Deforming arthrosis of the hip joint in medical classifications it is identified with coxarthrosis and osteoarthrosis. The development of pathology is facilitated by degenerative-dystrophic changes in cartilage tissue. Arthrosis is included in the group of the most common chronic pathologies that damage joints. People who have crossed the 40-year mark are susceptible to the disease. The female sex is more predisposed to painful abnormalities than the male sex.
Causes of the disease
Arthrosis is a chronic disease that gradually progresses, destroying the structure of joint, bone and cartilage tissue.
In this case, we are considering specifically damage to the hip joint, while the disease that has developed in this part of the body has the specific name coxarthrosis. According to experts, this particular type is one of the most common not only among the types of diseases of the same group, but also among diseases of the musculoskeletal system. It leads to degenerative changes in diarthrosis, both its dystrophy and nearby tissues, therefore it is a dangerous and serious illness that can significantly affect all areas of human life. That is why it is very important to promptly identify and apply immediate treatment for arthrosis of the hip joint.
https://www.youtube.com/watch?v=baIw-jnAqUo
The primary symptoms that may occur with the development of arthrosis of the ball-shaped hip joint are similar to some symptoms of other hip ailments; however, in any case, it is necessary to undergo an examination by a specialist to identify what causes discomfort. The primary signs are:
- Unpleasant sensations in the thigh that get worse. Pain can occur both during intense physical activity with arthrosis of the hip joint, and after it, and in a calm state;
- Weakening of the muscles in the affected area;
- Stiffness when making movements, when raising and lowering the leg;
- The appearance of external symptoms of inflammation: redness, swelling, swelling.
- A slight crunching sound is heard, which gradually becomes louder.
Arthrosis of the multiaxial hip joint at the initial stage does not cause severe pain; it is not characterized by obvious, acute symptoms over a long period of time. That is why people do not pay due attention to these “minor problems”, they hesitate and completely delay the time of meeting with a doctor, until their health and situation worsen. This should not be done under any circumstances, because arthrosis responds most successfully and positively to therapy at the initial stage of development.
Prerequisites for the development of coxarthrosis are obesity, increased physical activity, a sedentary lifestyle, metabolic disorders, hormonal disorders, kyphosis, scoliosis, and flat feet.
Diagnostics
The diagnosis of coxarthrosis is established by the attending physician based on the patient’s complaints and examination.
However, with arthrosis of the 1st degree, the symptoms and objective changes in the affected hip joint are so insignificant that additional examination is necessary to confirm the diagnosis:
- Radiography. Coxarthrosis is characterized by narrowing of the joint space and the formation of osteophytes. However, these changes can be present in many older people without causing any symptoms of coxarthrosis. However, in many patients who complain of severe pain in the hip joints, it is not possible to detect pronounced signs of arthrosis using radiography. Therefore, doctors always evaluate the data of this examination in combination with symptoms and the results of an objective examination.
- Magnetic resonance imaging. This method allows you to obtain a more detailed image of the hip joints and visualize soft tissues, including ligaments, tendons and muscles. In most cases of coxarthrosis, magnetic resonance imaging is not needed. It is indicated if the patient is suspected of having other diseases of the hip joint that cannot be diagnosed using radiography.
- Blood analysis. Blood tests cannot diagnose coxarthrosis, but they can help rule out other joint diseases, such as gout or infectious arthritis.
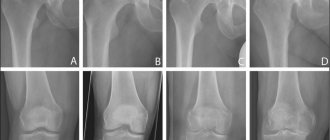
Comparison of radiographs of a healthy joint and a joint affected by coxarthrosis
Description of the pathology
Not only diseases provoke the development of coxarthrosis of the hip joint. There are a number of provoking factors that lead to these pathological changes:
- Factors associated with heredity. There are many diseases that are passed on from generation to generation. Among them, autoimmune pathologies (collagenoses) are often encountered, in which connective tissues (ligaments, bones, joints) are affected: dermatomyositis, Stickler-Wagner syndrome, scleroderma, periarteritis nodosa.
