Angiopathy – abnormal processes in blood vessels that occur due to a violation of nervous regulation.
The size of the veins and arteries changes, they become twisting. Ultimately, the blood supply deteriorates and the functioning of organs is disrupted.
Odnoklassniki
Characteristics of the disease
Angiopathy of the retinal vessels reflects insufficient blood supply to the organs of vision, which leads to distortion of perceived visual information. The retina is a retina located on the inside of the eyeball, consisting of nerve fibers. The shell perceives the image projected onto it by the lens and cornea. The received data is transmitted to the brain, so the person sees a certain picture.
To perform its functions, the retina requires a constant supply of oxygen and nutrients through elements of the bloodstream system. Angiopathy of the vessels supplying the retina can develop in one or both eyes. If the diagnosis indicates “retinal angiopathy” with o, this means that both eyes are affected, this is the abbreviation that ophthalmologists use when describing the disease.
Angiospasm of the vessels located in the retina leads to occlusion (impaired patency) of the vascular bed. Occlusion of the ophthalmic arteries is clinically manifested by deterioration of visual function. Damage to the central artery often leads to blindness. If the pathology affects single small branches, visual acuity may be preserved. With short-term angiospasms of the vessels supplying the retina, restoration of visual function is possible.
Symptoms
Rapid deterioration of vision is not typical for a disease such as retinal angiopathy. The progression of the pathology may take several years. However, this does not mean that early diagnosis is not important, because dystrophic changes with long-term vascular anomalies are always irreversible. That is why it is necessary to pay attention to the early symptoms of the disease, which appear long before visual acuity decreases. They may differ depending on the causes of retinal vascular insufficiency:
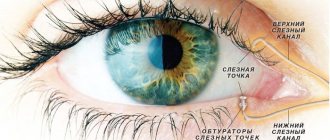
- against the background of diabetic vascular pathology and other endocrine diseases, lacrimation, burning in the eyes, and pinpoint hemorrhages in the sclera are observed;
- against the background of high blood pressure, pulsation is felt in the eyes, headaches and dizziness appear;
- against the background of thrombosis and inflammation of blood vessels, patients are worried about an increasing headache localized in the orbit or behind it, profuse hemorrhage in the eyeball or yellow spots on the sclera, body temperature often rises, fever appears;
- against the background of diseases of the musculoskeletal system, angiopathy of the retina of both eyes is accompanied by a gradual narrowing of the field of vision and the appearance of a foggy veil before the eyes.
With heart disease, there are no visible changes in the eyeballs, but when examining the fundus of the eye, the doctor can detect numerous changes:
- expansion of the lumen of large retinal veins;
- increased branching of the ophthalmic arteries;
- narrowing of the lumen of the eye capillaries;
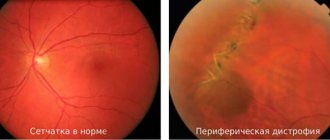
- local or widespread retinal dystrophy.
Additional symptoms that indicate a cardiovascular origin of fundus angiopathy are increased fatigue, shortness of breath during exertion, pain in the chest and limbs, and general fragility of blood vessels.
Classification
Idiopathic angiopathy is a consequence of dysregulation of the muscle tone of the arterial walls, usually developing due to malfunctions of the autonomic nervous system. In newborns, the primary form can occur as a result of intrauterine development anomalies, birth injuries, oxygen starvation caused by asphyxia or other teratogenic factors.
Juvenile angiopathy, also known as Izla disease, is an example of an idiopathic form. It is more often detected in male patients, in 90% of cases it is bilateral in nature. Juvenile angiopathy of the arteries and arterioles of the retina (OU-bilateral) is a disease that is characterized by a gradual development, which makes early diagnosis important.
At the initial (inflammatory) stage, periphlebitis (inflammation of the tissue surrounding the veins) of the peripheral elements of the circulatory system of the retina develops. Immune mechanisms play an important role in pathogenesis. The development of the pathological process is associated with an increase in the level of interleukins (cytokines - cells of the immune system synthesized by leukocytes), which can have anti-inflammatory and pro-inflammatory (mobilization of the inflammatory response) effects.
The next stages of development are disruption of blood microcirculation, infiltration (impregnation) of the vascular endothelium with leukocytes, and increased effects of oxidative stress. As a result, occlusion (impaired patency) of the arteries occurs with the formation of areas deprived of blood supply and a transition to the ischemic stage.
As a result, vascularization occurs (the formation of new elements of the vascular network), which often leads to hemorrhages in the area of the vitreous body (a gel-like, transparent substance that fills the space between the retina and the lens) and provokes the process of retinal detachment. Such violations indicate a transition to the proliferative stage.
