Chronic periodontitis is considered to be not an independent disease, but a complication that occurs as a result of the long-term development of other pathologies in the oral cavity. The disease is an inflammatory process that affects the periodontal area (tissue located between the alveoli and the root) and is accompanied by a change in the structure of its tissues. The main reason for the development of chronic periodontitis is infection. But there are other unfavorable factors that can provoke the development of a dangerous pathology.
Signs of the chronic form are very diverse. These are tooth pain, swelling and hyperemia of the gums, disruption of their structure, leading to tooth mobility, bad breath, and many other manifestations. The disease needs proper and timely elimination. The choice of treatment method is made based on the causes and symptoms present in the patient. In modern dentistry, both conservative and radical methods of therapy are used, and to achieve more effective results, folk recipes are also used.
Types of periodontitis
In dental practice, the classification of periodontitis according to I.G. is used. Lukomsky:
- Acute periodontitis (serous, purulent).
- Chronic periodontitis (fibrous, granulating, granulomatous).
- Chronic periodontitis in the acute stage.
Based on the location of the process, they are distinguished:
- apical periodontitis (the source of inflammation is at the apex of the tooth),
- marginal periodontitis (pathological changes affect the circular ligament of the tooth and are located at the edge of the gum).
Exacerbation of periodontitis
Treatment of periodontitis
As with any other chronic disease, periodontitis can worsen. Exacerbation begins due to factors such as:
- decreased immunity;
- hypothermia;
- allergy;
- cold.
In addition to simple factors, there are special specifics:
- The periodontal membrane is damaged. A focus of purulent inflammation is formed. Strong pressure and excess load on the tooth - for example, chewing hard food - lead to rupture of the purulent sac.
- Pus does not come out of the lesion due to various obstacles. If pus can flow through the root canals of the teeth, then the disease occurs without symptoms. But if the outflow of pus is hampered, then it accumulates, which is accompanied by severe pain.
Causes of periodontitis
Based on the cause that caused the development of periodontitis, the inflammatory process can be infectious, traumatic and drug-induced.
Infectious periodontitis develops due to the entry of microorganisms, their toxins, and decay products of pulp and dentin into the periodontium through the inflamed internal canals of the tooth or periodontal pocket (from the gum side). Less commonly, the infection spreads from surrounding tissues (with osteomyelitis, sinusitis) or through the blood in severe general diseases (sepsis, tuberculosis, typhoid).
Traumatic periodontitis occurs as a result of bruises, falls with damage to teeth, and biting on hard objects. The cause of injury can also be medical manipulations - pushing instruments beyond the apical opening of the tooth, the presence of over-inflated fillings and crowns. Acute injuries are often reversible, when after irritation of the periodontium there is a gradual recovery.
Drug-induced periodontitis is a consequence of the penetration of potent medicinal substances beyond the apex of the tooth: arsenic paste, phenol (if the terms of follow-up treatment of the tooth are not followed), solutions for canal treatment, filling materials.
Forms of the disease
Depending on the cause that caused the development of the infectious-inflammatory process, there are three forms of apical periodontitis:
- infectious;
- traumatic;
- medicinal.
In accordance with the routes of infection, the following forms of the disease are distinguished:
- intradental (infection penetrates through the apical canal of the problematic tooth);
- retrograde (infection enters from the gingival margin);
- extradental (infection enters the periodontium from another site of inflammation).
According to the activity of the inflammatory process, apical periodontitis can be acute or chronic. Acute forms of the disease, in turn, are divided into serous and purulent. Chronic apical periodontitis occurs:
- fibrous;
- granulomatous;
- granulating.
A complication of chronic forms of apical periodontitis is the formation of granulomas and cysts, requiring surgical intervention and sometimes removal of the diseased tooth.
Symptoms and classification of periodontitis
The clinical manifestations of different types of periodontitis are somewhat different from each other. In the acute phases, the severity of symptoms predominates; in chronic inflammation, complaints may be completely absent, and the diagnosis is established only on the basis of objective examinations.
Acute apical periodontitis
Acute periodontal inflammation is characterized by the appearance of sharp pain in the tooth. Initially, the pain is localized, and the patient can point to the causative tooth. Gradually, due to an increase in edema, the pain syndrome intensifies, the pain becomes intense and pulsating, and can radiate along the nerve fibers.
