Chronic oophoritis
Chronic oophoritis
is a long-term inflammatory process that affects the ovaries. An exacerbation of the disease is characterized by dull or aching pain in the lower abdomen and groin area, mucous and mucopurulent leucorrhoea. In the remission phase, disorders of the ovarian-menstrual cycle, dyshormonal disorders, and infertility are observed. To diagnose the disease, bimanual examination, ultrasound of the pelvic organs, laparoscopy, and laboratory diagnostic methods are used. The treatment regimen includes etiotropic antibacterial drugs, anti-inflammatory, immunocorrective and enzyme agents.
General information
The chronic form of oophoritis as an independent pathology is extremely rare. Typically, inflammation of the ovaries is combined with damage to the fallopian tubes and is called chronic salpingoophoritis (adnexitis). In the vast majority of cases, oophoritis is secondary and develops as a result of the spread of the infectious process from other organs. Both ovaries or one of them can be involved in inflammation. The disease most often occurs in women aged 18-28 years who are sexually active. The importance of timely detection and treatment of oophoritis is due to the high incidence of secondary infertility. According to various studies in the field of gynecology, reproductive dysfunction is observed in 60-70% of cases of the disease.
Causes of chronic oophoritis
An inflammatory reaction in ovarian tissues usually occurs in response to exposure to infectious agents. The direct causative agents of the process can be:
- Sexually transmitted infections
. The most common causes of chronic oophoritis are gonococci, chlamydia, trichomonas, and mycoplasmas. In this case, the disease is usually bilateral. - Opportunistic pathogenic microorganisms
. Inflammation can be caused by streptococci, staphylococci, E. coli, anaerobes, etc. In the case of activation of nonspecific flora, the process can be bilateral or unilateral. - Mycobacterium tuberculosis
. One- or two-sided specific oophoritis in the form of tuberculous tubercles or caseomas is observed in 1/3 of phthisiatric patients.
Due to the peculiarities of their anatomical location and the presence of a dense outer capsule, the ovaries are well protected from microorganisms. For the occurrence of a chronic inflammatory process in them, a combination of several predisposing factors is required, the main of which are:
- Women's inflammatory diseases
. Most often, inflammation is detected in women with vaginitis, cervicitis, endometritis and salpingitis. - Inflammatory processes in the pelvis
. Acute appendicitis and other pathological conditions involving the peritoneum can lead to the development of chronic oophoritis. - Invasive interventions
. The spread of pathogens is facilitated by abortions, complicated childbirth, curettage and other therapeutic and diagnostic procedures. - Promiscuous sex life
. Frequent changes of partners and unprotected sex increase the likelihood of contracting STIs that are tropic to ovarian tissue. - Concomitant pathology and decreased immunity
. The risk of developing symptoms of the disease is increased in patients who suffer from obesity, diabetes, chronic diseases, experience stress, or take immunosuppressive medications.
It is extremely rare that inflammation develops as a result of organ trauma during accidents and abdominal surgeries. In some cases, a secondary inflammatory process occurs with benign and malignant ovarian tumors.
Causes
There are many causes of inflammation of the left ovary (left-sided oophoritis), but they are all associated with infection by pathogenic microorganisms. The most common routes of infection are the following:
- Sexually transmitted infections. Unprotected sexual intercourse can transmit both sexually transmitted diseases (syphilis, gonorrhea, donovanosis, etc.) and conditionally venereal diseases (chlamydia, ureplasmosis, mycoplasmosis, trichomoniasis, genital herpes, human papillomavirus, cytomegalovirus, etc.). In addition to the specific symptoms inherent in these diseases, the ovaries and/or appendages are almost always inflamed.
- Household infection, which can cause oophoritis, is less common than sexual infection. It can occur in shared spaces - saunas, steam baths, swimming pools, public showers, and also when using someone else's towel. In this case, various viruses, bacteria and fungi can be transmitted, which do not cause sexually transmitted diseases, but accompany the occurrence of the inflammatory process.
- Surgical interventions, including abortions, in which there is a risk of infection. Therefore, in order to avoid this kind of complications, a course of antibiotics is mandatory.
- Diseases of related organs and systems. Most often, inflammation of the ovaries in this case occurs when an infection is transmitted from the urinary tract (cystitis, urethritis), less often - during intestinal infections.
- Hormonal imbalances can lead to the appearance of single cysts on the ovary or polycystic disease. These processes can trigger inflammation.
- A decrease in immunity leads to the fact that opportunistic microflora living in the body begins to actively multiply. The immune cells that held it back can no longer cope with their task, so an inflammatory process develops. A decrease in the body's immune forces in almost all cases causes an exacerbation of chronic left-sided oophoritis, if there is a history of one.
- Mechanical damage to the mucous membranes of the uterine vagina, which can occur, for example, when installing or removing the uterine device.
- Hypothermia contributes to a decrease in immunity, so the chronic inflammatory process worsens, or an acute one occurs.
- Prolonged stress is also a catalyst for decreased immunity.
- Infection can also occur during childbirth, since the genital tract is very vulnerable during this period, and the woman’s immunity is reduced.
- Neglect of personal hygiene rules.
- Miscarriage can also lead to oophoritis, since surgery is required and there is a high risk of pathogens.
Doctors cannot accurately determine why left-sided oophoritis occurs. Statistics show that right-sided inflammation of the ovary occurs more often, since it is in this place that large blood vessels and arteries pass, and the appendix is located nearby. But in most cases, the occurrence of unilateral inflammation is determined randomly, so it is impossible to predict which side of the ovary will become inflamed when an infection occurs.
Pathogenesis
Chronic inflammation can develop gradually (for example, with gonorrhea or asymptomatic chlamydia) or be the result of untreated acute oophoritis. There are four main ways pathogens enter the ovarian tissue: ascending (from the vagina, cervical canal, uterus, fallopian tubes), descending (through the peritoneum), lymphogenic (from nearby organs) and hematogenous (with tuberculosis). Often, inflammation spreads from the outer membranes of the organ to the cortex and medulla. In case of lymphogenous and hematogenous infection, the stroma and follicular tissue are the first to be involved in the process. Usually the inflammation is serous or serous-fibrinous, much less often purulent.
The chronic course of the disease is facilitated by increasing endogenous intoxication, decreased immune reactivity, local microcirculation disorders and changes in blood rheology. As the cortex is involved in the process, endocrine function is disrupted, which is manifested by signs of hypo- or hyperestrogenemia. Chronication of oophoritis is accompanied by the activation of autoimmune mechanisms, as a result of which antibodies to ovarian tissues are produced. The combination of these disorders with the effect of specific infections, especially chlamydia, depletes the ovarian reserve, which increases the risk of infertility and worsens the prospects for in vitro fertilization.
The disease occurs cyclically: a period of exacerbation with clinical symptoms, expressed to varying degrees, is replaced by remission. Exacerbation of the process is usually facilitated by hypothermia, stress, hormonal changes during pregnancy or before menstruation, colds, and decreased immunity.
