Rickets is a disease characterized by a disorder of phosphorus-calcium metabolism. Typically, this diagnosis is determined in children at an early age against the background of insufficient amounts of vitamin D - calciferol - in the body. Chronic deficiency of this microelement leads to disruption of the supply of phosphorus and calcium to bone and cartilage tissue. As a result of this, irreversible changes occur in the formation and mineralization of bones, which becomes the cause of rickets in children.
Most people consider this diagnosis to be a relic of years, so rickets is often called not a medical problem, but a social problem, since it is associated with a violation of the conditions of child care. Of course, the modern standard of living of the population and the improvement of the general socio-economic situation in the country should help ensure that this disease remains a thing of the past.
But despite this, rickets still poses a threat to the health of children in the first years of life.
Causes of rickets in children
The causes of rickets in children are conventionally divided into 2 groups. But as a rule, the disease is based on several reasons.
- On the part of the child, predisposing factors to the occurrence of rickets are: prematurity of the child, imperfect liver and kidneys, anatomical and physiological characteristics of the child’s bones (rapid leaching of calcium).
- From the external environment, predisposing factors to the occurrence of rickets are considered:
- Unfavorable course of pregnancy (preeclampsia);
- Pathologies of newborns (asphyxia, birth injuries, etc.);
- Poor nutrition of a child. When breastfeeding, the mother's diet should be varied, including vitamins and minerals. When artificial feeding, use adapted formulas, not milk from cows, goats or kefir. From October to April, children are advised to add vitamin D to their diet;
- Insufficient walks with the child.
When several factors combine in a child’s body, vitamin D deficiency increases, which leads to the development of rickets.
Prevention of rickets
Prevention of rickets in infants is as follows:
- You need to take your baby for walks often. At the same time, the baby’s skin should be in contact with the sun’s rays, so it is best to choose the time for walks before noon and after 3 o’clock in the afternoon, especially in the summer.
- The best prevention of childhood diseases is breastfeeding. From the age of six months, the baby can and should be introduced to complementary foods.
- The child must be active, crawl and walk a lot. Exercise for children and regular massage will also be useful.
- Prevention of rickets can begin before the baby is born: in the last months of pregnancy, it is useful for the expectant mother to walk in the sun more often and eat foods containing vitamin D.
- Rickets can also develop in older children. To prevent this condition, it is important for the child to lead an active lifestyle, often be in the sun and eat well. The baby's diet should include foods rich in vitamin D: dairy products, liver, fish oil and sea fish.
- It is also important that the baby’s body receives a sufficient amount of phosphorus and calcium. Phosphorus compounds are found primarily in dairy products, seafood and fish. Legumes are rich in phosphorus, but its absorption is difficult. In order for phosphorus from legumes to be absorbed, they need to be soaked in water for a long time before cooking.
- Calcium is found in seafood and in the green leaves of various vegetables: Chinese and ordinary white cabbage, broccoli, parsley leaves, celery, spinach. Calcium is also found in poppy seeds and sesame seeds. Legumes are also rich in this mineral.
Pathogenesis (development) of the disease
Vitamin D is ergocalciferol (entered into the body from food) or cholicalciferol (formed in the body under the influence of UV rays). Due to a number of reasons described above, there is a lack of vitamin D in the child’s body.
What happens in a child’s body with a lack of vitamin D, why are metabolic processes disrupted and bones deformed?
Hypovitaminosis D leads to impaired absorption of calcium in the intestine , which results in hypocalcemia (low calcium levels in the blood). Because of this, the function of the parathyroid gland is enhanced = the parathyroid hormone of this gland promotes the leaching of calcium from the bones (to increase the level of calcium in the blood). This is osteomalacia , i.e. the process of softening bone tissue.
In addition to affecting calcium metabolism, parathyroid hormone also interferes with phosphorus absorption . The level of phosphorus in the blood decreases - this is hypophosphatemia . Because of this, redox processes are disrupted, resulting in acidosis (increased acidity in the blood balance, i.e. pH decreases). In an acidic environment, calcium salts are not deposited in the bones, but remain dissolved in the blood.
As a result, as the child grows, instead of normal bone tissue, rough connective cartilaginous tissue (which does not have the properties of bone tissue) is formed. This is osteoid hyperplasia , i.e.
the process of formation of defective bone tissue.