There are usually two phases in the progression of symptoms:
- The first phase often develops after untreated pulpitis, as a complication. Constant aching pain appears. There may be discomfort when biting. Percussion (tapping) of the tooth is slightly painful.
- In the second phase, the pain becomes continuous, its intensity remains or increases. Patients complain of a feeling of an “overgrown tooth” (associated with the accumulation of inflammatory exudate in the apex area). There is sharp pain when biting, sometimes even when touching the tooth. The gums near the causative tooth are hyperemic (with redness) and swollen, painful to the touch. If exudate (pus) breaks through the gum from the inflammatory focus, a fistula forms, pain and swelling decrease. Changes in the general condition (fever, signs of inflammation in the blood) are rarely observed with periodontitis. The only characteristic feature is enlargement and tenderness of the submandibular lymph nodes.
Chronic fibrous periodontitis
Fibrous inflammation develops as a result of untreated acute periodontitis or chronic pulpitis, or after more severe forms of periodontal inflammation. There are no objective symptoms or complaints in this clinical form. Diagnosis of periodontitis is carried out on the basis of anamnesis (history of the disease and previous complaints) and X-ray data.
Chronic granulating periodontitis
Granulating periodontitis may not cause any special complaints or be asymptomatic. Some patients experience slight pain when biting and a feeling of fullness in the root area. When palpating the gums, you can feel a slight thickening in the projection of the apex of the tooth, which is sensitive when pressed.
Tapping a tooth produces a slight pain response compared to neighboring teeth. When interviewed, patients may mention the appearance of tooth pain after colds, or the periodic formation of a fistula.
Chronic granulomatous periodontitis
Granulomatous periodontitis is more stable and less active than granulomatous periodontitis. This form is distinguished by the presence of a fibrous capsule, which delimits the source of inflammation from the surrounding tissue. Symptoms outside of exacerbation of the process are usually not expressed. The presence of inflammation is indicated by survey data (pain in the tooth or fistulous tract) and radiological signs.
Exacerbation of periodontitis
When periodontitis worsens, the sluggish course of inflammation suddenly becomes more active. A painful sensation appears, the gums swell, and the facial tissues swell. Dentists identify several factors that influence the exacerbation of periodontitis:
- The shell of the purulent focus is damaged. During inflammation, pus accumulates in a kind of sac, which is limited by the membrane. With increased pressure on the tooth, the membrane ruptures, and the pus comes out along with all the bacteria. Inflammation begins.
- Problems with the outflow of pus. If a fistula is formed, then the pus comes out through it. This process does not cause discomfort in the patient. But if the root canals become clogged, then a purulent accumulation occurs, which causes pain.
Marginal periodontitis
With inflammation of the marginal periodontium, the first symptoms are pain and swelling of the gingival papilla directly near the affected part of the tooth. Patients complain of constant aching pain in the tooth and a reaction when biting. Upon examination, you can detect serous or purulent discharge from the site of inflammation (gingival pocket), pain when tapping horizontally on the tooth (from the lip towards the tongue).
Initially, the dental pulp may not be involved in the process. Infection occurs retrogradely through the apex of the tooth as the disease progresses.
Diagnosis of periodontitis
The diagnosis of periodontitis is made on the basis of complaints, clinical examination data and x-ray pictures.
Characteristic differences of periodontitis:
- change in the color of the tooth crown due to long-term inflammation;
- deep carious defect with an open tooth cavity, painless when examined with dental instruments (probing);
- presence of fistula tracts;
- the presence of radiological signs corresponding to one of the forms of chronic periodontitis: expansion of the periodontal fissure (the distance between the root of the tooth and the alveolar bone), destruction of the bone at the apex of the tooth (irregular or rounded).