Symptoms of chronic oophoritis
The clinical picture of the disease depends on its phase. During an exacerbation, the patient is bothered by a dull or aching pain in the lower abdomen and groin area. Possible irradiation to the sacrum, increased pain during physical exertion and sexual intercourse. If other genital organs are involved in the inflammation, the amount of vaginal discharge increases, usually mucous, less often mucopurulent. General symptoms, as a rule, are mild; in rare cases, they manifest as fever up to low-grade levels, nausea, and sometimes vomiting.
In remission there is usually no pain. A woman’s sleep may deteriorate, performance may decrease, fatigue and irritability may occur, the menstrual cycle, sexual and reproductive functions may be disrupted. With chronic oophoritis, periods become irregular, while the menstrual cycle usually lengthens, intermenstrual bleeding, pain and heavy menstrual flow may occur. Some patients experience severe PMS. In 50-70% of women, libido decreases, which is often associated with dyspareunia (painful sensations during sex). In some cases, the only sign of chronic inflammation is the inability to become pregnant with regular sexual activity.
Complications
Since in the chronic course oophoritis is usually combined with salpingitis, the most serious complication of the disease is adhesive disease. It is plastic pelvioperitonitis and disruption of the endocrine function of the ovaries that usually lead to tubal-peritoneal infertility. In addition, such patients have a significantly increased risk of ectopic pregnancy and miscarriage. With exacerbation, oophoritis can be complicated by purulent-inflammatory processes, from purulent melting of the ovaries (pyoovar) to the formation of a tubo-ovarian abscess and the development of peritonitis.
Diagnostics
When making a diagnosis, it is necessary to take into account that the symptoms characteristic of chronic oophoritis are quite nonspecific and may indicate other gynecological diseases. Therefore, the examination plan includes methods that reliably confirm the localization of inflammation and allow identifying the pathogen:
- Inspection on the chair
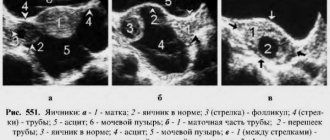
. On bimanual examination, the appendages are pasty, compacted or stringy. On palpation, pain and limited mobility are noted. - Transvaginal ultrasound
. The ovaries are enlarged, their surface is smoothed. The echogenic structure is enhanced due to the presence of areas of fibrosis. Echo signs of inflammation of the fallopian tubes and endometrium may be present. - Laparoscopy
. The endoscopic method is considered the gold standard for diagnosing inflammation in the ovaries. During the procedure, you can not only confirm the inflammatory process, but also, if necessary, take biomaterial for histological examination. - Laboratory diagnostics
. Microscopy, culture of vaginal discharge, PCR, RIF, ELISA and other tests can determine the causative agent of oophoritis. - Tuberculin test. Indicated in the presence of an extensive inflammatory process in the pelvic area with scant clinical symptoms.
Differential diagnosis is carried out with other inflammatory gynecological diseases and volumetric processes in the pelvic cavity. According to indications, the patient is referred for consultation to a gynecologist-reproductologist, oncogynecologist, or phthisiatrician.
Treatment of chronic oophoritis
The choice of therapeutic regimen depends on the phase of the process. In case of exacerbation and the identified causative agent of inflammation, the following are indicated:
- Etiotropic antibacterial therapy
. Medicines are selected taking into account the sensitivity of pathogenic flora. If necessary, broad-spectrum antibiotics are prescribed until culture results are obtained. - Anti-inflammatory drugs
. Non-steroidal drugs can reduce pain and the severity of inflammatory changes. - Enzyme therapy
. The use of enzyme preparations is aimed at preventing adhesive disease and resolving existing adhesions. - Immunocorrection
. To strengthen the body's own defenses, immunostimulants, interferonogens, and vitamin and mineral complexes are recommended.
During the period of remission, therapy aimed at strengthening the immune system and restoring reproductive and endocrine functions plays a leading role. At this stage, immunoregulators, enzymes, eubiotics, biogenic stimulants, and hormonal drugs are prescribed. A combination of drug treatment with physiotherapy and balneotherapy is effective. Surgical techniques are used in the presence of complications. Operations are indicated when severe purulent-inflammatory diseases (pyoovar, tubo-ovarian abscess, peritonitis, etc.) and adhesive disease leading to tubo-peritoneal infertility are detected.
Treatment
When the diagnosis is accurately established, the stage of the disease is known, then treatment is determined. The acute form, as we have already noted, is treated in the hospital. The patient must remain in bed; cold compresses are applied to her lower abdomen. Desensitizing and painkillers, antibacterial and restorative drugs are prescribed.
Treatment of the chronic form of the disease is complex. An individual course of treatment is drawn up, which includes physical therapy and medication. Physical therapy may include:
- hirudotherapy
- electrophoresis
- gynecological massage
- magnetic therapy
- laser therapy
Often they resort to folk methods of treatment and herbal medicine, which are also used in the prevention of oophoritis. The therapy is long-term, but it must be completed. If the cause of the disease is a sexually transmitted infection, then the partner is also treated to avoid prostatitis and re-infection of the partner. During the treatment period, both are prescribed sexual rest.
Antibiotics for oophoritis are prescribed for relapses of chronic inflammation and intensification of pathological processes in the ovaries. At the same time, they resort to methods of restorative treatment. The choice of antibiotics depends on the body's sensitivity to the drug. To do this, bacteriological culture is carried out and the type of pathogen is determined.
The most commonly used antibiotics to treat oophoritis are:
- Sumamed
- Azithromycin
- Hexamethylenetetramine
- Amoxiclav
- Gentamicin
- Urotropin
- Unidox Solutab
- Doxycycline
- Klindafer
- Doxibene
- Metronidazole
- Dalatsin
- Trichopolum
- Ceftriaxone, etc.
The following medications are used to relieve abdominal pain:
- Aspirin
- Nospaz
- Asalgin
- Spasmalgon
- Tempalgin
Vaginal suppositories are also used for treatment:
- hexicon
- betadine
- suppositories with indomethacin
Prognosis and prevention
With an uncomplicated course and proper treatment, the prognosis is favorable. To prevent chronic oophoritis, it is recommended to visit a gynecologist every 6 months, carry out invasive procedures reasonably, refuse abortions, and promptly and sufficiently treat infectious and inflammatory diseases of the reproductive sphere. It is important to exclude casual sex, use barrier contraceptives, maintain personal hygiene, lead a healthy lifestyle with sufficient physical activity, and quit smoking and alcohol abuse. It is necessary to avoid hypothermia, significant psycho-emotional and physical stress.
source
Prevention of pathology
To avoid the development of an inflammatory process in the left ovary, you should adhere to several recommendations:
- Use condoms during sexual intercourse.
- Don't get too cold.
- Don't be nervous and avoid stressful situations.
- Support the immune system.
- Respond to alarming symptoms in a timely manner.
- Visit the gynecological office several times a year.
- Maintain personal hygiene and be careful in public toilets.
Do not forget that ovarian inflammation is an insidious and dangerous disease. But if it is detected in time and adequate therapy is started, then you should not be afraid of any complications or harm to health.