- Age is one of the most important factors that causes the appearance of symptoms of coxarthrosis of the hip joint. In young people under 35 years of age, the pathology is diagnosed extremely rarely. According to American statistics, in people between 40 and 45 years of age, pathology is found in an average of 2.5% of the state population. But in people over 65 years of age, arthrosis of the hip joint is diagnosed much more often. Every third patient from the age category of 45-65 years suffers from this disease. And in older people (over 65 years old), the risk of developing coxarthrosis increases to 75-80%! Almost all older people have some symptoms of pathological changes in the tissues of the joints. There is a fairly high probability that this could be arthrosis of the hip joint.
This congenital pathology has already been discussed, but sometimes dysplasia practically does not manifest itself in any way, and a person learns about its presence only after some diagnostic tests, for example, radiography. When coxarthrosis is detected in these patients, this pathology is diagnosed as dysplastic. In most cases, it occurs in the female population, and the age of patients varies between 25-55 years.
The degenerative process occurs against the background of a decrease in physical activity, which provides the joint with full functionality. As for young women, this is associated with pregnancy and the postpartum period. And in adulthood and old age, for most women, physical activity decreases after retirement.
Treatment methods
Treatment of coxarthrosis cannot completely restore the structure and functioning of the affected hip joints, even if it is started in a timely manner and carried out correctly.
However, with proper and early treatment, it is possible to slow down or stop the progression of the pathological process and improve joint mobility.
Typically, for grade 1 coxarthrosis, a conservative approach is used, including:
- Lifestyle changes.
- Therapeutic exercise.
- Drug therapy.
- Traditional medicine is quite popular.
At this stage, the disease is practically not curable with the help of intra-articular injections and surgery.
Lifestyle change
The following changes play an important role in slowing the progression of coxarthrosis and reducing the frequency of exacerbation of its symptoms:
- Reduce or eliminate any physical activity that leads to the appearance or worsening of symptoms of arthrosis and can deform the joint. For example, don't walk up stairs, lift heavy objects, or play football or hockey.
- Rest your joints if they experience pain. The appearance of even mild pain in the hip joint indicates that it needs rest.
- Normalize your weight. The load on the hip joints increases exponentially with weight gain - for every 1 kg of added excess body weight, the load on the hip joint increases by 6 kg. Normalizing weight is the simplest and most effective way to reduce the frequency of symptoms of coxarthrosis and slow down its progression.
If pain occurs in the hip joint due to coxarthrosis, apply ice wrapped in a towel to it for 15–20 minutes. This will reduce swelling of damaged tissues and reduce the intensity of pain.
Special hip and thigh belt with ice pack insert
Physiotherapy
Physical therapy (physical therapy) helps prevent further progression of the disease. Gymnastics for coxarthrosis maintains muscle strength and flexibility, thereby reducing the load on the affected hip joint.
The most effective exercise program is one individually developed by an experienced physical therapy doctor.
However, any patient with coxarthrosis benefits from light gymnastic exercises, swimming and walking; physical activity promotes weight loss, which also has a positive effect on the condition of patients with hip arthrosis.
Examples of exercises for coxarthrosis
Drug therapy
To treat grade 1 coxarthrosis with medications, the following are most often used:
- Painkillers (paracetamol) and non-steroidal anti-inflammatory drugs (NSAIDs: ibuprofen, diclofenac, naproxen). Medicines are taken only in the presence of pain. These drugs are produced in the form of tablets for internal use, ointments or creams for external application to the joint area, solutions for intramuscular or intravenous administration.
- Chondroprotectors – glucosamine, chondroitin sulfate. These substances are a natural part of articular cartilage. Their use promotes the regeneration of damaged cartilage tissue, due to which the development of arthrosis slows down and its symptoms subside.
Traditional medicine
Many patients are interested in how to treat grade 1 coxarthrosis of the hip joint using traditional medicine.
The effectiveness of not a single traditional medicine recipe has been tested in scientific research, so each patient uses them at his own peril and risk. Most doctors have a negative attitude towards such treatment, preferring gymnastics and medications for coxarthrosis.
