Character of the current
Uveitis is classified as:
- acute: sudden onset, limited duration;
- relapsing: with periods of remission of at least 3 months, without treatment;
- chronic: return of episodes of the disease, despite therapy, less than 3 months after its completion.
The treatment regimen for uveitis is individual and based on the results of a clinical and ophthalmological examination and identification of the etiological factor; Both local and systemic therapy are used. In case of complications, surgical intervention is performed.
Inflammation of the uveal tract accounts for 30-50%; in 25% of patients, the pathology is complicated by persistent visual impairment and blindness.
Forms of uveitis are associated with the involved anatomical site and are represented by iritis, iridocyclitis, choroiditis, and chorioritinitis.
A developed vascular network and slower blood flow, against the background of predisposing factors, contribute to the accumulation and retention of pathogens that begin to actively multiply.
The blood supply and innervation of the anterior and posterior sections are separated, so inflammatory processes occur in isolation.
Causes and predisposing factors of uveitis
Predisposing factors include:
- genetic predisposition (presence of certain genes);
- smoking;
- a number of diseases: AIDS, autoimmune diseases/spondyloarthropathy/collagenosis, tuberculosis, sarcoidosis, psoriasis, ulcerative colitis/Crohn's disease, etc.);
- infections (viruses: herpes, cytomegalovirus, etc., some STIs, toxplasmosis, bacteria, fungi, rickettsia);
- injuries;
- burns;
- allergens;
- hormonal imbalance;
- history of eye diseases;
- taking certain medications;
- chemical exposure, etc.
Uveitis often develops against the background of an underlying systemic disease; about 50% of patients have an idiopathic form. Acute nongranulomatous uveitis is associated with pathologies associated with human leukocyte antigen B27 (HLA B27), including ankylosing spondylitis, inflammatory bowel disease, reactive and psoriatic arthritis, and Behçet's disease. Herpes simplex, herpes zoster, Lyme disease, and trauma are also associated with acute nongranulomatous uveitis.
Chronic non-granulomatous uveitis is diagnosed in juvenile rheumatoid arthritis, chronic iridocyclitis and Fuchs heterochromic iridocyclitis.
Chronic granulomatous uveitis accompanies sarcoidosis, syphilis and tuberculosis.
Posterior uveitis occurs in toxoplasmosis, ocular histoplasmosis, syphilis, sarcoidosis, and in immunocompromised patients with cytomegalovirus, candida, or herpetic infections.
How does it manifest in children?
, as a rule, have an acute onset. First there is severe pain in one eye. Gradually it begins to spread to the head and the part of the face where the sore eye is located. The pain becomes stronger when the eye is illuminated, at night, during palpation.
The vessels become overfilled with blood and then cause irritation to the cornea. As a result, the following symptoms occur:
- blepharospasm - difficulty opening the eye;
- fear of light;
- tearfulness;
- blurred vision;
- swelling of the eyelids
The pupil narrows, becomes sluggish and does not fully respond to light. The iris is somewhat thickened. In the area of the vitreous body and the pupil, a small amount of exudate is first noticed. Subsequently, it becomes larger and begins to spread to the anterior chamber. The moisture in the eye may be cloudy.
This directly depends on the development of the inflammatory process. The main symptom of anterior uveitis is hyperemia in the iris: small vessels dilate greatly.
In the chronic form of the disease, so-called Keppi's nodules are noticed on the iris of the child's eye. These are cellular deposits containing epithelial particles and lymphocytes. At the onset of the disease, eye pressure may be normal or slightly increased.
Posterior uveitis presents with a wide range of symptoms. So, the child complains of blurred vision and pain in the eyes. In addition, you may experience:
- micropsia (the child sees the image in a reduced version);
- macropsia (the image is perceived by the eye in a larger size);
- photopsia (so-called light flashes appear in the eyes);
- metamorphopsia (the child sees the image in a distorted version).
Symptoms of uveitis
General symptoms of uveitis:
pericillary injection;- change in iris color;
- miosis, changes in the contours of the pupil;
- slow/lack of reaction to light;
- accumulation of precipitates;
- inflammatory blood and purulent effusions in the anterior chamber;
- initiation of the adhesive process;
- decreased visual acuity (may initially be absent);
- pain of varying intensity, accompanied by blepharospasm and photophobia (fear of light), for several hours or days;
note
The above symptoms are not necessarily present simultaneously: the longer the pathological process exists, and the stronger its severity, the brighter and more diverse the clinical manifestations. Localization also matters.