What is chronic oophoritis?
The ovary (ovarium) is a paired hormonally active organ of the female reproductive system. Located in the pelvic area, on both sides of the uterus. Contacts the uterus through the fallopian tubes (salpinx).
The ovaries together with the fallopian tubes are often called the uterine appendages.
Follicles with eggs develop in the ovaries, and the bulk of female sex hormones (estrogens, progesterone) are produced.
Ovaries, fallopian tubes and uterus - location
Oophoritis is an inflammatory disease of the female genital area associated with infectious or immune damage to ovarian tissue.
Isolated oophoritis is extremely rare (6-10%). Usually the fallopian tubes are involved in the inflammatory process. In this case, the disease is called salpingoophoritis or adnexitis.
The course of oophoritis is more often of a primary chronic nature - the disease develops gradually, without obvious clinical manifestations, seriously complicating diagnosis and timely treatment. Chronic inflammation is periodically complicated by exacerbations.
In rare cases, the disease begins clinically acutely, and then, with inadequate treatment or the influence of other factors, takes a subacute or chronic form.
Oophoritis (inflammation of the ovaries): types of course
ICD-10 code
N70.1 Chronic oophoritis/salpingitis N70.9 Oophoritis/salpingitis, unspecified
Chronic unilateral oophoritis - what is it?
If the inflammatory process affects only one ovary (the other remains healthy), then the painful condition is one-sided.
Long-term inflammation of the left ovary is called chronic left-sided oophoritis, and the right ovary is called chronic right-sided oophoritis.
Localization of inflammation during oophoritis
Chronic bilateral oophoritis - what is it?
Without treatment, chronic oophoritis in women often becomes a source of ectopic pregnancy, infertility, and acute surgical pathology
Consequences of chronic oophoritis
- Decreased ovarian function, anovulation, menstrual irregularities
- Dishormonal diseases of the genital organs
- Spontaneous miscarriage
- Ectopic pregnancy
- Adhesive process
- Infertility
- Persistent pain syndrome
- Involvement of neighboring organs in the chronic inflammatory process: bladder, intestines, etc.
Dangerous complications of the disease
- Purulent tubo-ovarian "tumor"
- Ovarian abscess
- Piovar
- Peritonitis
Return to contents
What is the temperature during inflammation of the ovaries in women?
Inflammatory processes often occur in the female genital organs. They are dangerous because they can harm the entire body as a whole. As a result, the normal state of the appendages and uterus is disrupted. Very often, an ectopic pregnancy is provoked or it does not occur at all.
It is possible to prevent dangerous consequences only through early diagnosis and modern treatment. It is the symptoms of inflammation of the ovaries and appendages that will be discussed in this article.
Judging by its appearance, the ovary is comparable to a peach pit, the length of which does not exceed 4 centimeters and 2.5 centimeters in width.
In this case, the thickness of the paired organ is 1-1.5 cm.
The outer layer is well protected by the tunica albuginea.
It has appropriate properties, so pathogens do not penetrate inside the ovary.
Thanks to this membrane, inflammatory processes develop less frequently than in the fallopian tubes and the uterus itself.
The next layer is the cortex. Several follicles of unequal maturity are constantly present on its surface. These capsules look like bubbles filled with liquid, and a full-fledged egg should grow in them. When this process is completed, ovulation occurs. As a result, the follicle wall is destroyed, and the egg is ready to meet sperm for the purpose of fertilization. If conception does not occur, it dies, and if not, it begins to move through the tubes to gain a foothold in the uterus.
As for the ovaries themselves, they are responsible for the formation of key female hormones - progesterone and estrogen. Thanks to these substances, reproductive function is carried out.
Inflammation is often called an ovarian cold. In fact, if the body is overcooled, it is much easier for pathogenic microorganisms to enter the genitourinary system.
Reference! In the presence of a focus of infection, inflammation of the ovaries develops. In most cases, the source of infection is the omentum or fallopian tube.
The symptoms themselves that a woman has a cold on her ovaries are quite varied, but the principles are non-specific, since they can be confused with other diseases. Under the influence of the disease, the structure of the organ itself changes.
Such sensations indicate the presence of acute inflammation of both the ovaries and fallopian tubes. Discomfort occurs in the right or left side because the organ increases in size due to swelling and the action of biologically active organisms.
Important! The painful sensation is primarily of a pulling and aching nature. The intensity increases if the visceral peritoneum is involved.
As for the duration of pain, it varies depending on the type of inflammation and treatment, if any. Sometimes discomfort can last up to four weeks.
This reaction of the female body is nonspecific. It occurs mainly as a response to the ingestion of an external protein. A febrile state appears because conditions are formed that are unfavorable for pathogenic agents, but they become optimal for maintaining the functioning of the immune system as a whole.
Attention! The increase in temperature is caused by the action of biologically active substances, for example, fragments of provocateurs and pyrogens.
The following stages of development of a febrile state are distinguished:
- temperature increase. The rate of increase in indicators depends on the properties of the provoking virus. The woman begins to feel chills, indicating the activation of heat-saving mechanisms;
- plateau stage. The feeling of chills disappears here, so temperature readings stabilize. The maximum figure can be 39 degrees, but it is sometimes exceeded if complications develop;
- decrease in temperature. This happens both abruptly and gradually. The drugs taken during treatment have an effect.
Inflammatory processes often affect the gastrointestinal tract. Sometimes the following symptoms occur:
- nausea and frequent vomiting. All this happens reflexively, since there is a response to painful stimulation. The body also reacts in this way to an increase in temperature;
- diarrhea. This sign indicates intoxication of the body when the intestines are irritated;
- defecation. It occurs due to the fact that the inflammatory focus affects the rectum.
Important! These signs most often appear in a single case.
Normal secretion involves a small amount of odorless, transparent fluid. At the same time, a woman should not complain about discomfort.
Foci of inflammation are manifested by pathological vaginal discharge. They talk about the presence of infection and the body’s fight against it.
There are such secretion options:
- serous. Observed as a result of damage to the cervix and the organ as a whole;
- purulent. This is a specific sign indicating that the pathogens are of bacterial origin;
- bloody. There is an inflammatory reaction. The discharge is light, scanty, dark in color, and accompanied by discomfort in the lower abdomen.
Attention! If you observe this symptom, you should urgently visit a gynecologist’s office.
Normally, the menstrual cycle should be regular, sometimes slight deviations are allowed.
The arrival of menstruation without interruption indicates that the production of all hormones is balanced, and the body is ready for the potential conception of a baby.
The basis of the menstrual cycle is the renewal of the uterine mucosa and the formation of the egg.
The process includes two phases, each of which is responsible for the production of certain hormones. The cycle repeats again if the egg has not been fertilized, and is suspended otherwise during pregnancy and breastfeeding.
- hormonal imbalance;
- damage to the uterine lining;
- lack of ovulation;
- failures in endometrial regeneration.
Important! Sometimes there is heavy or scanty discharge during menstruation, severe pain localized in the abdomen, and increased duration of secretion.
This type of pathology does not occur often, but such an outcome does occur.