Types of chronic periodontitis
Studies of the clinical picture of the possible course of chronic periodontitis and morphological signs made it possible to identify the following types:
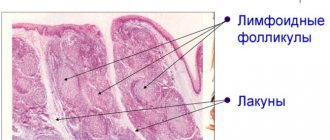
- Granulating
With this form of the disease, under a microscope, a noticeable thickening can be observed in the apical part of the tooth root. There is a change in the surface of the periodontium, it becomes uneven. Over time, granulation tissue grows, which causes resorption of bone tissue in the area of inflammation. This process is often accompanied by the appearance of purulent foci, which provokes the appearance of fistulas. In some cases, soft tissue adjacent to the site of inflammation undergoes granulation. This causes the formation of granulomas of various types (submucosal, subperiosteal, subcutaneous), after opening which, fistulas appear on the face and oral cavity, and unaesthetic scars appear at the site of their healing.
Patients experiencing granulating inflammation report pain when chewing solid food, aggravated by pressure, as well as periodic exacerbations of painful conditions.
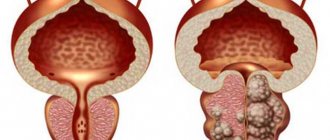
- Granulomatous
One of the forms of periapical inflammation, characterized by the formation of granulation tissue in the area of the root apex. The maturation of this tissue along the periphery provokes the appearance of a fibrous capsule that degenerates into a granuloma. Depending on the structural features, simple, epithelial and cystic granulomas are distinguished. Quite often, this form of the disease occurs as a consequence of granulating inflammation.
The course of the disease can occur according to various scenarios. Sometimes the granuloma grows slowly or does not grow at all. In this case, it usually does not cause any discomfort and is discovered by chance during an X-ray examination.
In other patients, the granuloma may enlarge, most often coinciding with exacerbations of chronic periodontitis, provoking changes in the granuloma tissue.
- Fibrous
It is characterized by the formation of a limited focus of inflammation caused by the spread of fibrous tissue. Most often this occurs after treatment of the forms of periodontitis described above, but sometimes the fibrous form occurs independently.
Often, fibrous inflammation is accompanied by excessive formation of cement, and in some cases, sclerosis of adjacent bone tissue.
An X-ray examination allows you to determine the form of chronic periodontitis. It is very important to correctly differentiate different types of disease, since the effectiveness of treatment directly depends on this.
Treatment of periodontitis
Conservative treatment of periodontitis is carried out by endodontic (intra-root) canal treatment using special instruments and antiseptics. The goal of therapy is to clean the canals from infected remains of dentin and pulp and, as a result, relieve inflammation in the periodontium and restore its structures.
The treatment regimen includes several visits to the doctor. On the first visit, under anesthesia, the canal is treated and washed with antiseptic solutions (2% chlorhexidine, 1% sodium hypochlorite). Anti-inflammatory paste is placed into the cleaned and dried canals, and the tooth is closed with a temporary filling. The next visit is scheduled in 2-3 weeks.
The tactics for treating periodontitis at the second visit depends on the condition of the tooth.
Canal filling is possible in the following cases:
- absence of complaints from the patient (the tooth does not react to biting, does not hurt);
- absence of discharge from the canal during tooth treatment;
- no changes on the radiograph (periodontitis - acute or fibrous);
- the presence of a fistulous tract. In all other situations, the channels are washed again and an anti-inflammatory agent is applied for a period of 2-4 weeks.
Chronic forms of periodontitis require longer treatment. Filling of the canals is carried out only after complete elimination of inflammation in the canals and the presence of positive dynamics on the radiograph (reduction of the inflammatory focus and rarefaction of bone tissue).
Treatment of periodontitis with antibiotics is not expected in the standard treatment regimen. Drugs can be prescribed individually in the following cases:
- periodontitis is accompanied by complications - periostitis, abscess, severe edema, severe general condition;
- periodontal inflammation cannot be cured therapeutically (for example, with obstructed canals), and antibiotics are used as a temporary measure to combat the infection;
- local treatment does not produce results - suppuration continues from the canals, the tooth does not withstand sealing (closure with a temporary filling).
Amoxiclav, Roxithromycin, and Clindamycin are used to treat inflammatory diseases in the oral cavity.
Treatment of periodontitis at home
At home, soda rinses (a teaspoon of soda in a glass of warm water) are recommended for the treatment of periodontitis. Rinses should be in the form of “baths” for the tooth. With their help, internal swelling and tension in the tissues are reduced. Rinsing promotes the formation of a fistula tract and the outflow of exudate.
It should be borne in mind that it is impossible to cure periodontitis on your own. Home treatment is intended to provide some relief from symptoms, but does not eliminate the infection inside the teeth.