Severity of rickets in children
There are 3 degrees of severity of rickets in children:
- 1st degree of rickets corresponds to the initial period of the disease (see below);
- Stage 2 rickets is characterized by moderately pronounced changes in the child’s skeletal and muscular systems;
- Stage 3 rickets is a severe degree in which not only damage to the skeletal and muscular systems occurs, but also a pronounced lag in the child’s psychomotor development. It is characterized by the appearance of complications and residual effects of rickets.
Serious consequences
In adults, among the consequences of the disease (especially after suffering rickets of the second degree), the most common are astigmatism, myopia, narrowed pelvis (during pregnancy this is a direct indication for a cesarean section, and in the postpartum period breastfeeding is excluded), malocclusion, osteoporosis, flat feet, dental disease (caries, periodontitis, gingivitis).
After suffering from rickets, it is necessary to prevent its reappearance, follow the rules of good nutrition, follow all doctor’s recommendations, exercise, and walks in the sun.
Clinic (symptoms) of rickets in children
The first signs of rickets in children begin in the 2nd month of life, and in premature babies they can appear in the first weeks of life. Clinical symptoms of rickets in children depend on the period of the disease.
Periods of rickets in children:
- Period of initial changes . During this period, the child’s nervous system suffers the most. The baby becomes emotionally labile (suddenly begins to cry for no apparent reason, but can calm down just as quickly). The child shudders in his sleep and often wakes up. Appetite disturbances occur (the child eats sluggishly and reluctantly). One of the important signs of rickets in this period is increased sweating of the baby (especially the scalp). Sweating causes itching, the child tries to scratch the head, as a result of which the hairs are wiped out and baldness of the back of the head occurs. Signs of osteomalacia appear - the edges of the child’s fontanelle (or fontanelles in premature babies) become pliable to the touch. Craniotabes appears - softening of the bones of the skull. When undressing a child, a sour smell of sweat comes from the clothes. The child's urine also takes on a sour, ammonia-like odor. This period lasts 3 – 4 months.
- The peak period of the disease (begins in a child after 5 months of life). During this period, the baby’s skeletal and muscular systems suffer most severely (visible changes are shown in the figure below):
- Changes on the skull . Late closure of the fontanelle, frontal and parietal tubercles are pronounced. Formation of malocclusion.
- Chest deformity . At the border of the bone and cartilaginous joints of the ribs, tubercles appear - “rosaries” . There is a depression (depression) under the ribs, called Harrison's groove . The chest has the shape of a truncated cone with an expanded lower aperture. The deformation of the sternum is similar to that of a chicken breast or a shoemaker's breast (the ribs protrude strongly forward).
- When the child is seated early, a rachitic hump or kyphosis is formed.
- Deformation of the bones of the limbs . The limbs have two types of curvature: O and X - shaped curvatures (the figure shows an O - shaped curvature of the legs of a patient with rickets). Bracelets are formed on the hands (in the wrist joints), on the phalanges of the fingers - strings of pearls - all these are thickenings of the epiphyses, which become visible visually.
- Muscular system . In patients with rickets, hypotonia of the striated and smooth muscles develops (therefore, the child has a flat stomach - “frog belly” ). Looseness of the articular-ligamentous apparatus occurs.
- Children suffering from rickets experience shortness of breath, tachycardia, and decreased appetite .
- There is a delay in psychomotor development , which with timely treatment goes away without consequences.
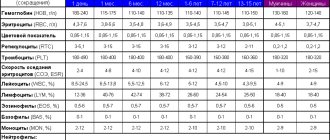
- Children with rickets are prone to anemia. Their immunity reduced , which means there is a high risk of secondary infection.
- Period of convalescence . Recovery period. Some believe that it is not necessary to treat rickets and that rickets will go away on its own without treatment by the age of 4 years. However, it is not. Children with untreated rickets suffer from residual effects of this disease.
- Period of residual effects . After severe rickets and untreated rickets, children remain with residual symptoms. These may be deformations of the pelvic bones (for example, a narrowed pelvis - in a woman it can subsequently lead to birth injuries to her child during childbirth or be an indication for a cesarean section), flat feet, malocclusion, persistent caries of milk and permanent teeth, fragile bones that become susceptible to frequent fractures, arthritis and other phenomena.