The proximity of the endings of the trigeminal nerve leads to irradiation of pain in the facial area: cheeks, jaw, nose, temples, forehead.
This symptom is considered pathognomonic for herpes infection and secondary glaucoma.
Additional symptoms that are important for diagnosis:
- headache;
- hearing impairment/sensorineural deafness;
- hair loss;
- change in mental reactions;
- skin manifestations;
- cough, shortness of breath;
- joint lesions;
- genital ulcers;
- enlarged salivary and lacrimal glands;
- lymphadenitis;
- aphthae in the oral cavity
Differential diagnosis includes the following:
- glaucoma;
- acute conjunctivitis;
- corneal ulcer and ulcerative keratitis;
- corneal abrasion;
- herpetic keratitis;
- intraocular foreign body;
- scleritis;
- keratitis caused by damage from ultraviolet rays.
Anterior uveitis: iridocyclitis, iritis, cyclitis
The iris and ciliary body are involved. Most often, ophthalmologists encounter anterior endogenous uveitis when the etiological factor is internal: general toxic-allergic reactions or metastatic lesions.
Anterior exogenous uveitis is always secondary and develops acutely following trauma, after surgery, perforation of a corneal ulcer, etc.
On palpation, the pain intensifies.
The mechanism of injury is thought to be a combination of microbial contamination and accumulation of necrotic debris at the site of injury, stimulating the body to inflammation in the anterior segment of the eye.
The accumulation of inflammatory elements causes clouding of the aqueous humor of the anterior chamber (hypopyon); in case of hemorrhage (hyphema) against the background of injury, the exudate acquires a reddish tint due to blood. Precipitates are localized in the lower part of the cornea and resemble a triangle, but can cover the entire posterior surface.
Pathologically dilated vessels and swelling against the background of inflammation change the color and pattern of the iris. Deformation of the pupil is a consequence of the adhesive process between the pupillary edge and the anterior surface of the lens, up to complete fusion of the pupil . Communication between the anterior and posterior chambers of the eye is disrupted, leading to increased intraocular pressure or secondary glaucoma. Nutrients and oxygen are supplied in limited quantities, and the developed cataract is accompanied by a decrease in visual acuity.
Iridocyclitis changes the structure of the vitreous body, clouding occurs, and the replacement of normal tissue with connective tissue sharply disrupts the functions of the eye. If it spreads to the retina, retinal detachment may develop.
note
Anterior uveitis, unlike posterior uveitis, is sterile in most cases: the infectious nature of the disease is absent.
More often, the pathology regresses within 1.5 months, but the cause cannot be determined.
Chronic uveitis is represented by blurred vision and slight redness. The patient experiences mild pain and photophobia, except during an acute episode.
Posterior uveitis (choroiditis)
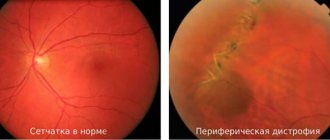
Inflammatory areas with perifocal inflammation (edema and hyperemia) in the fundus can be single or multiple, with variable shape and color. The process involves the retina or choroid: choroiditis, chorioretinitis, retinochoroiditis, retinitis, neuroretinitis. The patient's general condition does not suffer.
The pathology is visualized by ophthalmoscopy; the diagnostic method allows one to examine granulomatous lesions through a transparent or cloudy retina.
In advanced cases, the retina and optic nerve head are affected.
Choroiditis is characterized by loss of visual fields/blind areas, depending on the location of pathological formations : with central localization, visual acuity decreases, complaints of image curvature, the presence of dark spots when examining white objects, photopsia (moving dots, flashes, spots, figures, etc.) .).
Soreness and redness are not typical, the main complaint is blurred vision.
Posterior uveitis symptoms and pain indicate anterior chamber involvement, bacterial endophthalmitis, or posterior scleritis.
Intermediate (medium) uveitis
The process affects the vitreous body (posterior cyclitis, hyalitis) and is bilateral in nature.
Pain and hyperemia are less pronounced than with anterior uveitis, but opacities in the vitreous and visual impairment are more significant.
Moderate uveitis in children and adolescents is difficult to treat and has a high risk of complications.
Diagnosis is difficult, since the anatomical zone is inaccessible to standard ophthalmological diagnostics.