Background angiopathy is damage to elements of the circulatory system that develops against the background of a primary disease (cardiovascular pathologies, blood diseases, head injuries, cerebral blood flow disorders, central nervous system infections). Background angiopathy, affecting the vessels that supply the retina of the eye, is a disease that is caused by a primary pathology, which makes it possible to distinguish types taking into account etiological factors:
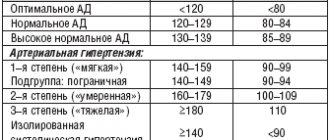
- Hypertensive. Due to a persistent increase in blood pressure.
- Hypotonic. Due to a steady decrease in blood pressure.
- Diabetic. Due to an increase in blood glucose concentration.
- Traumatic. Due to mechanical damage to tissues.
- Dysoric, also known as Morel's angiopathy. Due to deposits of amyloid (protein fractions) in the tissues of the vascular wall. Often combined with Alzheimer's disease.
Mixed angiopathy, which affects the vessels of the fundus, is diagnosed if the pathogenetic mechanisms are influenced by various factors, for example, cardiovascular pathologies in combination with a history of diabetes mellitus. Retinal neuroangiopathy means simultaneous damage to the elements of the circulatory system and the nerve fibers of the eye. Angiodystonia (decreased tone of the vascular wall due to impaired neurohumoral regulation) of the retinal arteries is a consequence of malfunctions of the autonomic system.
Traditional treatment
Due to the fact that angiopathy is just a symptom accompanying the course of various diseases, the fight against it should begin with the diagnosis and treatment of the underlying disease.
A comprehensive fight against vascular problems certainly includes drugs whose action is aimed at treating the underlying disease (the cause of angiopathy):
- sugar-lowering tablets or insulin injections for diabetics;
- for atherosclerosis or hypertension - not only means that normalize blood pressure, but also “normalize” cholesterol.
Treatment of diabetic retinopathy
If angiopathy is diagnosed in patients with diabetes, diet comes to the fore - patients should completely eliminate fatty, spicy, excessively salty and sugar-containing foods from their diet, saturate the daily menu with vegetables, fruits, cereals, herbal teas and natural juices. For diabetics with the second type of disease (non-insulin-dependent), it is very important to monitor their body weight and prevent obesity.
Patients with diabetes without manifestations of retinopathy should be observed by a retinologist and ensure that blood glucose levels (up to 6.7 mmol/l), blood pressure and glycated hemoglobin (up to 7%) are always normal.
Important: methods to preserve vision in diabetic retinopathy include:
- drug therapy;
- surgery;
- laser coagulation of the retina.
Drug treatment of diabetic retinopathy involves the injection directly into the vitreous of drugs that block vascular endothelial growth factor (anti-VEGF therapy). Their main task is to strengthen the vascular walls and prevent further hemorrhages in the retina. The most popular drugs are Ranibizumab, Bevacizumab, Aflibibercept.
Most patients require monthly injections of these medications for the first six months after starting treatment.
Laser therapy is designed to cope with retinal swelling and eliminate hemorrhages. For some patients, 1 procedure is enough to cope with the manifestations of diabetic retinopathy, while others require a whole course (or even several).
Injections of corticosteroids into the retina (Dexamethasone is most often used) complement both anti-VEGF drugs and laser surgery. True, hormonal treatment for diabetic retinopathy has several significant side effects - injections can provoke the development of glaucoma and cataracts.
As for surgery for DR, in most cases we are talking about vitrectomy (excision and subsequent replacement of the vitreous gel in the central part of the eye). The procedure can be performed under either local or general anesthesia. The direct indication for surgery is severe hemorrhage into the vitreous, which can subsequently lead to blindness.
Unfortunately, it is impossible to completely cure DR, but timely treatment measures will help stop the further development of pathological processes in the vessels and prevent their complications.
Treatment of angiopathy caused by arterial hypertension
Hypertensive retinopathy can only be combated by monitoring blood pressure levels (taking antihypertensive drugs). For rapid vision loss and retinal edema, laser therapy, injections of corticosteroids or anti-VEGF drugs (Pegaptanib, Ranibizumab) are used.
Causes
Angiopathy of the feeding arteries of the retina is a pathology that often occurs not sporadically, but against the background of a primary disease, which indicates the secondary nature of the disorders. Among the reasons that provoke the development of retinal angiopathy, it is worth highlighting the following pathologies:
- Arterial hypertension. A persistent increase in blood pressure negatively affects the condition of the vascular wall, which thickens and is penetrated by fibrous fibers. With angiopathy of hypertensive origin, narrowing and excessive tortuosity of the arterial bed is revealed.
