Streptoderma is a dermatological bacterial disease caused by streptococci. It is characterized by the formation of pinkish, flaky, round spots on the skin.
It is more correct to call this disease streptoderma, since together with staphyloderma, they form a large group of pustular skin diseases (pyoderma). The development of these diseases is based on a purulent inflammatory process that affects the skin and subcutaneous fat. All pyoderma are divided into clinical forms depending on the pathogen, the prevalence and depth of the inflammatory process.
Pyoderma code (staphyloderma and streptoderma) ICD 10 – L08.0. Streptococcal impetigo is classified as L01. Erysipelas (caused by group A beta-hemolytic streptococci) is classified as A46.
Streptoderma - classification
Depending on the depth of the inflammatory process, streptoderma is usually divided into superficial and deep.
Superficial forms of streptoderma are presented:
- streptococcal impetigo;
- crevice impetigo;
- paronychia;
- papulo-erosive streptoderma;
- intertriginous streptoderma;
- erysipelas;
- streptococcal toxic shock syndrome;
- acute diffuse streptoderma.
Deep forms of streptoderma include cellulite (phlegmon of subcutaneous fat) and vulgar ecthyma.
For reference. In some cases, the inflammatory process can be caused by mixed flora (staphylostreptoderma), in which case superficial vulgar impetigo most often develops.
Causes of streptoderma
Normally, human skin is colonized by a large number of opportunistic microorganisms. They constitute its natural microflora and do not cause an inflammatory process.
They also help maintain the skin's natural defense mechanisms.
With a sufficient level of immunity, intact skin has nonspecific resistance (relative innate resistance to some pathogenic microorganisms). Nonspecific resistance is the first protective barrier that prevents infectious agents from entering the body.
Fatty acids secreted by the skin have a pronounced bactericidal effect (destroying) on group A beta-hemolytic streptococci.
Attention. In the presence of risk factors (decreased immunity, skin trauma, etc.), the level of nonspecific resistance is noticeably reduced. Against this background, the inflammatory process can be caused by both pathogenic microorganisms and opportunistic microorganisms that are constantly present on the skin.
Risk factors contributing to the development of inflammatory processes in the skin and subcutaneous fat are:
- immunodeficiency states;
- stress, chronic sleep deficiency, overwork;
- constant hypothermia;
- work in hot, stuffy rooms;
- living in regions with a humid climate;
- work in conditions of high humidity (greenhouses, etc.);
- violations of the integrity of the skin;
- deficiency of vitamins A, B, C, E, as well as zinc, magnesium or sulfur;
- unbalanced diet;
- hormonal changes (adolescent acne, etc.);
- endocrine diseases (diabetes mellitus, polycystic ovary syndrome, thyroid disease, etc.);
- concomitant skin diseases (dermatitis, psoriasis, etc.);
- failure to comply with personal hygiene rules;
- improperly selected skin care (overdrying the skin, using too aggressive cleansers, etc.);
- use of low-quality cosmetics;
- obesity;
- the presence of foci of chronic infection (streptococcal tonsillitis).
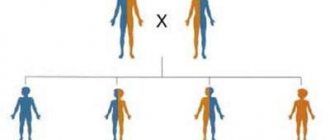
Attention. Due to the lack of barrier functions of the skin, young children are more predisposed to staphylo- and streptoderma than adults.
What can cause streptoderma
The most pathogenic streptococci for humans, often causing streptoderma, are hemolytic, viridans and non-hemolytic streptococci.
The main cause of all streptococci are beta-hemolytic streptococci of group A. Viridans and non-hemolytic streptococci affect the skin less frequently and, as a rule, cause streptoderma in children or weakened patients.
For reference. The prevalence of streptoderma is determined by the fact that about 45% of schoolchildren (in older patients this percentage is higher) are chronic carriers of group A beta-hemolytic streptococci in the nasopharynx.
Streptococci are transmitted by airborne droplets, coughing, talking or sneezing.
In the presence of streptococcal inflammatory processes on the skin (erysipelas, impetigo, etc.), the infection can be transmitted by contact (personal items, sheets).
For reference. The main difference between streptoderma and staphyloderma is damage to smooth skin.
With streptoderma, the skin around the mouth, the skin of the legs, armpits, over the mammary glands, in the groin and buttock folds, etc. are affected. There is also a peripheral spread of the inflammatory process (from the center to the periphery).
Sources of infection
You can become infected with streptococcal dermatitis from a sick person. For this reason, the disease spreads quickly in children's groups, since children come into close contact with each other while playing. The source of spread of pathogenic microflora can be:
- microorganisms living on the skin;
- any things used by the sick person;
- from a sick person, and he may suffer not from dermatitis, but, for example, from a sore throat, that is, any disease caused by a streptococcal infection;
- You can become infected not only from a person who is clearly sick, but also from an apparently healthy carrier.