Here are some popular recipes for home remedies used to treat joint diseases:
- Coat cabbage leaves with honey and apply to the sore joint overnight. Place plastic wrap and woolen cloth over the compress. In the morning, remove the compress, wash the skin and apply a new one, which should be worn until the evening. The course of treatment lasts 1 month.
- Grind 5 lemons, 250 g of celery and 120 g of garlic in a meat grinder. Place the mixture in a three-liter jar and fill it completely with boiling water, then close the lid and wrap it in a blanket overnight. Drink 70 ml of this decoction every day 30 minutes before meals for 3 months.
- Pour 8 tbsp. l. crushed celandine herb 1 liter of olive oil, let it brew in a warm place for 2 weeks. Then strain and rub the oil into the skin over the affected joint 3 times a day for a month.
Ingredients for cabbage and honey compress
Symptoms 1 2 3 degrees of arthrosis of the hip joint
If you are wondering where this disease came from, you need to carefully study the reasons that could provoke arthrosis of the hip joint. According to origin, primary and secondary arthrosis are distinguished.
In the primary type, arthrosis in the hip area develops due to the following reasons:
- Unknown and undetectable causative factor;
- Natural age-related changes;
- Predisposition at the genetic level;
- The presence of congenital pathologies of the musculoskeletal system.
The causes of secondary coxarthrosis, which can lead to its development at any age, are the following unfavorable factors:
- Injuries of varying severity;
- Increased physical activity;
- Poor nutrition;
- Inactive lifestyle;
- Improper therapy and recovery after long-term hip injuries;
- Infectious diseases and viral inflammations (arthritis, coxitis);
- Excess weight, obesity;
- Presence of diseases of the endocrine system.
Depending on the nature of the destruction, the intensity of symptoms and complications, the development of arthrosis of the lower extremities of the hip joints is classically divided into three degrees.
The duration of the disease at stage 1 can be quite long. At this time, significant changes are not observed, and accordingly the symptoms are mild or absent. A characteristic feature is the appearance of pain after or during physical activity, and it can be localized not only in the area of the hip joint, but also down to the knee.
Arthrosis in the initial 1st degree of minor damage to the hip joint is no longer characterized by any obvious symptoms. But on an x-ray, the doctor can already see a narrowing of the joint space, as well as the appearance of minor growths due to bone growth. The peculiarity is that such primary symptoms, as a rule, affect the work exclusively of those structures that are located deep inside the limb, so at first a person may not even be aware of arthrosis of the hip joint and its steady progress.
We invite you to familiarize yourself with: Effective methods of treating arthrosis of the knee joint with folk remedies
The next stage in the development of the disease openly announces itself with the manifestation of pronounced symptoms and their gradual complication. At the 2nd stage of development, arthrosis actively destroys the structure of not only the connective and cartilaginous tissue of the hip joint, but also the muscle tissue. She loses tone and strength, so it becomes difficult to move the limb.
Movement is accompanied by intense pain, which at rest does not subside as quickly as before, or turns into a long-lasting, mild, aching pain. Walking becomes problematic; if you need to walk for a long time, cramps, muscle spasms and lameness begin to appear. X-ray images show distinct destruction and changes, an increase in growths on the bone, deformation of the head of the hip joint, changes in its size, and, as a result, a narrowing of the gap.
In the picture (right): severe destruction of the cartilage and very large osteophytes are noted.
Arthrosis, which has developed to degree 3, is characterized by constant and intense pain, not only in the hip joint, it can spread higher to the lower abdomen, or to the leg to the knee. Often unbearable pain does not give rest around the clock, or sharply intensifies at night.
It is no longer possible to move without support at this stage, since the muscles of the limb atrophy and the affected leg shortens, which significantly worsens the patient’s position. X-rays demonstrate the disappearance of the joint space, which is caused by a large-scale growth of bone tissue; the previously mobile diarthrosis turns into a single immovable hardened structure.