Surgical methods for treating periodontitis
Surgical methods for treating periodontitis include operations:
- Preserving the tooth and the integrity of the periodontium - cystectomy (husking the cyst), resection of the root apex (extraction of the cyst along with the damaged part of the tooth root).
- Partially preserving the integrity of the tooth (in multi-rooted teeth) - root amputation, hemisection of the tooth (removal of one root along with part of the crown).
- Removal of a tooth.
Indications for surgical treatment:
- lack of effect from conservative therapy;
- tooth mobility of 2-3 degrees due to significant bone destruction;
- periodontitis complicated by periostitis or osteomyelitis;
- the presence of complications resulting from the treatment of the canal - fracture or perforation of the root, breakage of an instrument in the canal.
Causes and risk factors
The chronic form of the disease develops as a result of exposure to the following unfavorable factors:
- Reproduction of pathogenic bacteria in the oral cavity in diseases such as caries, periodontal disease, pulpitis or acute periodontitis. In the absence of timely correction, pathogenic microflora penetrates through the affected areas (carious canals or gum pockets) into the periodontal area, provoking the development of inflammation.
- Traumatic damage to tooth enamel and deeper tooth tissues (superficial or pulpal dentin).
- Long-term impairment of the functionality of the immune system due to frequent colds, viral diseases, or pathologies of an autoimmune nature.
- Incorrect treatment of pulpitis, when arsenic-based drugs were used for a long time to devitalize (kill) the pulp.
- Violation of the technique of cleaning and filling a carious canal, when strong antiseptic drugs were introduced into its cavity, or the cauterization method was used.
- Failure to comply with the rules of oral hygiene and dietary errors are the reasons that provoke the development of caries, which can later be complicated by periodontitis.
Treatment of periodontitis during pregnancy
A feature of periodontitis therapy during pregnancy is limited diagnostic capabilities and control over the quality of treatment. According to sanitary and epidemiological standards, the use of X-ray examinations is prohibited in the first trimester; in the future, images using a computer visiograph are permitted.
In this regard, the final filling of the canals and installation of a filling is carried out in later stages of pregnancy, or the tooth is closed with temporary materials with follow-up treatment after the birth of the child.
Treatment
Treatment of both acute and chronic apical periodontitis consists of several stages:
- Mechanical preparation. Under local anesthesia, the doctor opens the cavity of the diseased tooth and thoroughly cleans it of necrotic masses, processes and expands the lumen of the root canals, which allows creating the necessary conditions for the outflow of exudate from the periodontium. At home, the patient should regularly rinse the mouth with antiseptic solutions. For this purpose, infusions of medicinal plants (eucalyptus leaves, chamomile flowers) are often used.
- Antiseptic treatment. Antiseptic preparations in the form of pastes are placed into the cavity of the affected tooth. To stop the inflammatory process, antibacterial and anti-inflammatory drugs can be prescribed.
- Canal filling. After complete relief of inflammation, the canals of the diseased tooth are filled with mandatory x-ray control. The tooth cavity is then closed with a permanent filling.
Treatment process for apical periodontitis
Timely initiation of therapy for apical periodontitis allows for complete cure while preserving the tooth in 90% of cases.
Possible complications of periodontitis
In acute and exacerbation of chronic periodontitis, complications are associated with the spread of infection to surrounding tissues.
The consequences of this are possible in the form of:
- fistula tracts (including those opening on the skin of the face);
- periostitis (inflammation of the periosteum);
- osteomyelitis (inflammation of the jaw bones).
As a result of chronic periodontitis, there is a high risk of developing a tooth root cyst.
The main danger of long-term periodontitis is that it is a chronic source of infection. The constant accumulation of pathogenic bacteria in it leads to increased sensitivity of the body to infections, allergization of the body, and frequent exacerbations of chronic diseases.
How does the pathology manifest itself?
The causes of inflammation of the peri-root structures of the tooth are trauma, caries or pulpitis. Also, the catalyst for the appearance of apical periodontitis is drugs used in the treatment of pulp inflammation, which irritate periodontal tissue. As a result, the disease becomes infectious. The disease is also provoked by bacteria: staphylococci, streptococci, actinomycetes, lactobacilli. The disease occurs in acute and chronic forms. Symptoms:
- increased tooth sensitivity to cold and hot;
- pulsating pain radiating into surrounding tissues;
- enlargement of local lymph nodes;
- increase in body temperature up to 38 degrees;
- headache;
- general deterioration of condition.