- Diabetes. Elevated blood glucose concentrations are associated with inflammatory processes affecting the tissues of the arterial walls. The permeability of the walls increases, the liquid fraction containing blood and lymph cells seeps outside the bloodstream, which correlates with the development of edema of the tissues of the perivascular (located around the vessels) space.
- Arterial hypotension. A persistent decrease in blood pressure correlates with chronic dilation of the bloodstream and a decrease in the tone of the vascular wall.
- Injuries in the area of the organs of vision and skull. Traumatic injuries are associated with a high risk of rupture of blood vessels in the visual organs. As a result, visible foci of hemorrhage appear.
- Pathologies of elements of the blood flow system (thrombosis, vasculitis, atherosclerotic lesions).
Among the factors that contribute to the development of vascular pathologies and related disorders, it is worth noting intoxication (poisoning with ethyl alcohol, narcotic substances), blood diseases (coagulation disorders, anemia), and age over 50 years. In the presence of provoking factors, the likelihood of developing angiopathy increases.
Angiopathy: what is it?
Retinal angiopathy of both eyes (both eyes) is not an independent disease; it is always a sign of other diseases that affect the vascular system of the body, including the eyes.
It occurs in people of all ages, but is more often observed in those over 30 years of age.
Detection of angiopathy contributes to the timely recognition of certain ailments: diabetes mellitus, hypertension, carcinoid tumors, head and spine injuries, diseases of blood vessels with the formation of cholesterol on their walls. This helps to determine the necessary treatment in time.
Attention! If the disease occurs, the patient may complain of blurred vision, blurry or flickering vision, blood in the urine, pain in the legs, and nosebleeds .
Symptoms
Angiopathy of the arteries located in the retinal area is characterized by symptoms such as pathological changes in the elements of the circulatory network, which determines treatment tactics. The affected vessels dilate because the vascular wall loses its elasticity and tone. The vascular bed becomes tortuous, which, together with impaired patency, leads to a change in the speed and volume of blood flow.
Manifestations of angiopathy of the elements of the blood supply to the eyes include loss of vision, which can be partial or complete, affecting one or both organs of vision. Typically, disorders develop under the influence of provoking factors - psycho-emotional stress, physical stress. Often severe symptoms appear in the morning after waking up.
A decrease in visual acuity is often preceded by symptoms - transient visual dysfunction, short-term loss of visual fields, the appearance of foreign objects (dots, spots, sparks) within the boundaries of the visual field. Angiopathy of the vessels located in the retinal area in adults and children is manifested by the following symptoms:
- The presence of a pink, cherry-colored spot in the retinal area. The spot clearly appears against the background of the retina of a white-gray color, caused by edema of ischemic origin.
- Narrowing of arterioles (small arteries preceding capillaries) of the inner lining of the organs of vision.
- Formation of foci of intraretinal (located inside the retinal nerve sheath) hemorrhage.
In the early stages of the pathology, the disc at the base of the optic nerve is pale pink with blurry, indistinct boundaries. Later, the disc becomes pale, the borders are not visible due to swelling in the peripapillary zone of the inner eye membrane. If ischemic processes affect the entire inner membrane, the color of the papillomacular area may remain unchanged.
If the patency of the central artery or its branches is impaired, pathological changes of ischemic origin occur in the areas that supply the affected vessels. If ischemia does not extend to the macula (the central point of the retina where light rays are refracted), loss of visual fields is detected in accordance with the localization of the ischemic focus.
In cases of damage to the macular area, deterioration in visual acuity is observed. As a consequence of destructive processes, atrophy of the optic nerve tissue develops. You need to make an appointment with an ophthalmologist in cases where the following symptoms are observed:
- Frequent redness of the mucous membrane of the eyes.
- Cloudiness of the visible image.
- Feeling of pulsation and swelling inside the eyes.
- Loss of field of view.
- Pain in the visual area.
- The appearance of foreign objects and blind spots within the field of view.
If these signs appear, then you need to consult a specialist who will conduct a diagnostic examination and develop a treatment program.
Causes of retinal angiopathy in both eyes
The main types of angiopathy are the diseases that caused its occurrence.
Hypertensive
Occurs with arterial hypertension and serves as a source of damage to the veins and arteries of the eye shell.
When the pressure in the arteries increases , spasm occurs, blood clots appear, hyaline (fibrillar protein) increases in the walls of the vessels, and clouding of the eyeball occurs.
As a result, the vessels lose their strength and may rupture, resulting in hemorrhage.
The main sign of hypertension is changes in the fundus of the eye.
During its examination, you can determine:
- that the veins are not easy to see, the arteries are slightly compressed;
- arteries are narrowed and intertwined with veins;
- changes in the color and shape of arteries;
- the color of the arteries became silver.