If a patient has been diagnosed with arthrosis of the hip joint at any stage of development, he immediately wonders how to relieve the main disturbing symptoms and what kind of treatment to apply. This question is indeed very important, because the correct use of healing methods can bring significant relief and improve the patient’s health. Therefore, let's look carefully at how, with what and by what method arthrosis can be cured at different stages of destruction of the hip joint.
There are two broad treatment methods: conservative and surgical. Therapeutic or conservative - offers to restore and alleviate symptoms without surgical intervention, and with surgical intervention in this case everything is absolutely clear. First, let's look at the conservative methods used to treat arthrosis of the hip joint.
It is considered the most effective, fast-acting, proven and popular method of treating coxarthrosis. It is aimed at relieving or completely eliminating pain and inflammatory syndromes, slowing down the processes of destruction, igniting blood circulation and stimulating nerve endings, the weakening of which deprives joint tissues of the ability to nourish themselves.
Nonsteroidal anti-inflammatory drugs and analgesics are usually used together. Arthrosis of the multiaxial hip joint, which has developed, for example, to degree 2, usually cannot be managed without the use of such drugs. But we should not forget that it only relieves symptoms, but treatment and restoration of diarthrosis does not occur at this time, the disease gradually progresses further. The following NSAIDs and painkillers are used: Etodolac, Ketoprofen, Lornoxicam, Indomethacin, Aspirin and others.
Hormonal medications and corticosteroids are used if arthrosis has destroyed most of the hip joint, usually this occurs with the transition to 3 degrees of development. At this time, the treatment of acute symptoms with the above group of drugs no longer works, therefore stronger ones are used: Kenalog, Hydrocortisone, Flosterone. Most often they are prescribed as an injection, twice a year.
Physiotherapy
Hip arthrosis and its main symptoms can be gradually cured with physical therapy. Many people underestimate this treatment method, but in fact, it is one of the most effective, especially if it is part of a therapeutic complex.
Doctors usually give a referral for a course, which consists of several procedures, such as:
- Magnetic laser treatment, which has a rehabilitative effect;
- Ultraviolet irradiation, which relieves pain;
- Darsonvalization, which thins and stimulates blood flow;
- Centimeter wave therapy, which has a calming effect and relieves severe inflammation;
- Electrophoresis, used simultaneously with painkillers for external use;
- Massage, manual influence on the affected part of the body.
Arthrosis of the hip joint, as well as its secondary advanced symptoms, can be weakened and gradually eliminated with the help of proper, light and simple physical activity and activity, the most important condition is regularity of exercise and a reasonable approach to the load. For example, such banal exercises as swings, when performed slowly and smoothly, speed up treatment by strengthening and toning the ligamentous apparatus and muscles. In the photo you can see how to swing from side to side; 15 times will be enough for each leg.
Another simple but useful exercise against coxarthrosis is the following: get on all fours on the floor, slowly lift one leg to the side and lower it down. Repeat on each leg 10-15 times.
To perform the next exercise, lie on your back, bend your knees, grab the knee of one leg with your hands and, without sudden movements, gently pull it to your chest, hold in this position for 30 seconds and lower the limb. Repeat for the other leg.
Arthrosis of the hip joint, precisely at the initial 1st stage of development, responds well to treatment with physical education. This method certainly has a general strengthening effect, helps tone muscles and accelerates the blood, improving nutrition and enriching cells with oxygen.
Treatment of any stage of arthrosis of the hip joint is accompanied by changes in the nutritional system and daily diet. The diet for this disease cannot be called too strict, but restrictions or prohibitions are still introduced on the consumption of such products as:
- Sweets, flour and sugar;
- Salt, hot pepper, seasonings in large quantities;
- Alcoholic drinks;
- Fatty types of meat, fish, cheese;
- Fast food;
- Smoked meats and semi-finished products;
- Sour fruits.
Doctors recommend adhering to a proper, rational and healthy diet, which involves eating food at a certain time, not overeating, and eating foods rich in minerals, vitamins and microelements. To have a chance to cure arthrosis of the hip joint, the basis of the diet should be cereals, porridges, vegetables, both raw and cooked, fermented milk products of medium and low fat content, seasonal fruits, seeds and nuts, berries, lean fish and meats in baked, boiled and stewed.