Advice! The disease is most severe if the infection occurs from a sick person, since pathogens living in the most favorable conditions for their reproduction are more resistant and aggressive.
Thus, there are three routes of infection:
- Contact. Transmission of infection occurs by touching a patient - by hugging or shaking hands.
- Domestic. You can become infected by using objects that have been used by someone who is sick.
How does streptoderma begin in children?
Streptoderma in children most often occurs as papulo-erosive streptoderma and streptococcal impetigo. Streptoderma on the face of a child often occurs as crevice impetigo (sealing in the corners of the mouth) or Fox's streptococcal impetigo.
Papulo-erosive streptoderma: symptoms
For reference. Papulo-erosive streptoderma most often occurs in infants.
Predisposing factors contributing to the development of this streptoderma are:
- improper child care,
- constant use of diapers,
- the baby has heat rash,
- irritating effect of urine on the skin (with infrequent diaper changes and rare washing of the child),
- use of aggressive detergents when washing clothes, etc.
This streptoderma is located mainly on:
- buttocks,
- gluteal folds,
- hips,
- crotch,
- scrotum
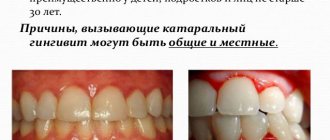
For reference. Symptoms of papulo-erosive streptoderma are manifested by the appearance of dense bluish-reddish papular rashes. Around the papules there is a halo of hyperemia (redness).
On the surface of a papular rash, phlyctenas (purulent formations with an easily ruptured cover) often form. After rupture of the conflict, the erosive surface is exposed. The skin around the erosions is inflamed, swollen and hyperemic.
The formation of crusts (dry or weeping) is also characteristic.
Streptococcal Tilbury-Fox impetigo
For reference. Streptococcal impetigo occurs mainly in children. This type of streptoderma is highly contagious. Therefore, often when impetigo occurs in one child, the entire team becomes infected.
This type of streptoderma is characterized by the appearance of serous-purulent or serous (vesicles with a flaccid, flabby lid and transparent contents) phlyctenas, surrounded by a halo of hyperemia.
As the disease progresses (3-4 days), the phlyctens dry out, forming loose, yellowish-green crusts. After the crusts fall off, erosive surfaces may be exposed. After healing of erosions, temporary foci of hyperpigmentation and peeling remain.
The formation of deep atrophic scars is not typical for this streptoderma.
The disease is often complicated by the addition of lymphadenitis (inflammation of the lymph nodes) and lymphangitis.
Streptococcal impetigo is located mainly on:
- facial skin,
- around the lips (and on the red border of the lips),
- around the wings of the nose, etc.
For reference. A severe type of streptococcal impetigo is bullous impetigo.
How does streptoderma begin as bullous impetigo?
Bullous streptoderma primarily affects the skin on the hands, legs and feet.
The disease is accompanied by the appearance of large blisters filled with serous-purulent or serous contents. The size of the bubbles can reach several centimeters. The bladder cover is tense, the formation is surrounded by an inflammatory rim. The severity of the disease is determined by the thickness of the stratum corneum of the skin in areas of inflammation.
After opening the bubble, extensive erosive surfaces are exposed.
Intertriginous streptoderma
The inflammatory process affects the skin in the inguinal and buttock folds, the axillary region, behind the ears, and under the mammary glands.
This type of streptoderma is typical for patients with obesity, severe sweating, severe cardiovascular pathologies or diabetes mellitus.
In severe cases of streptoderma, ulceration of inflammation and the appearance of purulent and purulent-hemorrhagic crusts are possible. It is also possible that lymphangitis and lymphadenitis may occur.
Streptoderma on the face in the form of seizures (cleft impetigo)
Cleft impetigo is located in the corners of the mouth. The disease can be either concomitant (combined with another type of staphylo- or streptoderma) or the only appearance of streptococcal skin lesions.
Seizures have a highly specific clinical picture. The skin affected by streptococcus is swollen and inflamed. In the depths of the folds, quickly opening conflicts and erosions form with overhanging white rims of exfoliated epithelium. Next, a loose crust forms, easily torn when moving the lips.
Dry streptoderma (lichen simplex)
Dry streptoderma occurs mainly in children. Adults get sick much less often.
The cause of this streptoderma is low pathogenic strains of streptococci.
Most often, lichen simplex occurs in organized children's groups in the spring. Predominantly exposed areas of the skin are affected (face, hands, etc.).