If hypertension is treated on time, eye angiopathy will go away on its own.
Diabetic
Diabetes mellitus affects the body's blood vessels, as well as the eyes. Glucose metabolic products are deposited on the walls of blood vessels, their lumen decreases, blood circulation is disrupted, which does not provide the tissue with a sufficient amount of oxygen. This causes vision impairment.
Hypotonic
Low blood pressure is accompanied by a decrease in the degree of tension in the vascular walls. Because of this, the vessels become oversaturated with blood, and it begins to flow slowly. As a result , this contributes to the formation of blood clots . In this case, the patient experiences pulsation in the eyes.
Photo 1. Fundus of the eye with hypotonic angiopathy of the retina. The arrow indicates the formed thrombus.
Traumatic
Appears with injuries to the spine and brain. The occurrence of eye disease is associated with pinching of blood vessels in the cervical spine or with increased pressure inside the skull.
Youth
The most dangerous type of disease. The causes of this disease are not fully understood. Symptoms: vascular inflammation, hemophthalmos. Such signs can lead to complications: cataracts, glaucoma, retinal detachment and vision loss.
Diagnostic methods
The diagnosis of retinal angiopathy is made based on the results of an ophthalmological examination and instrumental examination. The main diagnostic method is ophthalmoscopy, during which the condition of the elements of the circulatory system located in the fundus area is revealed. Ophthalmoscopy shows the presence of edema of ischemic origin. Other instrumental methods:
- Visometry. Determination of visual acuity.
- Refractometry. Study of the refractive power of the optical system of the organs of vision.
- Tonometry. Determination of intraocular pressure values.
Biomicroscopic examination allows us to draw preliminary conclusions about the degree of patency of the arteries supplying the retina. With partial obstruction, a pupillary defect of the afferent type is observed (dilation of the pupil on the side of the lesion of the optic nerve tissue when the source of light stimulus quickly moves from the healthy organ of vision to the damaged eye).
In case of complete obstruction, the absence or significant decrease in the reaction of the pupil to a light stimulus is detected. At the same time, ultrasound Dopplerography of the vessels and radiography with contrast are performed (allows one to determine the speed and volume of blood flow). During neuroimaging (CT, MRI), the morphological structure and the nature of the structural changes that have occurred in the tissues of the visual organs are determined.
Diagnostics
It is virtually impossible to determine angiopathy based on patient complaints and medical history. The only way to detect defects in the fundus vascular system is to conduct a visual examination of the retina under a microscope. To do this, before the procedure, the ophthalmologist instills a solution into the eye that dilates the pupil, and then begins the examination. In the presence of pathology, dilated vessels or areas of ischemia (insufficient blood supply), pinpoint or heavy hemorrhages, and displacement of the macula are visible on the retina.
To clarify the diagnosis, identify concomitant changes and establish the extent of retinal damage, additional diagnostic methods are used:
- Ultrasound of the eyeball, combined with duplex scanning and Dopplerography, which allows you to measure the speed of blood flow, establish the localization of vessels with the lowest indicator, and also visualize the condition of the walls of the ocular arteries and veins;
- angiography of the ocular vessels - an x-ray study with contrast, which reveals places where blood flow is worsened or completely stopped;
- MRI, CT or OCT of the eye is a high-tech hardware technique that allows you to obtain a three-dimensional image of all structures of the organs of vision, on which the vessels, retina and other tissues of the eye will be visible in detail.
Sometimes, to confirm the effect of angiopathy on vision, computer diagnostics are performed for light and color sensitivity, the width of the visual field and other indicators.
Additionally, the doctor may prescribe monitoring of the functions of the cardiovascular system, blood pressure, laboratory blood tests for glucose levels, cholesterol, hormones, etc. This information will be needed to identify the main causes of the disease.
Treatment methods
Background angiopathy of the arteries supplying the retina is a pathology that can be cured if the therapeutic effect is directed at the primary disease, which will eliminate the provoking factors. Therapy is carried out with drugs:
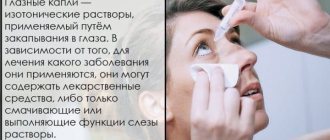
- Blood circulation stimulants (vasodilators - vasodilators, cerebral blood flow correctors, improving microcirculation - Cavinton, Actovegin). In addition to oral, intramuscular, and intravenous administration of drugs, topical drops are used - Taufon, Emoxipin.
- Statins (lower the level of lipid fractions in the blood).
- Thrombolytics (improve the rheological properties of blood).
- Angioprotectors (stimulate metabolic processes in the tissues of the vascular wall).