The clinical picture of arthrosis directly depends on the stage of the disease. First, a person begins to feel slight discomfort in the groin and morning stiffness of the leg, but swelling and swelling of the soft tissues does not occur. As the pathology develops, an acute period begins, characterized by intense pain.
We suggest you read: Tendinitis of the patellar ligament, causes, symptoms and treatment
The main complaint of all patients is pain and limited mobility. Their severity depends on dystrophic changes in cartilage.
There are 3 degrees of the disease:
- At grade 1, only discomfort occurs after prolonged physical activity (climbing mountains, running, cycling), which goes away on its own after rest. The muscles are toned, movements are not limited. On an x-ray, you can notice a narrowing of the joint space.
- At grade 2, pain begins that radiates to the groin area, spreading to the buttock and the front surface of the thigh. “Starting” pain occurs when trying to stand up or start walking, which goes away after 2-3 minutes. After prolonged exercise, the pain intensifies and goes away with rest. A sign of arthrosis is a characteristic crunch in the joint, movements are limited (hip abduction), muscle strength decreases, and when pain occurs, a spasm of smooth muscles occurs. The x-ray shows small osteophytes that are located along the edges of the bone areas of the joints. The femoral neck is thickened and widened, the joint space is significantly narrowed.
- At stage 3 of the disease, pain is constant and does not subside even at rest. When walking, patients use improvised objects (cane, crutch). The muscle tissue of the thigh and lower leg atrophies, the limb shortens - in order to reach the ground, the patient is forced to stand on his fingertips. The x-ray shows massive osteophytes, the femoral head is flattened, and the joint space is practically invisible.
Stages of osteoarthritis of the hip joint
The disease is classified into 3 stages, depending on the X-ray and magnetic resonance imaging. Let's look at what features are characteristic of each stage.
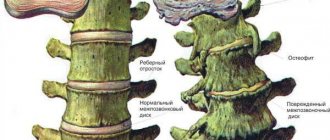
- It is extremely rare to catch stage 1 in practice, since patients usually do not go to a medical facility for examination in the initial period, not counting periodically mild discomfort in the joint as a serious pathology. But it is an achievable task to detect early pathogenesis using X-ray examination. The clinical picture on x-ray is as follows: slight narrowing of the joint space, small calcifications (pointwise) along the outer and inner edges of the acetabulum, sharpening in the area of the fossa of the spherical component of the femur. No serious deformations of the articular surfaces are detected, the condition of the hyaline cartilage is satisfactory.
- At stage 2 of osteoarthritis of the hip joint, a progressive reduction in the level of the joint space is determined (the clearance decreases by 45% of normal). The second stage is also characterized by subluxation of the femoral head and moderate subchondral sclerosis. Additionally, pronounced osteophytosis with large bone growths along the marginal line of the acetabulum and along the periphery of the femoral head, significant tuberosity and roughness of cartilage tissue, protrusion of the pelvic bed, exposure and moderate deformation of the articular surfaces are diagnosed. In some cases, bone cysts and chondromic bodies free in the joint are detected.
- For stage 3, a characteristic sign is a critically small lumen of the joint space or complete closure of the space between the articular surfaces. This stage is extremely severe, disables the person, and therefore surgical treatment is unconditionally required. Based on the results of radiography and other leading diagnostic methods, generalized necrosis of the head, maximum disappearance of cartilage tissue from the surfaces of the joint, giant osteophytes of various shapes and sizes, advanced sclerosis and cystic reconstructions of bone tissue are detected. The next signs are a critical condition of the acetabulum with an abnormally large depression, which is caused by severe osteophytosis; subluxation/dislocation of the hip, reduction in size and deformation of the femoral head with loss of rounded shape.
Dynamics of disease of large joints of the lower extremities.
Many people are interested in how the concept of “deforming osteoarthritis” differs from the concept of “osteoarthrosis”? We answer: nothing, both medical diagnoses refer to the same pathology, the outcome of which is deformation of the joint and periarticular structures. That is, the word “deforming” simply emphasizes the deforming properties typical of pathology.