Generalized uveitis (panuveitis)
The most serious form, the entire vascular tract of the eye is involved in the process: the anterior chamber, the vitreous body and/or the choroid.
The infection enters the uveal tract hematogenously, or toxic damage occurs. With severe hypersensitivity reactions and general allergization, conditions accompanied by immunosuppression, panuveitis can also develop.
Clinical manifestations are varied: panuveitis can be present with any symptoms.
Diagnostic features
Need advice from a beauty expert? Get advice from a beauty expert online. Ask your question right now.
A diagnostic ophthalmological set of measures is carried out by a specialist doctor, who, if necessary, prescribes additional biochemical tests or instrumental studies. For differential diagnosis of symptoms, additional consultation with related specialists may be necessary: neurologist, dermatovenerologist, phthisiatrician.
The diagnostic complex of uveitis consists of the following procedures:
- The ophthalmologist notes a change in the color of the iris, narrowing or dilation of the pupils, and notes a unilateral or bilateral lesion.
- Carrying out an ophthalmoscopy procedure with repeated entrainment of the fundus using lenses.
- Measuring intraocular pressure using special devices.
- Determination of symptoms using a perimeter meter measuring the boundaries of visual fields.
- Diagnosis of visual acuity using tables with circles and letters.
- Examination of the eye chambers under magnification using a gonioscope.
- Microscopic examination of structures in uveitis.
- Ultrasound diagnosis of foci of petrification of the eyeball.
- Rheoophthalmography – identification of circulatory disorders with a tendency to slow blood flow. Angiography to determine blood supply disturbances to the visual organ.
- Laser tomography of the retina - detecting changes in the structure or detachment of the retina.
- Optical coherence tomography allows us to determine pathological disorders of the structure of the visual apparatus and damage to the nervous structures of the eye.
- Electroretinography – response to light pulses and adaptation time from darkness to light.
- Laboratory diagnostics include an anticardiolipin test (analysis for syphilis), HLA typing of the virus, PCR diagnostics (analysis for CMV, mycoplasmosis and many other pathogens). Mainly used to determine the symptoms and causes of the disease, differential diagnosis.
The danger of uveitis is its hidden course, masking as other eye diseases, and the rapid development of complications.
With the progression of atypical manifestations and decreased vision, you should not self-medicate using drugs to relieve fatigue or traditional medicine; when the first symptoms are detected, you must contact an ophthalmologist for a thorough diagnosis and effective elimination of pathological processes.
Treatment of uveitis
Uveitis has no standard treatment regimen.
Therapy includes a number of drugs from different groups; their action is aimed at eliminating the etiological factor and relieving pathological symptoms, they use:
- antiviral and immunomodulators;
- vasodilators;
- antibiotics;
- non-steroidal anti-inflammatory drugs (NSAIDs);
- hormones: topical and systemic corticosteroids;
- immunosuppressants;
- antihistamines;
- mydriatics and cytoplegics;
- vitamins;
- enzymes, etc.
Additionally, physiotherapy is used.
Cycloplegic and corticosteroid drops are initially prescribed to relieve pain and reduce inflammation.
Important
Before treatment, intraocular pressure must be assessed and the herpetic nature of uveitis excluded.
In patients with severe cases who do not respond to steroids or who have complications with conventional therapy, immunosuppressants may be used. They are also considered as first-line therapy for the treatment of uveitis in Behçet's disease, Wegener's granulomatosis and necrotizing scleritis. These diseases are often associated with life-threatening systemic vasculitis.
Necrosis factor inhibitors
Immunomodulatory therapy is used in situations where long-term treatment with systemic corticosteroids is necessary. New treatment approaches are drugs that target specific mediators of the immune response. Although these drugs have been studied primarily in patients with rheumatoid arthritis, psoriasis, and Crohn's disease, the similarities in disease pathogenesis have stimulated interest in using these drugs to treat various inflammatory eye diseases. Tumor necrosis factor alpha blocking molecules (eg, adalimumab, infliximab) have been found to effectively modulate the immune response in patients with uveitis.
In June 2020, the FDA approved adalimumab (Humira) for the treatment of noninfectious intermediate uveitis, posterior uveitis, and panuveitis in adults. The basis is the results of two pivotal phase 3 studies: VISUAL-I and VISUAL-II, which showed that adult patients with active and controlled non-infectious intermediate uveitis, posterior uveitis and panuveitis had a significantly lower risk of treatment failure with adalimumab.