It is worth talking about it because functional and structural changes in the organ are taking place.
As a result, the production of estrogen and progesterone decreases.
It is known that hormones are responsible for the regulation of key physiological processes. If there is a shortage or excessive quantity, the following consequences arise :
- damage to the central nervous system;
- depression;
- heart diseases;
- increased blood pressure;
- metabolic disease.
This factor is the most common when it comes to the consequences of pathology. The inability to conceive a baby is due to impaired cell production and hormonal disorders.
Very often, infertility occurs against the background of damage to the fallopian tubes, and it is this factor that accompanies oophoritis. Due to inflammation, the pipes narrow and change, causing partial or complete obstruction.
Discomfort occurs due to the fact that the inflammatory process affects the anterior wall of the peritoneum. Muscle contraction occurs reflexively. This is a kind of response to pain arising from the lesion.
Important! Muscle tension reduces irritation and tension in the area, which relieves pain.
There are also signs of a complicated pathology:
- localization of pain in the right hypochondrium and upper abdomen. This condition is characterized by an increase in temperature, disruption of the normal functioning of the liver, and a yellow color on the skin;
- on the affected side, the abdomen swells. This sign can be determined by palpation or visually.
These conditions are considered potentially dangerous, so it is necessary to resort to surgical intervention in order to minimize dangerous consequences.
There are three forms of ovarian inflammation, namely acute, subacute and chronic.
The signs may be similar, but their severity varies.
Acute inflammation has pronounced symptoms. As a rule, it is at this stage that the patient decides to contact a specialist so that he can prescribe the appropriate treatment.
The symptoms here are as follows:
- pain in the lower abdomen. Localization can be on one or both sides. Sometimes the discomfort spreads to the groin area;
- headache , aches in muscles and joints;
- chills accompanied by fever;
- painful and frequent urination;
- metabolic disease;
- bleeding on days other than your expected period;
- pain during intimate contact;
- constant change of emotional state.
Attention! Often, palpation cannot be used for diagnosis, since pain and swelling are recorded.
Subacute inflammation mainly occurs in those suffering from tuberculosis. The signs of the disease are similar to those mentioned above, but they are much more difficult to determine.
Chronic inflammation occurs if the patient does not see a doctor or the prescribed treatment is not completed. Sometimes the disease worsens, but the condition is replaced by periods of temporary improvement.
Relapses do not occur if a woman complains only of pathological secretion or menstrual irregularities. The same symptoms are observed, for example, with gonorrhea. However, over time, adhesions form and the walls of the fallopian tubes thicken.
This or that treatment tactic for a woman who has a cold in her appendages should be based
on the form of the disease and the type of infection that provoked it.
When it comes to the acute form, the woman is placed in a hospital for constant stay in bed under the supervision of medical workers.
Cold compresses are placed on her lower abdomen. In addition, it is customary to use antipyretic, analgesic and antibacterial agents. Also, based on the individual clinical picture, antibiotics are prescribed.
The subacute form of inflammation involves quartz irradiation of the affected area. If we are talking about the chronic type, then medications, medicinal baths and elements of physiotherapy are used:
Reference! If the causative agent of the pathology is a sexually transmitted infection, then both partners must undergo treatment.
Symptoms of the inflammatory process occurring in the ovaries and appendages can be different. First of all, the signs make themselves felt depending on one or another form of neglect of the disease. It is important to listen to your own body and notice early symptoms so that you can diagnose the disease in time and begin its treatment.
source
Inflammation of the appendages and ovarian cysts have become a real scourge plaguing modern women of reproductive and elderly age. What signs and symptoms do women, including those in an interesting situation, need to know in order to immediately contact a gynecologist?
In gynecology, the term “appendages” is used to collectively refer to the ovaries and fallopian tubes.
Inflammatory processes in the ovaries and tubes proceed in the same way and very rarely develop in isolation, so the disease has received a mixed name - salpingoophoritis (adnexitis).
The lesion begins from the inner layer of the tubes, covers the middle and outer membranes, then flows to the integumentary epithelium of the ovaries. In this case, pathological processes can affect both ovaries (both tubes) or be localized only on one side.
Inflammatory processes in the ovaries and fallopian tubes are caused by infectious pathogens, including sexually transmitted ones. These include:
- chlamydia, gonococci, myco- and ureaplasma;
- staphylococcus, streptococcus, Escherichia coli,
- Mycobacterium tuberculosis and other pathogenic viruses and bacteria, as well as non-spore-forming anaerobes.
As a rule, these infectious pathogens come from the lower genital tract (ascending infection), so advanced inflammation of the vaginal mucosa (vaginitis, colpitis) and/or external genital organs (vulvitis) will inevitably lead to inflammation of the appendages.
Less commonly, inflammatory pathogens can enter from:
- peritoneum;
- rectum or appendix;
- spread through the bloodstream.
Based on the localization of the inflammatory process, it can be assumed with 90% probability which of the infections caused adnexitis:
- bilateral inflammation is a consequence of damage by chlamydia, gonococci or tubercle bacilli;
- unilateral (right or left) – a manifestation of “activation” of E. coli, staphylococci, streptococci or enterococci.
Of the inflammatory diseases that affect only the ovaries, a cyst is the most common type of pathology. An ovarian cyst is a benign neoplasm in the form of a thin-walled “sac” filled with semi-liquid contents, which can occur outside or inside the organ itself.
There are the following types of cysts:
- follicular (functional);
- luteal (corpus luteum);
- hemorrhagic;
- dermoid;
- endometriosis (“chocolate”);
- cystadenoma;
- polycystic syndrome.
In 70% of cases, the cyst arises as a functional feature of “defective” maturation of the egg and goes away by the next menstruation. In other cases, it can not only reach enormous sizes, but also degenerate into a malignant tumor. With early diagnosis and treatment, situations where surgical intervention is required are quite rare.
An ovarian cyst can be a consequence of surgical interventions, inflammatory diseases or hormonal imbalance, including the resulting imbalance of hormones in the body of a pregnant woman.
The cause of the formation of a cyst in the left ovary may be chronic colitis. The causes of a cyst in the right ovary include not only colitis, but also surgery to remove the appendix.
The most common and first cause of inflammation of the appendages is considered to be hypothermia of the body - wearing clothes and shoes that are not in season, ignoring drafts, frequently getting wet feet, prolonged swimming in cold water.
Other predisposing factors that weaken the immune system and trigger the development of the disease include:
- regular large blood losses during menstruation;
- chronic diseases of internal organs and untreated infectious diseases;
- overwork, stress and depression;
- excessive enthusiasm for diets;
- practicing “male” sports or work associated with increased physical exertion.
Women need to pay special attention to the treatment of mechanical tissue damage received during an abortion or during labor. The same warning applies to women who have undergone gynecological surgery.
Provoking factors contributing to the occurrence of ovarian cysts include:
- the appearance of menstruation before the age of 11 years;
- irregular menstrual cycle;
- taking the oncological drug Tamoxifen;
- diseases caused by hormonal disorders;
- complications after gynecological operations;
- obesity;
- smoking.