Characteristic symptoms and signs
The leading symptoms of arthrosis of the hip joint are pain when walking in the hip area, radiating to the groin and knee joint. A person suffers from stiffness of movement, stiffness, especially in the morning. To stabilize the joint, the patient begins to limp and his gait changes. Over time, due to muscle atrophy and joint deformation, the limb is noticeably shortened.
Arthrosis of the first severity is characterized by periodic pain that occurs after intense physical activity. They are localized in the articulation area and disappear after a long rest.
With arthrosis of the second degree of the hip joint, the severity of the pain syndrome increases. Discomfortable sensations occur even at rest, spread to the thigh and groin, and intensify with lifting weights or increasing physical activity. To eliminate pain in the hip joint, a person begins to barely noticeably limp. There is a limitation of movements in the joint, especially during abduction and internal rotation of the hip.
Arthrosis of the third degree is characterized by constant severe pain that does not subside during the day and night. Difficulties arise when moving, so when walking a person is forced to use a cane or crutches. The hip joint is stiff, there is significant atrophy of the muscles of the buttocks, thighs, and legs.
Due to the weakness of the abductor muscles of the femur, the pelvic bones are displaced in the frontal plane. To compensate for the shortening of the leg that has occurred, the patient bends towards the injured limb when moving. This provokes a strong shift in the center of gravity and an increase in loads on the joint. At this stage of arthrosis, severe ankylosis of the joint develops.
| Degrees | Radiographic signs |
| First | The changes are not pronounced. The joint spaces are moderately, unevenly narrowed, there is no destruction of the surface of the femur. Minor bone growths are observed on the outer or inner edge of the acetabulum |
| Second | The height of the joint space is significantly reduced due to its uneven fusion. The bony head of the femur is displaced upward, deformed, enlarged, and its contours become uneven. Bone spurs form on the surface of the inner and outer edges of the glenoid fossa |
| Third | Complete or partial fusion of the joint space is observed. The head of the femur is greatly expanded. Multiple bone growths are located on all surfaces of the acetabulum |
- The most important and constant pain is severe, constant pain in the groin, hip, knee joint, sometimes radiating pain to the leg and groin area
- Stiffness of movement, limited joint mobility
- Limiting the abduction of the affected leg to the side
- In severe cases, lameness, gait disturbance, shortening of the leg, atrophy of the thigh muscles
The following types of arthrosis are distinguished:
- dysplastic – the bevel of the acetabulum is determined;
- post-traumatic – depends on the nature of the injury and the shape of the joint after bone fusion.
At the initial stage of development, coxarthrosis can manifest itself only with mild pain. They usually occur after intense physical exertion or a hard day at work. The person attributes the deterioration in health to muscle “fatigue” and does not seek medical help. This explains the frequent diagnosis of coxarthrosis at stages 2 or 3, when conservative therapy is ineffective.
The range of motion in the hip joint is reduced due to compensatory growth of bone tissue, damage to the synovial membrane, and replacement of areas of the articular capsule with fibrous tissues devoid of any functional activity. Mobility may be somewhat limited even with grade 1 coxarthrosis. Difficulties arise when performing rotational movements with the leg.
When walking, flexing and (or) extending the hip joint, clicks, crunching, and crackling sounds are clearly heard. The reason for this sound accompaniment of each step is the friction of bone surfaces, including osteophytes, against each other. Crunching can also appear in normal health due to the collapse of carbon dioxide bubbles in the joint cavity. Coxarthrosis is indicated by its combination with dull or sharp pain.
We invite you to read: What is protrusion of the lumbar spine
Painful sensations become constant already at stage 2 of coxarthrosis. Their severity decreases somewhat after a long rest. The pain intensifies during the next relapse or the development of synovitis (inflammation of the synovial membrane) that often accompanies osteoarthritis. During the remission stage, the discomfort decreases somewhat. But as soon as a person becomes hypothermic or lifts a heavy object, severe pain appears again.