- Vitamins B, C, E.
To treat idiopathic angiopathy of the arteries in the retinal area, corticosteroids are prescribed - anti-inflammatory agents. Desensitizing therapy is carried out to suppress allergic reactions and autoimmune processes. At the same time, laser therapy and other methods of physiotherapy (electrical stimulation, magnetic therapy) are prescribed.
Physiotherapy methods help improve blood flow and blood supply to the tissues of the organs of vision. Surgery is indicated in the absence of a therapeutic effect after conservative treatment. Operations are performed - photocoagulation (cauterization of retinal tissue with a laser beam to close damaged vessels, suppress the progression of pathological processes), vitrectomy (partial or complete removal of the vitreous body).
How to treat
Treatment of angiopathy is selected individually and depends on the underlying disease. In this case, the patient’s age and the presence of concomitant health problems must be taken into account.
For example, if the cause of angiopathy is hidden in arterial hypertension, then it is necessary to take vasodilating drugs. When it is a complication of diabetes, blood glucose levels should be monitored using medicinal and non-medicinal means. To control the elasticity of the walls of blood vessels, it is important to adhere to a therapeutic diet. It involves the exclusion of foods rich in fiber and carbohydrates. It is recommended to eat more protein foods.
Treatment should be carried out comprehensively and only under the supervision of specialized specialists (ophthalmologist, endocrinologist). It includes not only taking medications, but also physiotherapy and local therapy.
Drug treatment
Retinal angiopathy can be treated at home. It is only necessary to follow the dosage of the medications prescribed by the doctor and the time of administration. Conservative therapy involves taking medications from the following groups:
Important information: Focal (arterial) hyperemia of the gastric mucosa
The standard course of treatment is 2-3 weeks. It is repeated twice a year.
Eye drops
For atherosclerosis of the retina, treatment always includes the use of drops. They can be fortified (Lutein Complex) or vascular (Taufon). Such drugs help improve blood microcirculation in the eyeball.
Physiotherapy
Treatment of retinal angiopathy is not complete without physiotherapeutic procedures. They enhance the effect of taking medications. Well proven in this matter:
- Acupuncture. Prescribed to patients whose angiopathy is caused by trauma, hypertension or hypotension.
- Magnetotherapy. Promotes activation of blood circulation, reduces tissue swelling, eliminates pain. The only contraindication is the patient’s history of hypotension.
- Laser irradiation. The main goal of this treatment is blood purification. It is recommended for diabetic types of angiopathy.
The procedures should be carried out in a course. Each consists of 10-15 sessions.
Folk remedies
Traditional medicine recipes are used as an auxiliary therapeutic measure. However, before starting such treatment, you should consult your doctor. Some infusions and herbs can do more harm than potential benefit.
A decoction prepared using St. John's wort and chamomile has a positive effect on angiopathy. Mix a teaspoon of dry plants in one container and pour 0.5 liters of boiling water, let it brew under the lid. The product should be divided into 2 servings. It is recommended to consume the first one in the morning on an empty stomach, and the second one before bedtime. The course of treatment is 30 days.
Prevention
Preventive measures include quitting smoking and abusing alcoholic beverages, organizing a healthy diet, regular, dosed physical activity, walking in the fresh air, and an active lifestyle. To prevent the development of eye diseases, it is important to visit an ophthalmologist at least once every year.
Angiopathy of the arteries supplying the retina is a disease that must be treated promptly to avoid complications such as decreased visual acuity and blindness.
Why does it happen
The disorder can appear at any age, but is most often diagnosed after 30 years of age. For conservative treatment methods to be effective, it is necessary to identify hidden disorders that contribute to spasms and decreased tone of the vascular walls. The following diseases are potential causes:
Important information: How to treat chronic idiopathic myelofibrosis and its symptoms
- diabetes;
- systemic vasculitis;
- atherosclerosis of the ocular vessels;
- hypertonic disease;
- cardiopsychoneurosis;
- scoliosis;
- cervical osteochondrosis.
The following factors are considered predisposing to retinal vascular angiopathy:
- smoking;
- elderly age;
- congenital vascular anomalies;
- mechanical damage and trauma to the retina;
- intoxication of the body;
- long-term use of medications;
- blood diseases;
- high intracranial pressure.
To eliminate the high risk of angiopathy, it is enough to eliminate the listed factors from life.
Diagnosis of the disease
Retinal angiopathy of the hypertensive type in the initial stages is most often diagnosed during a routine examination in the ophthalmologist's office. During an examination of the condition of the fundus by a specialist, a small spot in the shape of an oval or circle may be detected. It is usually located where the optic nerve enters the retina of the eye.