For the formation of an ovarian cyst, which can degenerate into a malignant tumor, the provoking factor is considered to be a female age threshold over 40 years.
Signs of inflammation of the uterine appendages and ovarian cysts are varied and depend on the stage and degree of spread.
Common signs of ovarian inflammation are disruption of the menstrual cycle, decreased libido, pain in the lower body, irritation, itching and vaginal discharge.
Pain in the lower abdomen can be acute, paroxysmal or almost continuous, dull and aching. Often women complain of pain in the lumbar or sacral area. All types of pain intensify after cooling, before menstruation (dysmenorrhea). Women receive particular complaints about pain during sexual intercourse.
Symptoms of ovarian inflammation that cause particular discomfort are purulent or serous discharge (leucorrhoea). The released liquids can be colorless, white, gray. In purulent cases they have a dirty yellow or swamp-greenish tint, and are accompanied by an extremely unpleasant odor.
As a result, heavy discharge causes irritation of the mucous membranes of the vagina and severe annoying itching of the external genitalia.
Acute inflammation of the appendages is accompanied by:
- fever above 38°C, chills and fever;
- nausea, general lethargy and sharp cutting pain in the solar plexus;
- purulent discharge;
- the appendages increase in size and upon palpation respond with acute unbearable pain, and when the uterus is displaced, painful sensations occur.
The duration of the acute course is 1-2 weeks, after which the disease becomes subacute and then chronic and will require significant efforts from the woman for a complete cure.
The chronic course is dangerous due to the absence of pronounced symptoms. In most cases, a diagnosis is made only after a woman consults a gynecologist with the problem of being unable to get pregnant for a long time.
During a gynecological examination, the doctor feels “heaviness” when palpating the appendages; during such manipulation, women complain of moderate pain.
As a result of a chronic purulent inflammatory process, not only the appendages themselves are affected, but also the inner lining of the abdominal cavity - adhesive connections between the layers of the peritoneum occur, which are manifested by constant constipation or diarrhea.
In addition to stool disorder, chronic adnexitis is always accompanied by a faint, blurred pain in the area below the stomach.
As a rule, a functional ovarian cyst does not manifest itself in any way and is diagnosed accidentally during an ultrasound examination of another disease.
Other types of ovarian cysts are characterized by the following symptoms:
- pallor, attacks of dizziness (up to loss of consciousness);
- heartburn and constipation;
- increased hair growth on the body and face;
- painful sensations during sexual intercourse;
- nagging dull pain from the affected ovary during menstruation;
- pain in the lower abdomen that appears after physical activity;
- frequent false urge to urinate and/or defecate;
- intermenstrual bleeding or slight spotting;
- delay or severe disruption of the menstrual cycle;
- sudden loss of body weight;
- an increase in the volume of the abdominal circumference and palpation of the compaction;
- unsuccessful attempts to get pregnant.
In cases of cyst rupture, women complain of nausea and uncontrollable vomiting, spotting appears, body temperature rises sharply and pain appears characteristic of an “acute abdomen”. If such symptoms occur, urgent hospitalization is required.
In pregnant women, pain in the ovarian area can be caused by the following reasons:
- ectopic pregnancy;
- sprains caused by the growth of the uterus;
- inflammation of the appendages or the ovaries themselves (oophoritis);
- chronic intestinal diseases and constipation;
- ovarian cyst.
Women who were able to become pregnant against the background of a chronic inflammatory process in the appendages should prepare for the inevitable process of exacerbation.
Manifestations of adnexitis will depend on the type of infectious agent. The “first signs of return” of inflammation will be the appearance of leucorrhoea and causeless pain in the lower part of the body.
Particularly noteworthy are cases of not repeated inflammation of the appendages during pregnancy, but direct infection during it.
It is recommended to terminate pregnancy if adnexitis is caused by pathogens of syphilis or gonorrhea. In other cases, the woman has to make a difficult choice between maintaining the pregnancy and terminating it, since antibacterial treatment of inflammation of the appendages threatens the normal development of the fetus, and at the same time, the pregnancy is very difficult to maintain due to the constant threat of miscarriages.
The follicular type of neoplasm and corpus luteum cyst are asymptomatic, do not require treatment and disappear before the 20th week of pregnancy.
A danger to the health of a pregnant woman and to the normal development of the fetus are “asymptomatic” ovarian cysts that are too large (over 6-8 cm) or external forms in the form of a “hat on a stem”. Such neoplasms must be removed between 14 and 16 weeks of pregnancy.
Constant and severe pain in the lower abdomen is caused to a pregnant woman by “chocolate” (endometriotic) types of ovarian cysts. They are dangerous due to possible growth (up to 30 cm) and subsequent rupture.
During early pregnancy, characteristic symptoms that are caused by an increase in the volume of the cyst above 5 cm include:
- pain in the ovaries and pelvic area;
- swelling;
- bloating;
- frequent urination.
An immediate call to the ambulance is necessary in the following cases: severe nausea, vomiting, fever, severe pain in the lower body.
If signs of a cyst or suspected inflammation of the ovaries are detected, the symptoms should become an unconditional motivator for a visit to the gynecologist. Don't delay treatment! Ignoring can lead to regular instability of the menstrual cycle, persistent infertility, pathological intrauterine pregnancies of tubal or abdominal forms; in advanced cases - to the formation of purulent abscesses and peritonitis with a fatal outcome.
Attention! According to statistics, 25% of women are susceptible to relapses of repeated inflammation in the ovaries. So, after the course of treatment, you need to radically reconsider your lifestyle and behavior.
source
Inflammation of the ovaries is a negative oppression of tissues in the genitourinary system, as a rule, it has infectious and inflammatory characteristics. This disease often does not occur separately.
It is no different from other diseases, since it has three stages of development: subacute, acute and chronic. Each has its own pathogenesis (degree of development). In turn, each of the degrees has its own range of treatment methods in gynecology. But it is simply impossible not to treat this disease.
For greater clarity in the course of the disease, you should first understand what exactly the ovaries are, why a woman needs them, and about the organs that are located in close proximity to them.
This organ has two main jobs: reproductive and hormonal. The fact is that it is in the ovaries that the egg is synthesized, which, through the fallopian tubes, ends up in the uterus. Here the egg, attaching to the uterine walls, continues its formation. And as a result - pregnancy.
Causes of chronic oophoritis
- Infection: germs, viruses, fungi.
- Autoimmune inflammation develops as a result of: chronic diseases of the genital area, radiation, hormonal disorders, enzymatic defects, etc.
Factors that increase the risk of chronic ovarian inflammation
- Sexually transmitted infections
- Long-term wearing of an intrauterine device
- Bacterial vaginosis
- Urogenital diseases of the sexual partner
- Abortion
- Complicated childbirth
- Gynecological therapeutic and diagnostic procedures: hysteroscopy, hysterosalpingography, diagnostic curettage, etc.