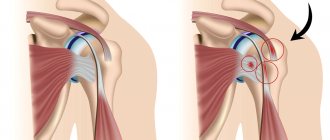
Muscle spasm
Increased tension in the skeletal muscles of the thigh occurs with coxarthrosis for several reasons. Firstly, the ligaments weaken. The muscles spasm to hold the head of the femur in the acetabulum. Secondly, increased tone often accompanies inflammation of the synovial membrane. Thirdly, when osteophytes are displaced, nerve endings are compressed, and muscle spasm becomes a compensatory reaction to acute pain.
Lameness
In the later stages of development of coxarthrosis, the patient begins to limp severely. Changes in gait are provoked by flexion contractures and deformation of bone surfaces, making it impossible to maintain a straight leg position. The person also limps to reduce the severity of pain by transferring body weight to the unaffected limb.
Leg shortening
Shortening of the leg by 1 cm or more is typical for coxarthrosis of grade 3. The reasons for the decrease in the length of the lower limb are severe muscle atrophy, thinning and flattening of cartilage, narrowing of the joint space, and deformation of the femoral head.
Causes and provoking factors
Idiopathic or primary arthrosis develops without any reason. It is believed that the destruction of cartilage tissue occurs due to the natural aging of the body, a slowdown in recovery processes, a decrease in the production of collagen and other compounds necessary for the complete regeneration of the structures of the hip joint. Secondary arthrosis occurs against the background of a pathological condition already present in the body. The most common causes of secondary disease include:
- previous injuries - damage to the ligamentous-tendon apparatus, muscle ruptures, their complete separation from the bone base, fractures, dislocations;
- impaired articulation development, congenital dysplastic disorders;
- autoimmune pathologies - rheumatoid, reactive, psoriatic arthritis, systemic lupus erythematosus;
- nonspecific inflammatory diseases, such as purulent arthritis;
- specific infections - gonorrhea, syphilis, brucellosis, ureaplasmosis, trichomoniasis, tuberculosis, osteomyelitis, encephalitis;
- dysfunction of the endocrine system;
- degenerative-dystrophic pathologies - osteochondropathy of the femoral head, osteochondritis dissecans;
- hypermobility of the joints, caused by the production of “superextensible” collagen, provoking their excessive mobility, weakness of the ligaments.
Since the development of arthrosis can be caused by hemarthrosis (bleeding into the cavity of the hip joint), provoking factors include hematopoietic disorders. Prerequisites for the occurrence of the disease are excess weight, excessive physical activity, and a sedentary lifestyle. Its development is caused by improper organization of sports training and a deficiency in the diet of foods high in microelements, fat- and water-soluble vitamins. Postoperative arthrosis occurs several years after surgery, especially if it was accompanied by excision of a large amount of tissue. The trophism of hyaline cartilage is disrupted by frequent hypothermia, living in an environmentally unfavorable environment, or working with toxic substances.
Osteoarthritis of the hip joint cannot be inherited. But in the presence of certain congenital characteristics (metabolic disorders, skeletal structure), the likelihood of its development increases significantly.
Tactics of drug treatment
Drug treatment is aimed at improving the patient’s well-being. For this purpose, drugs of various clinical and pharmacological groups are used:
- nonsteroidal anti-inflammatory drugs (NSAIDs) - Nimesulide, Ketoprofen, Diclofenac, Ibuprofen, Meloxicam, Indomethacin, Ketorolac. Injection solutions are used to relieve acute pain, and tablets, dragees, ointments, and gels help eliminate pain of mild or moderate severity;
- glucocorticosteroids - Triamcinolone, Diprospan, Dexamethasone, Hydrocortisone, Flosterone. They are used in the form of intra-articular blockades in combination with the anesthetics Novocaine, Lidocaine;
- muscle relaxants - Mydocalm, Baklosan, Sirdalud. Included in treatment regimens for spasms of skeletal muscles, pinching of sensitive nerve endings;
- drugs that improve blood circulation in the joint - Nicotinic acid, Eufillin, Pentoxifylline. Prescribed to patients to improve tissue trophism and prevent disease progression;
- chondroprotectors - Teraflex, Structum, Artra, Dona, Alflutop. Effective only at stages 1 and 2 of arthrosis.