Intraocular implants and intravitreal injections
Another new treatment option is the use of intraocular pharmacotherapy through injections and surgical placement of implants. Cataract formation and increased intraocular pressure are common side effects, and the risk of endophthalmitis (usually sterile) is approximately 0.1%.
Cycloplegics
Symptoms and complications of inflammation can be reduced by topical cycloplegic agents. Short-acting drops (cyclopentalate) and long-acting drops (atropine) can be used to reduce photophobia caused by ciliary spasm and to break up or prevent the formation of posterior synechiae (adhesions).
Cyclopentolate causes mydriasis after 30-60 minutes and cycloplugia after 25-75 minutes. The effect lasts up to 24 hours.
Corticosteroids
Corticosteroids slow the release of arachidonic acid from phospholipids, inhibit transcription and cytokine action, and limit the activity of B and T cells. They are indicated for inflammatory diseases of non-infectious causes. Three routes of administration are available: local, periocular and systemic, which is determined individually in each case. Because of serious side effects, especially with high doses and long-term use, immunosuppressants are commonly used for chronic or sight-threatening uveitis.
note
For anterior uveitis, steroid drops are used. Prednisolone acetate 1% is preferred. Sometimes steroids can cause ocular hypertension; therefore, you need to monitor intraocular pressure once a month.
Intravitreal implants of dexamethasone and fluocinolone may be considered as an option to provide prolonged treatment.
Periocular corticosteroids are used to treat posterior uveitis.
In the presence of a systemic disease that additionally requires ophthalmological treatment; For uveitis that does not respond well to other treatments, systemic oral or intravenous therapy is necessary. Prednisone is the most used oral corticosteroid.
Prednisolone ophthalmic (Pred Forte) treats acute inflammation after eye surgery or other types of eye injury. It reduces inflammation and neovascularization of the cornea, inhibits the migration of polymorphonuclear leukocytes and reduces capillary permeability. In cases of bacterial infections, the use of antibacterial agents is mandatory.
Other drugs:
- Dexamethasone (Ozurdex implant for chronic non-infectious uveitis),
- Fluocinolone ophthalmic (Retisert implant),
- Triamcinolone for intravitreal administration,
- Prednisone, etc.
Immunosuppressive agents
Immunosuppressants: antimetabolites, T-cell suppressors and cytotoxic agents. Antimetabolites include azathioprine, methotrexate, and mycophenolate mofetil. T-cell inhibitors include cyclosporine and tacrolimus. Cytotoxic agents: cyclophosphamide and chlorambucil. Most drugs take several weeks to be effective and are initially given in combination with oral corticosteroids.
Diagnostic features
When visiting a doctor, the child should first be examined. Parents should disclose any recent health problems for the child. It is imperative to tell about past infectious and viral diseases, as well as systemic diseases of the baby.
Using a biomicroscopic device, the doctor can examine the affected area of the eye in detail. An ophthalmoscope makes it possible to view the fundus of the eye.
The following methods are also used for diagnosis:
- fluorescein angiography;
- electroretinography.
If the doctor has suspicions about infectious diseases, the child will have to undergo a biochemical and general blood test, and undergo an immunological examination. If toxocariasis is suspected, the child must be tested for the presence of parasites.
If you discover the true root cause of uveitis in a child, it will be easier to treat the disease. Sometimes it is enough to solve the main problem for the choroid to return to normal.
When diagnosing uveitis, it is important to differentiate choroiditis from exudative retinitis. In addition, the doctor will have to find out whether only one eye is affected by the disease, or whether the problem affects both organs of vision.
It is also worth paying attention to:
- type of disease - acute uveitis requires the use of stronger drugs, but short-term treatment, and chronic, on the contrary, the use of less strong drugs, but longer treatment;
- type of relapse;
- type of inflammatory process - it may be granulomatous or not.
Prevention
Preventive measures include:
timely seeking help at the first symptoms of problems with the visual organs;- control of the underlying disease;
- protective measures in case of contact with damaging agents;
- strengthening the immune system;
- avoiding hypothermia;
- proper care when wearing contact lenses;
- taking multivitamin complexes;
- reducing/eliminating contact with allergens;
- treatment of infectious diseases.
Mishina Victoria, doctor, medical columnist
4, total, today
( 50 votes, average: 4.74 out of 5)
Strabismus in children: causes, symptoms, treatment
How to treat stye on the eye?