- Sexual intercourse during menstruation
- Obesity
- Inflammation of the urinary system
- Anemia
- Hypovitaminosis, vitamin deficiency
- Intestinal dysbiosis
- Immunodeficiency, decreased body resistance
- Site of chronic infection (tonsillitis, stomatitis, sinusitis, etc.)
- Early onset of sexual activity
- Frequent change of sexual partners, active sex life
- Unfavorable living conditions, alcoholism, drug addiction
- Stress
- Sedentary lifestyle
Please note: Why do the ovaries hurt 10 days before your period?
What contributes to the chronic course of the disease?
- Features of the infectious pathogen
- Violation of general/local immunity
- Chronic gynecological diseases, including dishormonal diseases
- Untreated/undertreated acute oophoritis or adnexitis
Risks of exacerbation of chronic oophoritis
Causes of exacerbation of chronic inflammation of the appendages:
- Hypothermia
- Overwork
- Psycho-emotional stress
- Physical overload
- General disease or condition leading to decreased immunity
- Poor intimate hygiene
- Use of vaginal hygienic tampons, douching
What causes oophoritis?
| Nature of infection | Frequent pathogens |
| STIs – sexually transmitted infections | Chlamydia (30% of cases) Gonococci (40%) Trichomonas (20%) Ureaplasma (mycoplasma) |
| Commensal microbes or opportunistic microflora inhabiting the human body, including the vaginal environment | Escherichia coli Enterococci Proteus Klebsiella Bacteroides Staphylococci Streptococci Peptococci Peptostreptococci Gardnerella etc. |
| Viruses, including sexually transmitted ones | Herpes virus type 2 Cytomegalovirus |
| Fungi | Candida Actinomycetes |
| Tuberculosis | Mycobacterium tuberculosis |
How do microbes enter the ovary?
Pathogenic microorganisms enter the uterine appendages in three ways:
- Ascending - the infection spreads from the vagina and/or uterine cavity through the fallopian tube to the ovary.
- Descending - microorganisms penetrate the ovary from the peritoneum (appendix, sigmoid and/or rectum, etc.)
- Hematogenous - pathogenic agents are delivered to the ovary via blood/lymph flow from a distant site.
Causes and pathogens
The disease can be caused by the following pathologies:
- chlamydia
- gonorrhea
- t richomoniasis
- tuberculosis
- staphylococci (rare)
- streptococci
- Candida
- coli
The development of the disease is influenced by the following factors:
- menstrual cycle
- hypothermia
- surgical manipulation of the genitals
- abortions
- installation of an intrauterine device
In most cases, ovarian inflammation is a secondary process. This means that the infection first develops in the fallopian tubes, uterus or cervical canal, and then moves upward. In rare cases, pathogens of oophoritis penetrate the gonads through lymph and blood.
If the disease is not treated, the infection spreads to the fallopian tubes, causing them to thicken. Pathological changes in the ovaries negatively affect periadnexitis, and the accumulated inflammatory exudate causes the accumulation of pus and forms pyovar. The infection may subsequently extend beyond the ovary and be accompanied by pelpioperitonitis. Oophoritis can also be caused by appendicitis, from which the infection spreads to the ovaries.
Oophoritis develops actively if the following factors are present:
- endocrine system diseases
- infections in the body that develop chronically
- stressful situations and overwork
- diseases of the genitourinary system
- lack of a regular sexual partner
- unprotected sexual intercourse
- smoking
- promiscuity
Symptoms of oophoritis
Signs of chronic ovarian inflammation in remission:
- Menstrual irregularities: - amenorrhea - irregular menstrual cycle
- Infertility
- Chronic pelvic pain syndrome
- Decreased ability to work, irritability, mood instability, sleep disturbance
Outside of exacerbation, chronic oophoritis can be asymptomatic or with minor, erased clinical manifestations
Signs of chronic oophoritis/adnexitis
| Signs | Subacute inflammation of the appendages | Chronic inflammation of the appendages |
| Chills, fever | No | No |
| Body temperature | Normal/Not higher than 38 degrees | Norm |
| Abnormal vaginal discharge | Sometimes | No |
| Painful periods | Sometimes | Sometimes |
| Sharp cutting pain in the lower abdomen | Sometimes | No |
| Dull aching pain in the lower abdomen | Yes sometimes | Yes |
| Pain during uterine displacement during bimanual examination | Yes | No |
| Enlargement of the appendages, determined by palpation | Sometimes | No/Heaviness |
| White blood cell count | Normal/ Slightly above normal | Norm |
| Acceleration of ESR | Moderate | Sometimes |
Where does it hurt during oophoritis?
Outside of an exacerbation of the disease, pain may be absent or manifested by unpleasant sensations in the lower abdomen during straining or during sexual intercourse
In the subacute period, during exacerbation:
- Localization of pain: lower abdomen, groin area, sacrum.
- Nature of pain: dull, aching.
- The pain intensifies: - after physical activity - during hypothermia - during any acute non-gynecological diseases (colds, sore throat, bronchitis, cystitis, etc.) - in stressful situations - before and/or during menstruation - after a gynecological examination (bimanual examination) - during or after sexual intercourse
Return to contents
Symptoms
When ovarian inflammation occurs in women, symptoms and treatment vary. The disease is acute, subacute and chronic. Each type of disease is accompanied by characteristic symptoms.
Exacerbation stage
When adnexitis worsens, the following symptoms occur:
- severe pain, pain when urinating;
- constant pain radiating to the lower back or sacrum, lower abdomen, above the pubis;
- a sharp increase in temperature, sometimes up to 39 degrees;
- feverish condition;
- weakness, fatigue;
- bleeding between periods;
- excessive pain during intimacy;
- copious discharge of serous or purulent exudate.
An exacerbation is manifested by another pronounced symptom: inflammatory processes lead to a significant enlargement of the ovaries, the palpation procedure causes pain to the woman. This symptom is determined by the gynecologist when examining the patient. Treatment of adnexitis in the acute stage is carried out in a hospital setting.
Signs of the subacute form
This type of illness is a rare occurrence. The disease develops against the background of mycoplasmosis or tuberculosis. The signs of the subacute phase of the disease are similar to the symptoms of the acute form, but are less pronounced.
Symptoms of chronic inflammation
If not cured immediately, the disease develops into a chronic form. The disease either worsens or subsides. In the acute stage, chronic inflammation of the ovaries manifests itself as follows:
- soreness in the groin, above the pubis;
- increased pain during menstruation;
- sexual dysfunction (low libido, pain during intimacy);
- poorly discharged leucorrhoea;
- menstruation disorder;
- ovarian dysfunction;
- It is impossible to conceive a child even with regular sex life.
The size of the inflamed ovary is increased. When palpating it, pain occurs. Women burdened with adnexitis:
- irritable;
- lethargic;
- suffer from increased fatigue, sleep disturbances, and decreased performance.
Diagnosis of the disease
It is difficult even for an experienced clinician to recognize chronic or subacute oophoritis that occurs with erased symptoms.
Outside of exacerbation of chronic oophoritis, laboratory parameters (general blood count, urine test, blood biochemistry, etc.) do not change.
Data from a “two-handed” gynecological examination are not enough to make a diagnosis.