The disease manifests itself as pink spots with whitish scales. When a large number of scales appear, the spots become gray. After the disappearance of the scales, a focus of temporary hyperpigmentation remains.
For reference. Lichen simplex is characterized by a long, sluggish course and frequent relapses.
Treatment
With adequate therapy, a mild degree of the disease (impetigo) can be treated within 5-7 days. More severe degrees (ecthyma, ulcerative lesions) will require more time - up to several months. Treatment can last up to 3 months if the body’s immunity is weakened. After consultation with a doctor, therapy is carried out at home independently.
The therapy method involves local treatment: external treatment and application of antibiotic ointments. Treatment is necessary to prevent the spread of infection to healthy areas of the skin. Antibiotics can destroy streptococcus. The treatment procedure is as follows:
- Lubricate the lesion with a solution of hydrogen peroxide (3%).
- Drying the wound with a cotton swab.
- Applying iodine, brilliant green, alcohol or salicylic solution (optional) around the wound.
- Lubrication with antibiotic ointment (erythromycin ointment).
- Applying a sterile dressing for deep lesions.
A person is considered cured when the clinical picture of the disease changes: the crust disappears, the spots change color. They take on a pink or brownish-pink hue. In this case, the patient ceases to pose a danger to others - he is no longer contagious . The pink mark left after the source of inflammation goes away on its own within 5 days.
Important! Doctors strongly recommend avoiding water procedures during treatment and limiting yourself to wet wiping.
Traditional treatment
Traditional methods are used as additional treatment. Basically, they are limited to washing with various decoctions and applying lotions. The following tools work well for this:
- Elderberry bark . Grind and mix with a glass of milk. Boil the mixture and let it brew. Soak a cotton swab in the broth and go over problem areas.
- Walnut leaves . Use dried leaves. Two tbsp. l. pour boiling water over the leaves. Let cool. Drink the resulting infusion twice a day, 100 g.
- Sophora japonica . The plant must be crushed and filled with moonshine (1:10). It will take time to get an infusion. After this, wipe the areas of the disease 2 times a day.
- Oak bark . Bring the bark to a mushy consistency. Pour boiling water at the rate of 1 tbsp. l. bark per glass of boiling water. Add 1 tsp. alcohol Soak cotton swabs in the resulting liquid and wipe the affected areas.
Streptoderma in children - how to treat
Treatment of streptoderma should be carried out exclusively by a specialist. All medications must be prescribed by a dermatologist.
For reference. In case of deep streptoderma, surgical treatment may be necessary, opening and draining the purulent cavity with its subsequent washing with antibacterial solutions. Surgical excision of necrotic surfaces may also be necessary.
Streptoderma in adults - treatment
The principles of treatment of streptoderma in adults and children do not differ. However, when prescribing drugs, age restrictions on their use must be taken into account.
Diagnostics
First of all, the specialist examines the patient, finds out complaints, living conditions and what diseases he suffered in the near future.
Scraping from the affected area will help determine the pathogen; bacteriological examination is also carried out. Based on the results, antibacterial therapy is prescribed. Additionally, the skin is illuminated with a Wood's lamp.
To diagnose the disease, they donate blood for sugar and other tests.
During the examination, a person passes:
- Analysis of urine;
- biochemical and general blood test;
- blood for sugar;
- feces on worm eggs.
To differentiate streptoderma from skin tuberculosis and ulcers that form with syphilis, a Mantoux test is done and blood is taken for RV.
Streptoderma - how to treat it
All treatment must be carried out under the supervision of the attending physician.
Treatment depends on the type of streptoderma, the patient’s age, the state of his immunity, the prevalence and depth of the inflammatory process, the presence of complications and concomitant pathologies that aggravate the course of the disease.
To treat streptoderma, ointments and lotions with antiseptics or antibiotics can be used. Systemic antibacterial therapy (azithromycin, erythromycin, ceftriaxone, cefazolin, cephalexin, doxycycline, gentamicin, ciprofloxacin, etc.) may also be prescribed.
For reference. Taking antibiotics for streptococcal infections should last at least 10 days. Immunomodulatory therapy may also be prescribed.
According to indications, additional physiotherapeutic treatment may be carried out.
Prevention
Doctors advise following several rules to prevent streptoderma:
- Detect skin lesions promptly.
- Be able to distinguish streptoderma from other skin diseases.
- Treat concomitant diseases that are a risk factor for the development of streptoderma (gastrointestinal diseases, renal dysfunction).
- Strengthen immunity.
- Maintain hygiene standards.
- Eat right and follow a diet.
- Reduce contact with people suffering from infectious diseases.