Rubbing in ointments with a warming effect (Viprosal, Apizartron, Finalgon, Dikul balms) helps eliminate mild pain. The active ingredients of external agents are capsaicin, cinquefoil, camphor, menthol. These substances are characterized by a locally irritating, distracting, analgesic effect.
Compresses on the joints with Dimexide, bischofite, and medical bile will help you cope with puffiness and morning swelling of the thigh. Patients are recommended classic, acupressure or vacuum massage for coxarthrosis. An excellent prevention of further progression of arthrosis is daily physical therapy exercises.
Surgical intervention
If conservative treatment is ineffective, pain that cannot be eliminated with medication, or the steady progression of coxarthrosis, patients are advised to undergo surgical intervention. The operation is performed immediately in case of pathology of 3rd degree of severity, since it is impossible to eliminate the resulting destructive changes in cartilage and bones by taking medications or exercise therapy.
Stages of coxarthrosis.
Arthroplasty
The operation is performed using general anesthesia. The head of the femur is removed from the acetabulum. Visible destructive changes in tissue are corrected - bone growths are removed, articular surfaces are leveled, tissue that has undergone necrosis is excised. During surgery, cavities are formed and filled with ceramic implants.
Endoprosthetics
Hip replacement with an implant is performed under general anesthesia. To prevent the development of an infectious process, a course of antibiotics is prescribed. After 10 days, the sutures are removed and the patient is discharged from the medical facility. At the rehabilitation stage, patients are shown physiotherapeutic and massage procedures, exercise therapy.
Hip arthrosis in an advanced form requires only the only possible treatment – surgery. Depending on the severity and presence of developed symptoms, the degree and nature of joint destruction, various types of operations are used, namely:
- Diarthrosis-preserving, corrective osteotomy of the femur and pelvis;
- Endoprosthetics, which can be either partial or total, is a replacement of the hip joint;
- Arthrodesis, an operation involving closure of the hip joint.
If conservative therapy is ineffective or a pathology complicated by ankylosis is diagnosed, surgery is performed. It is impossible to restore cartilage tissue in a joint damaged by arthrosis without prosthetic surgery, but with the right approach to treatment, compliance with all medical prescriptions, maintaining a correct lifestyle, doing therapeutic exercises, regular massage courses, taking vitamins and proper nutrition, you can stop the process of damage and destruction of cartilage and hip joints.
Causes of the disease
The main factors that influence the development of the disease are:
- injuries and microtraumas of the hip joint;
- excess weight;
- load on joints due to the nature of the profession;
- infarction (necrosis) of the hip joint, which occurs as a result of taking various medications, suffering from stress, drinking alcohol in large quantities;
- congenital defect of joints in the pelvic area;
- arthritis (inflammatory processes in the joints);
- changes in hormonal levels (mainly age-related);
- osteoporosis (death of bone tissue).
Non-traditional folk treatment of arthrosis
Many people who are wondering how to treat chronic arthrosis of the hip joint will try traditional medicine on themselves. Opinions about this method of therapy are very diverse and far from unanimous; for some it helps, but for others it only brings disappointment. But the fact is that there are too many “grandmother’s recipes”, so finding an individually suitable one will require a lot of time and effort. The most common folk remedies include:
- Compresses (honey, oil, clay, mud, cabbage, gelatin);
- Rubs (based on herbal infusions, vegetable oils and animal fats);
- Herbal infusions and teas (used for oral administration);
- Ointments (based on honey, mustard, plant and vegetable juice);
- Baths (pine, salt, herbal).
Complications
The lack of adequate treatment for deforming arthrosis of the hip joint is fraught with consequences such as:
- venous stagnation of blood, leading to the formation of blood clots;
- scoliosis – curvature of the spine;
- disturbances in the functioning of the urinary system.
Clinical and morphological changes that occur in the second and third stages of the disease lead to the loss of the ability to fulfill basic physiological needs. A person develops a need for partial or permanent outside care. In this case, you will have to officially prove your disability. Which may require a lot of effort and time.