The second period of rickets lasts for several months, then, with timely treatment, the third period begins.
Clinical features
Characteristic clinical manifestations of the disease are:
- skeletal deformation, bowed legs;
- vague bone pain in the back, pelvis, lower back, hips and chest;
- hypotension and weakness of muscle and bone tissue;
- muscle wasting;
- change in gait;
- anemia and whiteness of the skin;
- decreased level of immune defense, which contributes to the occurrence of viral and infectious diseases;
- in the climacteric form of the disease – pronounced kyphosis and changes (deformation) of the pelvis;
- tendency to frequent fractures;
- nervous system disorders.
As a complication of insufficiency, absence or poor absorption of vitamin D, osteomalacia occurs in adults.
The cause is hereditary predisposition, renal failure, impaired metabolism of vitamin D, and rare exposure to the sun.
Experts consider the puerperal form to be the main form of osteomalacia. Women aged 20-45 years are susceptible to the disease, especially often during re-pregnancy, less often in the postpartum period or during prolonged breastfeeding, it is at this time that a woman’s body needs a large amount of vitamin D.
The pelvic bones, lower parts of the skeleton, and femurs are affected. The development of the disease is accompanied by increased fatigue, softening of the bones, their unstable shape, deformation of the pelvis, muscle contractions of the hips, difficulty walking (duck walk), decreased growth, and the onset of paralysis and paresis.
The disease occurs in a chronic form with increased pain, gradual exhaustion, has an undulating course and depends on concomitant diseases. A characteristic feature when making a diagnosis is the occurrence of an osteomalatic pelvis (reduction in the diameter of the pelvis and the formation of the coracoid symphysis) and pain in the pelvic bones.
It is necessary to differentiate osteomalacia with neuralgia, rheumatism, and osteitis. It is possible to avoid the disease with a nutritious diet rich in vitamins, salts and phosphates. Treatment is carried out as for rickets in adults.
Treatment of rickets in children
Treatment of rickets is outpatient. Vaccinations for rickets are carried out in accordance with the National Vaccination Calendar.
The basis of the treatment of rickets in children is the creation of conditions favorable for the development of the child and helping to prevent complications:
- Walks with the child should be carried out every day, preferably several times (depending on the weather).
- If the child is small, it is necessary to frequently change the position in the crib.
- The development of skills in a child (sitting, turning over, walking) should only be done at the request of the child, in no case by force! This can lead to curvature of the baby's bones.
- Massage courses are recommended, but please note that at first the massage should be gentle.
- Light exercises in accordance with the child’s age and condition (after consultation with an orthopedist).
- Feeding the baby. If you are breastfeeding, then the mother's diet should be balanced, additional vitamins, meat, and dairy products should be present in the diet daily! When artificially feeding, use a good adapted milk formula, not milk from cows or goats! Please note that with rickets, complementary foods are introduced into the child’s diet earlier than in other children (regardless of whether the child is fed breast milk or receives an adapted formula). For example, cottage cheese is introduced from 3 months. It is better to consult with your doctor about the specifics of introducing complementary foods for your child.
Drug treatment of rickets in children
The basis of treatment for rickets is a course of vitamin D. As a rule, children are prescribed a daily dose of 3000 to 5000 IU (international units) depending on the severity of the disease).
Vitamin D oil solution – 1 drop of oil solution contains 1500 IU.
Aqueous solution of vitamin D – 1 drop of aqueous solution contains 500 IU.
The course of treatment is approximately 1.5 – 2 months.
After the main course, a prophylactic dose of vitamin D of 500 IU per day is prescribed for the next two to three years after the illness.
In addition to vitamin D, the following is prescribed:
- Calcium preparations. To avoid the occurrence of spasmophilia during recovery from rickets, children are prescribed calcium supplements (calcium gluconate, calcium glycerophosphate) for 2 weeks.
- In case of muscle hypotension, the child is given injections of ATP (adenosine triphosphoric acid).
- Additionally, B vitamins and ascorbic acid are prescribed.
- Physiotherapeutic treatment is recommended - medicinal baths, ultraviolet radiation - irradiation. During the UV treatment, vitamin D intake will be canceled (to avoid its excess).