In some cases, the examination does not find any deviations from the norm.
In others, it reveals limited mobility of the uterus and/or pain, heaviness, and compaction in the area of the uterine appendages.
Ultrasound examination of the pelvic organs in the diagnosis of chronic oophoritis is ineffective (≈55%).
Indirect echo signs of oophoritis (identified in only half of the patients):
- Increased ovarian size
- Ball-shaped form of an inflamed ovary
- Fuzzy contours, thickening of the outer membrane of the ovary
- Echo heterogeneity or hypoechogenicity of the ovarian stroma
- Absence or poor visualization of follicles in the ovary
- Free fluid in the pelvis
- Pain during transvaginal ultrasound
Smear for urogenital flora
This is a bacteriological examination of a smear from the urethra, vagina and cervical canal.
Examination of smears under a microscope can detect a large number of leukocytes (a sign of inflammation), dysbacteriosis, pathogenic microorganisms (STIs)
If necessary, an ultra-precise examination of vaginal discharge is carried out for ureaplasma, mycoplasma, chlamydia, cytomegalovirus, herpes virus, HPV, etc. using the polymerase chain reaction method.
CT or MRI of the pelvis with contrast
Computer or magnetic resonance imaging with intravenous contrast is a good help to clarify the diagnosis of chronic oopharitis, to distinguish it from tumors and other diseases of the appendages.
Needle biopsy of the ovary
Ovarian biopsy followed by histological examination is the gold standard for diagnosing autoimmune chronic oophoritis.
Laparoscopy is the most effective method for detecting chronic oophoritis.
Indications for therapeutic and diagnostic surgery:
- Persistent pain syndrome that is not amenable to drug treatment
- Suspicion of a dangerous complication of chronic oophoritis
- Infertility
Return to contents
How to treat chronic oophoritis of the ovary?
/consultation with a doctor is required/
Medicines for the treatment of chronic oophoritis are prescribed by a doctor
Antibacterial therapy for chronic inflammation of the ovaries, as a rule, is not used, or is prescribed in individual cases
Indications for the treatment of chronic inflammation of the appendages with antibiotics:
- Rational antibiotic therapy has not previously been carried out
- Period of exacerbation of the disease
- Prescription of therapeutic actions that aggravate the chronic inflammatory process: administration of staphylo- or gonova vaccines, physiotherapy, etc.
Drugs for the treatment of oophoritis
European recommendations for outpatient antibiotic therapy of nonspecific inflammatory diseases of the uterine appendages:
| Name of active substance | Reception mode |
| Moxifloxacin 400 mg | 1 time per day, orally, for 14 days |
| (1) Levofloxacin 500 mg + (2) Metronidazole 500 mg | (1) once a day, orally, for 14 days + (2) 2 times a day, orally, for 14 days |
| (1) Ceftriaxone 500 mg + (2) Azithromycin 1.0 g | (1) intramuscularly, once + (2) 1 time orally, a week later 1 more time orally |
Prescribed according to indications, according to an individual regimen: - while taking antibiotics, - for the treatment of mycoses of the urogenital tract.
- Fluconazole
- Introconazole
Anti-inflammatory treatment
Anti-inflammatory and at the same time analgesic treatment of chronic oophoritis is carried out with drugs from the NSAID group.
- Diclofenac (tablets 50 mg) – orally, 1 time per day + Diclofenac (suppositories 100 mg) – rectally, at night
- Naproxen (tablets 50 mg) - orally, 1 time per day + Naproxen (suppositories 50 mg) - rectally, at night
- Nimesulide - 100 mg 2 times a day, after meals (for severe pain)
Antihistamines
To reduce inflammatory reactions, histamine H1 receptor blockers are prescribed, for example:
- Suprastin – 1 tablet 1-2 times a day
- Tavegil – 1 tablet 1-2 times a day
- Cetirizine - 1 tablet 1 time per day
- Loratadine - 1 tablet 1 time per day
Vitamin therapy
Vitamins are used to increase the body's protective properties and prevent relapse of the disease.
- Vitamin B1 - 1 ml intramuscularly, 10 injections, every other day
- Vitamin B6 - 1 ml intramuscularly, 10 injections, every other day
- Vitamin A - capsules of 5000 IU, 1 capsule 10-15 minutes after meals for a weekly course
- Vitamin C - 50 - 100 mg orally, 3-5 times a day for a two-week course
- Vitamin E - orally 50 - 100 mg, 1-2 times a day, weekly course
On the recommendation of the attending physician, multivitamin preparations can be used in courses, for example: Vitrum, Unicap-T, Triovit, Multi Tabs, etc.
Absorbable agents with anti-inflammatory effect
- Wobenzym – 5-7 tablets 3 times a day for 2-4 weeks
- Magnesia (magnesium sulfate) 25% – intramuscularly, 5 ml, 1 time per day, for 1-3 weeks
- Serta (serratiopeptidase) - 5-10 mg, 3 times a day after meals, for 2-4 weeks
Eubiotics or probiotics
To maintain healthy vaginal microflora, prevent and treat intestinal dysbiosis, probiotics are prescribed.
- Linex
- Bifiform
- Acipol
- Normobakt
- Buck-set forte
- Bifidum, etc.
Locally, in the form of vaginal suppositories/capsules:
Features of the treatment of bilateral oophoritis
An important component of the complex treatment of chronic oophoritis is to increase the immune reactivity and nonspecific defenses of the body.
Immunostimulants are prescribed individually, after consultation with an immunologist, strictly as prescribed - there are contraindications!
- Levamisole – as an immunomodulator, with a proven decrease in the activity of the T-immune system, orally according to an individual regimen.
- Pyrogenal - intramuscularly, 1 time per day, every other day or at two-three-day intervals in an individual dose, a monthly course. Prescribed for prolonged recurrent oopharitis, also for resorption of adhesions.
- Timalin or T-activin is used according to an individual regimen for the correction of combined immunodeficiencies, autoimmune and allergic diseases.
- Lykopid is a highly effective synthetic immunomodulator that stimulates all forms of anti-infective defense. For chronic oophoritis, take 1 mg 1-2 times a day for a 10-day course.
- Tamerit (Galavit ®) is an immunomodulator with an anti-inflammatory effect. It is used in the form of intramuscular injections according to an individual scheme.
- Polyoxidonium – has an immunostimulating and detoxifying effect. It is used according to indications: in the form of injections, tablets, rectal suppositories - according to an individual scheme.
- Bestim (0.1 mg) is an effective drug for restoring immunological reactivity and complex treatment of chronic viral infections, chlamydia, tuberculosis. It is administered intramuscularly 1 time per day. Course of treatment: 5 injections.
Interferons and interferon inducers
To support the functions of the immune system and strengthen antiviral immunity in the complex therapy of chronic oophoritis, interferon preparations and their inducers are used according to indications. For example:
- Cycloferon - in the form of intramuscular injections
- Neovir – as an immunostimulant, for the treatment of pelvic inflammation
- Viferon - in the form of rectal suppositories for oophoritis
- Reaferon – capsules, orally, according to an individual regimen
Physiotherapy
(in the absence of contraindications)
- Electrophoresis of iodine, zinc, copper - on the appendage area
- Ultraphonophoresis - on the area of the appendages
- Ultraviolet irradiation of the bikini area
- Magnetic laser therapy
- Low frequency magnetic therapy
- Ozone therapy, etc.