The acute form lasts 2-14 days and, in the absence of adequate treatment, becomes chronic.
Fistulas form, purulent discharge particles appear, bad breath, moderate pain, and a feeling of fullness from the inside. Important! Apical periodontitis is dangerous due to complications in the form of perimandibular abscess, osteomyelitis, purulent melting of tissue (phlegmon).
Differences between periodontitis and pulpitis
Differential diagnosis of diseases is carried out according to the following criteria:
- Pain – with pulpitis is spontaneous, often nocturnal, long-lasting, paroxysmal, a pronounced reaction to hot food. Periodontitis is characterized by pain when biting, aching and diffuse pain - in later stages, the tooth reacts to cold.
- Probing a carious cavity is sharply painful in case of pulpitis; in case of periodontitis, there may be no reaction.
- Palpation of the gums in the area of the tooth root with pulpitis is always painless.
- X-ray signs – with pulpitis, a deep carious cavity is observed, there are no changes in bone tissue and periodontium.
What should not be done if periodontitis develops?
If you experience tooth pain and suspect periodontitis, you should not:
- warm the tooth from the outside (including applying your hand, a heating pad, all kinds of compresses, tying a scarf around the tooth) - all this can lead to an increase in the amount of exudate and its breakthrough into the soft tissues;
- sleeping on the sore side also leads to heating of the area of inflammation;
- apply tablets to the gum or tooth cavity;
- try to squeeze out, puncture the fistula or lubricate it with alcohol solutions (iodine, brilliant green).
What to do if a tooth hurts after periodontitis therapy?
If a tooth becomes sick during treatment (after placing a temporary filling), it should be “opened” again to create an outflow through the canal. If it is impossible to contact a dentist, the temporary filling is removed independently. In the future, you need to visit a doctor as soon as possible to re-rinse the tooth and install the medicine.
After treatment, sensitivity in the tooth and pain when biting may persist for some time (usually within a week). In case of severe pain, it is recommended to continue rinsing with soda, and take Suprastin (1 tablet in the morning and evening) as a means to reduce swelling.
If there is no positive dynamics, you should consult a dentist. The doctor will take another picture and, if necessary, prescribe anti-inflammatory or antibacterial drugs. If there is severe pain in the tooth, it may be necessary to unfill and re-treat the canal.
Diagnostics
If characteristic symptoms appear, you should contact your dentist as soon as possible. The specialist will necessarily examine the patient, conduct a survey regarding complaints and refer him for an x-ray examination. X-rays are the gold standard for diagnosing apical periodontitis. Depending on the changes in the image, the doctor can judge the development of one or another form of pathology.
Differential diagnosis of apical periodontitis is carried out with purulent diffuse pulpitis, as well as maxillary sinusitis and osteomyelitis, in which a similar clinical picture is observed. To clarify the diagnosis, electroodontometry (EDO) is performed, which is designed to determine the degree of pulp damage.
Errors and complications in the treatment of periodontitis
Errors in the treatment of periodontitis are associated with damage to the internal tissues of the tooth (perforation of the bottom of the tooth or root canal) or breakage of instruments in the canals.
Possible complications:
- pain of varying intensity associated with residual inflammation, penetration of materials beyond the apex of the tooth, traumatic neuritis of the facial nerve;
- preservation of the focus of infection or its increase;
- change in the color of the tooth crown;
- crown chipping.
Possible complications and consequences
If treatment is not started in a timely manner or is carried out incorrectly, it is not possible to achieve a lasting positive result with conservative treatment methods. In this case, the apex of the root of the diseased tooth is resected. If this intervention is unsuccessful, the tooth is removed.
The acute form of apical periodontitis can be complicated by the development of:
- periostitis;
- abscess;
- phlegmon;
- osteomyelitis;
- odontogenic sepsis.
A complication of chronic forms of apical periodontitis is the formation of granulomas and cysts, requiring surgical intervention and sometimes removal of the diseased tooth.