The progress of the disease is accompanied by an increase in the size of the nerve, as a result of which the shape of the spot is distorted and uneven edges appear. The blood circulation system is disrupted, the size of the eye arteries decreases, as a result of which floaters or a veil appear in the spectrum of visual perception.
Diagnosis and treatment
Pathology can be detected by chance - during a medical examination. Or when monitoring the underlying disease - diabetes, hypertension, low blood pressure.
The doctor checks the fundus of the eye with a special apparatus and evaluates the condition of the retina and blood vessels in both eyes. If you suspect angiopathy, you will also need an ultrasound, magnetic resonance imaging, and x-ray of blood vessels (angiography).
Therapy for retinal angiopathy should be carried out in conjunction with eliminating the source - the underlying disease. Therefore, each type of angiopathy has its own treatment algorithm.
In addition to drugs that correct the underlying disease, the following are prescribed:
- Medicines to improve blood circulation and strengthen the walls of blood vessels in the eyes (Actovegin, Trental, Kaviton, Emoxipin);
- Medicines that reduce vascular permeability (Dobesilate, Parmidine);
- Vitamin complexes to restore vision and strengthen capillaries;
- Blood thinning drugs (Agapurin, Curantil, Persantine);
- Drops that improve microcirculation (Taufon, Emoxipin);
- Physiotherapeutic measures (infrared laser radiation, magnetic therapy, acupuncture).
As maintenance therapy, plant extracts and decoctions of chamomile flowers, lemon balm and St. John's wort leaves, and hawthorn flowers and fruits can be used.
If the pathology of the retinal vessels has led to irreversible consequences, surgery will be required. One of the fastest and most effective methods of such treatment is laser coagulation. The procedure is performed under local anesthesia and takes only 20 minutes. As a result, the damaged vessels fuse with the retina.
Recommendations for patients with angiopathy
You can significantly increase the effectiveness of treatment, reduce the risks of complications and the likelihood of further progression of angioneurosis by following the following recommendations:
- The diet must include a sufficient amount of foods that are natural sources of vitamins and substances necessary for the proper functioning of the visual apparatus and blood vessels of the fundus (chicken and quail eggs, vegetables, herbs, lettuce, offal, butter, sour cream, nuts, etc. .).
- Self-massage of the cervical-collar area should be performed regularly, unless there are contraindications (such massage has a positive effect on blood circulation in this area and prevents compression of nerve endings due to myofascial syndrome).
- When there is increased stress on the eyes (working at a computer, long reading, activity in poorly lit rooms), it is necessary to perform therapeutic exercises for the eyes.
- When engaging in traumatic sports, it is necessary to protect your eyes from damage.
Natural sources of vitamins for the eyes
It is necessary to visit an ophthalmologist for early detection of pathological changes in the fundus every year (for patients with diabetes mellitus - at least 2-3 times a year).
Retinal angiopathy is a vascular pathology that can provoke more severe ophthalmological disorders and, with a progressive course, lead to low vision and complete blindness. The maximum risk of angiopathy is present in patients with arterial hypertension, diabetes mellitus, endocrine disorders and heart disease. Treatment in the initial stages is medicinal and can be supplemented with physiotherapeutic methods. In severe cases and in the presence of complications, microsurgical or vitreoretinal intervention is indicated.
Angiopathy in diabetics
In diabetes, this disease develops most often (angiopathy of the hypertensive type is in second place), so you need to be very careful. It is the cause of blindness in diabetics under 65 years of age. The reason for this increase is due to a constant increase in blood glucose levels, which leads to pathologies in the structure of blood vessels throughout the body.
A gradual loss of vision will be caused by the development of occlusions and blood penetration into the tissues of the retinas of both eyes, resulting in the formation of infiltrates and hemorrhages. With diabetes, there are a number of factors that can increase the likelihood of developing the disease:
- kidney disease;
- pregnancy;
- deadlines. If the disease has lasted for more than 7 years, the probability increases, but it can occur earlier if the patient does not adhere to the basic rules and recommendations of the doctor;
- smoking;
- pressure (increased).
Angiopathy in pregnant women
It occurs quite often when carrying a child, but it cannot be said that cases are extremely rare. But it is more harmless and can go away on its own 3 months after childbirth. The disease occurs due to an increase in the volume of blood that circulates throughout the body. This will not harm either the mother or the child.
But, if the mother was sick before the fetus was conceived, especially with diabetic or hypertensive angiopathy of the retina of both eyes, then complications or development of the disease are possible. It is imperative that you regularly go for preventative examinations to an ophthalmologist throughout your pregnancy to keep the situation under control. When there is a threat of retinal detachment, doctors may prescribe artificial birth.