Methods of nonspecific anti-inflammatory therapy improve microcirculation, prevent the formation of microthrombi and necrosis in the pathological focus, and activate all parts of local immunity.
In case of intolerance to drug treatment, many researchers consider ultraviolet irradiation of blood to be a promising direction in the treatment of chronic oophoritis.
Ultraviolet blood irradiation procedure Plasmapheresis
There is clinical evidence of the successful immunocorrective effect of plasmapheresis in patients with chronic oophoritis.
Therapeutic exercises for chronic oophoritis
Congestion in the abdominal cavity contributes to impaired microcirculation, the appearance of hypoxia, decreased local immunity, and the development of chronic inflammation and adhesions.
Regular physical therapy eliminates these phenomena, heals the genitourinary area, and strengthens the pelvic floor muscles.
Folk remedies for the treatment of oophoritis
What it is? Mumiyo (mountain oil) is a resinous substance formed in the mountains. It is a natural complex of organic biologically active substances. It has a powerful immunostimulating effect, enhances the processes of hematopoiesis and regeneration.
Where to get it: It’s safer and more reliable to buy ready-to-use mumiyo at a pharmacy.
How to use: Take once a day: 0.2-0.5 g in the morning, strictly on an empty stomach, with water (50-100 ml) or warm milk. Course of treatment: 1-2 months.
Aloe – nutritional mixture
For chronic inflammation of the appendages, it is useful to take a general tonic based on bioactive juice from aloe leaves, which increases the body's resistance to infection.
Please note: Pregnancy with polycystic ovary syndrome symptoms and causes
What you need: Aloe juice – 100 g Walnut kernels – 1 glass Natural honey – 300 g Fresh lemon – 3 pieces.
How to do it: Cut off the leaves of indoor aloe (15 cm or more in length). Place them in a paper bag and keep them in the refrigerator for 7 days to increase the activity of biological substances.
Then mince the aloe leaves and squeeze through cheesecloth. Boil the resulting juice for 3 minutes. Cool. Mix with chopped nuts and other ingredients. Keep refrigerated.
How to use: Take 1 teaspoon 30 minutes before meals 3 times a day for a month. The course of treatment can be repeated.
Stoneweed - a decoction of stems and leaves
Kostyanika is a little-known effective folk remedy for inflammatory diseases of the female genitourinary system.
What you need: Drupe leaves and stems – 2 tablespoons
How to do it: Pour boiling water over the raw materials. Heat in a water bath for 30 minutes. Cool, strain, add warm boiled water to obtain the original volume (250 ml). Keep refrigerated.
How to use: Take 2 tablespoons 30 minutes before meals 3 times a day for 3 weeks. After a 7-day break, the treatment course can be repeated.
Treatment of the disease
Treatment tactics are determined after an accurate diagnosis has been established. The choice of treatment option depends on several factors:
- stages of the disease;
- causes of pathology;
- symptoms.
Only the acute form of oophoritis is treated in a hospital setting. The remaining stages of ovarian inflammation with mild symptoms can be treated at home.
Antibiotic therapy
When ovarian inflammation is detected in women with acute symptoms, treatment with these drugs is mandatory. During diagnosis, it is only necessary to identify the type of pathogen and its sensitivity to the drug. The dosage is selected individually to ensure the required concentration of the antimicrobial component. In severe cases of the pathology, several medications may be prescribed at once.
You cannot self-medicate, as there are several groups of antibiotics with their own characteristics. A doctor can figure them out; he prescribes medications, taking into account diagnostic data.
For inflammation of the ovaries in women with pronounced symptoms, prescribe treatment at home, and a quick recovery can only be achieved with the help of properly selected antibiotics. The table presents the main medications for the treatment of ovarian inflammation.
Streptocide, Sulfasalazine, Co-Trimoxazole
Strong drugs with a wide spectrum of action. Used as injections.
They show high efficiency and are used in the form of injections and tablets.
They have few side effects, but are low in effectiveness.
Has many side effects.
Often prescribed and well tolerated.
To achieve maximum antimicrobial effect, antibiotics are often combined.
Application of candles
For severe inflammation of the ovaries in women with complex symptoms, treatment with antibiotics is supplemented with suppositories. Vaginal suppositories that contain:
- oak bark;
- walnut extract;
- propolis.
A positive result is shown by the use of Clindamycin suppositories. They are administered at night. Metronidazole suppositories are used morning and evening. Voltaren suppositories have a calming effect and are recommended for complex treatment.
For chronic inflammation of the ovaries in women with mild symptoms, treatment with suppositories is recommended to be carried out regularly in courses for the purpose of prevention.
Forecast and prevention of the disease
The prognosis of the disease largely depends on the cause of chronic inflammation of the ovary, the individual characteristics of the immune system and the hormonal background of the patient. With the right management tactics, the outcome of oophoritis is optimistic.
Measures to prevent chronic oophoritis:
- Healthy lifestyle
- Balanced diet
- Body weight control
- Planning pregnancy (avoid abortion)
- Barrier contraception (condom)
- Correction of hormonal activity of the ovaries (use of combined oral contraceptives as recommended by a doctor)
- Spa treatment
- Physiotherapy
- Regular examination by a gynecologist once every 6 months
source
Treatment of ovarian inflammation
Only after establishing a diagnosis and determining the stage of the disease, it becomes clear how to treat inflammation of the ovaries in women.
Therapy depends on the infection that provoked it and the patient’s tolerance to medications. The treatment is gradual and each stage has its own methods and therapeutic goals. Patients with acute oophoritis are subject to hospitalization with the mandatory use of antibacterial drugs. The doctor prescribes complex treatment. Severe pain is relieved with painkillers.
In parallel, antihistamines, antivirals, and immunostimulating drugs are used. After the symptoms of acute inflammation have reduced, continued treatment on an outpatient basis is indicated.
During this period, physiotherapy is carried out under the control of clinical and laboratory data: medicinal electrophoresis, radon baths, magnetic therapy, phonophoresis with magnesium or calcium.
Treatment of chronic ovarian inflammation occurs over a long period of time. Therapeutic measures are aimed at achieving an antimicrobial, anti-inflammatory, analgesic effect, as well as restoring the functions of the hormonal, reproductive, nervous and vascular systems. Acupuncture, acupressure, psychotherapy are prescribed, and sanatorium-resort treatment has a beneficial effect.
An important part of therapy is restoration of the menstrual cycle. The pathology must be treated methodically so that the ovary does not stop functioning, which is important for women planning a pregnancy.
Only after regulating the function of the ovaries can one begin to solve the problem of infertility. In case of extensive scarring and adhesions in the pelvis and purulent formations, surgical treatment with dissection and removal of adhesions is indicated.