancy.
Androstanediol glucuronide during pregnancy
Serum concentrations of 3-alpha-17-beta-androstanediol glucuronide (3a-diol-G), a product of dihydrotestosterone metabolism in skin hair follicles, increase during pregnancy in pregnant women. It is not completely known whether this is due to increased activity of 5-alpha reductase and other androgen-metabolizing enzymes, or to increased substrate availability.
The mechanism of action of the hormone on the female body
What is the mechanism to counteract the increase in testosterone growth in the female body? A fairly common question, especially when it comes to reproductive issues.
First of all, you need to adjust your own diet. Often failures are the result of improper nutrition. That is why it is immediately necessary to give up vegetarianism. Next, you should reduce animal fats in your diet and try to maximize your intake of fruits and vegetables.
Added to the menu:
In the case of a strict diet, most likely, some of the above elements will have to be abandoned.
Most experts in this situation (the desire to get pregnant, but not lose their figure) advise girls to attend yoga classes. According to professionals, these exercises allow you to cleanse the body of toxins, removing them naturally while restoring hormonal balance.
However, it is worth paying attention to the regularity of classes. In the case of consistent yoga training, the body will always remain in good shape, thereby preventing hormonal imbalances.
Regarding folk remedies, the following can be noted. Based on medicinal preparations, the following will help lower testosterone levels: evening primrose, licorice root and Maryin root, sacred vitex and others. In addition, the consequences of this treatment will help relieve the fair sex from insomnia, arrhythmia and excessive sweating.
The most effective is the combination of traditional medicine with drug therapy. The use of hormonal therapy is also likely. Unfortunately, this option can be called an extreme option. It is prescribed only when the level of the hormone is extremely high, which is a threat to the woman’s life.
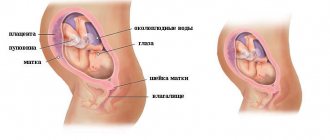
Androgen levels in amniotic fluid
The concentration of testosterone and androstenedione in amniotic fluid is, on average, approximately two to three times higher if the fetus is male. The median probable deviation in boys is 17.3 to 33.7 ng/dL (0.60 to 1.17 nmol/L) and 5.05 to 12.98 ng/dL (0.175 to 0.45 nmol/L) in girls. This difference in levels between male and female fetuses indicates that at least part of the androstenedione and testosterone in amniotic fluid is produced by the fetal testes. The concentration of DHEA-S in amniotic fluid is the same in female and male fetuses. This is probably due to the fact that this hormone is of adrenal origin.
Why is there increased testosterone in women when planning pregnancy?
Author: Rebenok.online · Published 02/27/2017 · Updated 02/14/2019
Testosterone is considered primarily a male steroid hormone. But in the female body it is necessarily present in relatively small quantities.
Deviation of this hormone from the norm adversely affects the health of girls in general, and also prevents successful conception when planning pregnancy.
Androgen levels in fetal blood
Testosterone —Serum testosterone concentrations are higher in male fetuses than in female fetuses, while dihydrotestosterone concentrations are similar.
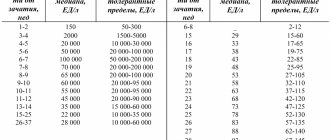
In male fetuses, testosterone concentrations peak at the end of the first trimester of pregnancy at about 150 ng/mL (5.2 nmol/L; half the lower limit of normal in adult males), and then gradually decrease to about 60 to 70 percent. .
Little is known about the regulation of fetal testosterone, but it is thought to be more dependent on maternal hCG levels than on fetal pituitary luteinizing hormone (LH). Concentrations of hCG in maternal and fetal blood peak between 9 and 12 weeks of gestation and then gradually decline (maternal hCG concentrations in fetal serum are significantly lower than in the mother's own serum: fetal readings can range from barely detectable to 2.5 mIU/ml).
The appearance of maternal hCG in the fetal serum coincides with the appearance of Leydig cells (the source of testosterone production in the testes), which occurs around 8 weeks of pregnancy. It is assumed that maternal hCG plays an essential role in the development of Leydig cells in the fetus and in the production of testosterone. Leydig cell formation peaks between 14 and 18 weeks of pregnancy.
Gonadotropins are detected in the fetal pituitary gland at approximately 10 weeks of pregnancy, and in fetal serum approximately another week later. A study conducted on transgenic male mice, as well as the late onset of gonadotropin production in the fetus, confirms the theory that the development of Leydig cells and testosterone production is initiated mainly by maternal hCG. In addition, Leydig cell function was found to be normal in mice lacking LH or its receptors.
In female fetuses, serum testosterone concentrations are low (about 50 ng/dL [1.7 nmol/L]) and tend to decrease during most of pregnancy. The source of testosterone is most likely the fetal ovaries, because gonadotropin can stimulate the production of androgens in the fetal ovaries, which are subsequently converted into estrogens.
Reasons for increasing testosterone
If pregnancy occurs with elevated testosterone, a diagnosis of hyperandrogenism may be made, but this is an extremely rare case in medical statistics. After conception, protective structures operate in a woman’s body to protect her and the fetus from the negative effects of increased hormone levels.
The reasons for this increase may be:
- Congenital pathologies of the adrenal glands or ovaries;
- Polycystic formations in the reproductive system;
- Poor nutrition;
- Taking certain hormonal medications (for example, oral contraceptives).
In addition, a genetic predisposition to this condition has also been proven. Pregnancy and testosterone are interconnected, so if you have the slightest doubt, you need to undergo diagnostics and find out the cause of elevated hormones.
Androgen levels in newborns
In newborn boys, the level of testosterone concentration in the umbilical artery is only slightly higher than in girls. However, the concentration of testosterone (and androstenedione) in the blood increases significantly during the first 24 hours of life, especially in boys, and then decreases over the next six days.
An increase in androgens during the first day of life may be a response to the production of free hCG.
During pregnancy, other steroids produced by the placenta may partially inhibit the effect of hCG on fetal cells. The decrease in the concentration of serum androgens during the first week of life occurs simultaneously with a decrease in the concentration of hCG in the blood serum.