Treatment of angiopathy
Treatment of retinal angiopathy of both eyes should always be carried out only as part of complex measures in relation to the underlying disease. In the absence of such an approach, treatment will have low effectiveness, and the likelihood of improvement is almost zero.
Treatment of hypertensive angiopathy
To reduce the effects of ischemia, vasodilators are used, which have a selective effect - they affect only the vessels of the eyes and brain. Such drugs include:
To reduce signs of oxygen starvation, inhalations with oxygen or carbogen are often used; they can significantly expand the cerebral and retinal vessels.
To reduce blood viscosity and improve its fluidity, antiplatelet agents are prescribed (Agapurin, Clopidogrel, xanthinol nicotinate, Curantil, Persantine); To protect blood vessels from free radicals and lipid oxidation products, antioxidants (alpha-tocopherol, ascorbic acid, Veteron, Divertin) and angioprotectors (Doxium) are used. To resolve foci of hemorrhage, it is advisable to prescribe enzymes (Wobenzym, Papain, prourokinase).
Treatment of angiopathy using low-energy infrared laser radiation has also proven effective.
Treatment of diabetic angiopathy
First of all, treatment should begin with the correction of diabetes mellitus (normalization of hyperglycemia, lipid metabolism, blood pressure, body weight) and bringing all the main indicators to normal levels. It is very important to start treatment before the point of “no return” occurs—the moment when neovascularization begins in the retina and irreversible changes occur.
The main method of treating diabetic retinopathy is laser coagulation of the retina; drug therapy for this condition is ineffective. Laser coagulation before the onset of neovascularization occurs practically without complications and in most cases additional treatment is no longer required; moreover, a reverse development of existing changes is observed.
Treatment
structure of the eye with angiopathy
Therapy depends on the characteristics of the body and accompanying ailments. When prescribing medications, the doctor also takes into account the degree of the disease. You can learn more about the treatment of amblyopia in adults here.
The goal of drug therapy is to eliminate factors that contribute to the development of angiopathy.
If the disease occurs against the background of hypertension, you should take medications to lower your blood pressure. If angiopathy is associated with diabetes mellitus, the endocrinologist prescribes drugs to stabilize glucose.
Therapy for the disease that has become the root cause must be comprehensive. If necessary, you need to contact a rheumatologist or cardiologist.
Taking medications
- For treatment, the doctor prescribes medications that help strengthen small veins.
- It is recommended to take vitamins B, C and E.
- Magnicor is recommended for the prevention of blood clots.
- To restore microcirculation, Taufon should be used (dosages vary individually).
Depending on the stage and symptoms of the disease, physiotherapeutic procedures may be prescribed, and acupuncture is effective. If treatment does not give satisfactory results and the disease progresses, the doctor prescribes surgery. Laser coagulation of the retina is performed; an alternative to the procedure may be vitrectomy. If an advanced stage of the pathology is diagnosed, blood purification is prescribed. Timely treatment allows you to maintain visual acuity. The treatment of angiopathy requires an integrated approach. Why allergies occur on the skin around the eyes can be found in our article.
Use of folk remedies
angiopathy due to hypertension
- The following medicine is used to improve vascular tone. Take washed, peeled valerian root, mix it with lemon balm leaves (the optimal amount of the mixture is 30 g). You need to pour 150 ml of boiling water into this mixture, wait for it to cool, boil in a water bath for 10 minutes, then strain and cool. The infusion should be drunk 2 times a day for 15 days.
- To strengthen vascular tone, take 20 g of horsetail, the same amount of knotweed and hawthorn. Twenty grams of the mixture is poured with 200 ml of boiling water. The medicine is infused for 30 minutes, taken 1 tbsp 4 times a day (preferably taken on a lean stomach).
- Another effective remedy is parsley juice. It is necessary to grind the product, squeeze out the juice and take 1 tsp 2 times a day.
Prevention of angiopathy
In order to maintain blood vessels, including the eye ones, in normal condition, it is important to follow simple rules:
- Lead a healthy lifestyle. This is also necessary to correct and prevent the development of hypertension, diabetes, and other diseases that provoke angiopathy;
- Monitor chronic diseases, undergo treatment courses, and do not neglect them;
- Carry out an annual preventive examination with an ophthalmologist, even if there are no obvious vision problems;
- If there are risk factors (illness, hazardous work, old age), it is better to visit an ophthalmologist at least once every six months;
- If angiopathy is detected in pregnant women, a cesarean section is prescribed to avoid retinal detachment.
The eyes are an important organ, without which we would not be able to receive so much information and impressions about the world. Advanced retinal angiopathy can deprive a person of a normal life and make him disabled. Therefore, any, even minor, visual impairments should be corrected in a timely manner by a specialist. And such serious diseases as diabetes and hypertension should be kept under constant control.
Retinal angiopathy: diagnosis
Diagnostic studies for this disease are aimed at identifying any pathological changes in the blood vessels of the eye, the presence of blood clots in them, determining the thickness of their walls and their location. To do this, the ophthalmologist conducts comprehensive diagnostic studies, which include the following:
- taking anamnesis;
- visometry - determination of visual acuity and its impairments;
- tonometry - changes in IOP and determination of its compliance with the norm;
- ophthalmoscopy - assessment of the condition of the retina, identification of the affected area and its size;
- biomicroscopy—studying the state of the PGC structures;
- perimetry - determination of the boundaries of the field of view;
- OCT - examination of eye tissue;
- angiography is a study of the condition of the blood vessels of the retina.
Retinal vascular angiopathy - what is it?
The retina of the eyes requires a large intake of nutrients and oxygen because it is responsible for capturing light waves, converting them into nerve impulses and transmitting them to the brain, where image formation takes place. Insufficient blood supply to the choroid causes serious visual impairment. Retinal vascular angiopathy is not a separately occurring disease, but a pathology that develops as a result of the destruction of blood vessel cells and disruption of their functions in diseases of various origins.
Retinal vascular angiopathy is a pathological disorder of the tone of the blood vessels and capillaries of the fundus. As a result, their tortuosity, narrowing or expansion occurs. There is a change in the speed of blood flow and a failure of nervous regulation. Vascular defects make it possible to suspect and diagnose the underlying disease before its clinical manifestations.
This type of pathology signals the presence of a disease in the body that interferes with normal blood circulation, affects the tone of small and large vessels, causes necrotic lesions in a certain area of the retina, and threatens complete or partial loss of vision or a decrease in its quality. Angiopathy is more common in adult patients (over 35 years of age) against the background of chronic diseases, but is sometimes diagnosed in childhood, and even in newborns.
Reasons for the development of the disease
Angiopathy develops against the background of vascular pathologies, so the reasons for the development of the disease are the risks that provoke vascular diseases:
- age from 30 years,
- smoking,
- alcoholism,
- pathological conditions of pregnancy,
- overweight,
- systematic intoxication (when working in toxic industries, during treatment),
- congenital disorders,
- diabetes,
- atherosclerosis,
- osteochondrosis and scoliosis,
- inflammation of the vascular wall,
- blood diseases and so on.
Research methods
Source: doctorcardio.ru The vessels of the fundus and their condition are of important diagnostic importance.
Most often, a mirror ophthalmoscope is used in a clinic setting. This is a concave mirror with a hole in the center. This shape makes it possible to collect and direct a beam of light through the pupil dilated with the help of special drops onto the retina. A more detailed study is carried out using fluorescent vasography. A special substance is injected into the bloodstream. It spreads throughout the bloodstream. Fundus vasoconstriction can be detected and photographed in great detail using contrasting light of specific wavelengths.
Angiopathy is diagnosed with a comprehensive ophthalmological examination. The main diagnostic method is various options of ophthalmoscopy - examination of the fundus.
Diagnosis and treatment of retinal angiopathy should be carried out by a highly qualified specialist. In case of angiopathy, the doctor always prescribes drugs that improve blood circulation in the vessels of the eyeball: pentilin, solcoseryl, trental, vasonit, arbiflex, emoxipin and others.
These drugs increase the bendability of red blood cells, which helps normalize blood flow in the capillaries. For patients with fragile vessels, calcium dobesilate is prescribed. The drug thins the blood, significantly improves blood circulation in the vessels, and normalizes the permeability of the vascular walls.
What does the doctor see?
Angiopathy is characterized by a violation of the lumen of blood vessels or their course: they can be narrowed, dilated, tortuous, congested, etc., depending on the reason that caused their change.
The disease usually develops in both eyes at once. In complicated situations, pathological changes in the retina and/or optic nerve head are determined.
According to indications, additional examination methods are carried out: computer perimetry, optical coherence tomography of the central zone of the retina and optic nerve, ultrasound scanning of intraocular structures.
The disease is diagnosed by an ophthalmologist after taking into account the symptoms of retinal angiopathy and a general examination of the patient.
In order to clarify the diagnosis, special studies are used, such as ultrasound scanning of blood vessels (carried out to obtain information about the speed of blood circulation and study the condition of the walls of blood vessels) and X-ray examination (carried out by injecting a radiopaque contrast agent).
Also, if necessary, magnetic resonance imaging is used, which makes it possible to clearly determine the structure and condition of soft tissues.