A dangerous bacterial pathology, the mortality rate of which reaches 10% - infectious meningitis. Its formation in adults and school-age children is caused by hemophilia, pneumococci, and meningococci. Haemophilus influenzae and meningococcal meningitis are droplet infections diagnosed in children visiting closed children's institutions.
Characteristics of the pathological syndrome
Severe pathology accompanied by an inflammatory process of the bases of the spinal cord and/or brain. There are several types of fabrics: hard and soft. Depending on the location of the lesion, the following types of diseases are distinguished:
- leptomeningitis - occurs most often; with this form of the disease, soft tissues are injured;
- pachymeningitis – damage to the hard membranes of the “gray matter”, diagnosed in 2% of 100 patients;
- Panmeningitis is an inflammation of all brain tissues.
In medicine, when diagnosing meningitis of various forms of an infectious disease, it is understood that only the soft membranes of the “gray matter” are affected. This is one of the most serious pathologies that provokes the development of complications, impaired mental development, and permanent disability.
Forms of infectious disease
Before the creation of antibiotics, the risk of death reached 95%. The use of penicillin drugs has reduced the mortality rate.
In modern medicine, synthetic medications are used to treat meningococcus; to prevent many forms of the disease, special vaccines are used against the most common pathogens - Haemophilus influenzae, meningococcus and pneumococcus.
The infectious form of the disease includes:
- Meningococcal meningitis. Diagnosed in children, adolescents and young adults. Meningococcal infection is transmitted from carriers of the bacilli or patients.
- Hemophilic type of disease. This form of meningitis most often occurs in infants and children under 5 years of age. In adults, we are talking about a secondary type of infection during the inflammatory process of the sinuses and middle ear.
- Pneumococcal meningitis. It develops as a secondary infection during another type of inflammation. It is diagnosed regardless of age, but the majority of patients are people over 50 years old and infants.
Meningitis as an infectious form of pathology is quite rare, only in isolated situations or during outbreaks recorded every 10-25 years.
Infectious forms of the disease
Treatment
First of all, medical measures are aimed at the source of infection and at eliminating the pathogen. However, it should be noted that the patient’s health condition does not always make it possible to carry out such therapeutic measures.
First of all, the patient is hospitalized in a medical facility. If the patient was not immediately sent to a specialized hospital, he can be transferred locally only after the patient’s condition improves or stabilizes. Clinical measures against the virus are carried out using etiotropic agents.
The treatment program includes the following measures against meningococcal infection:
- antibacterial therapy;
- saline infusion therapy;
- anti-seizure medications;
- glucocorticosteroids;
- detoxification therapy;
- drugs with a syndromic spectrum of action.
It should be noted that if the patient’s family has children of primary preschool age or employees of child care institutions, vaccination against meningococcal infection is mandatory. Vaccination against infection should also be carried out as a preventive measure.
Treatment of meningococcal infection is possible on an outpatient basis only if a localized form of infection is diagnosed. In all other cases, treatment must be carried out only inpatiently, according to the protocol of the Ministry of Health.
The patient can be discharged only after the cerebrospinal fluid and blood levels are normal. A nasopharyngeal swab is taken only after three days after antibacterial treatment.
Routes of transmission of meningococcal bacillus
Primary damage to the bases of the brain as an infectious disease develops under the influence of pathogenic bacteria. Microorganisms and viruses that cause meningitis are transmitted in different ways:
- by airborne droplets: the pathogen is released with mucus when sneezing and coughing, saliva;
- contact method: in direct interaction with a patient or a carrier of the virus, using common household items, hygiene products, towels, dishes;
- by the fecal-oral route due to poor personal hygiene: eating with dirty hands, consuming unprocessed fruits and vegetables;
- hematogenously: the causative agent of the disease of various origins is transferred through the blood plasma, then the infection spreads throughout the body to the membranes of the “gray matter”;
- lymphogenous route: the infection spreads to all organs through the lymph;
- placental: with the intrauterine formation and passage of a “provocateur” of the inflammatory process through the placenta, as well as infection in the tract during labor or penetration of an agent from the amniotic substance to the fetus;
- orally: when swallowing water infected with meningococcal bacillus (while swimming in pools, reservoirs, drinking unboiled liquid).
Outbreaks of infectious meningitis most often occur in winter and early spring, when people constantly stay in unventilated, stuffy rooms. The causative agents of the disease, entering the external environment, quickly die. The likelihood of infection is high only in close, close contact with a sick person.
Men and boys suffer meningitis much more severely than the fair sex. If there are any signs of inflammation of the meninges, you should immediately consult a doctor.
Outbreaks of infectious meningitis most often occur in winter and spring.
Origin of infectious pathology
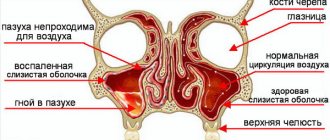
In addition to meningococcus, the causative agent of meningitis can be pneumococcus or tuberculosis bacillus. Often, the infection spreads to the membranes of the human brain due to inadequate treatment of certain pathologies:
- Sinusitis.
- Rubella.
- Pigs.
- Osteomyelitis of bones.
- Otitis.
Among adult patients, men aged 20-30 years are susceptible to the disease. A common cause of inflammation at the base of the “gray matter” at this age is neglect of one’s health.
Representatives of the fairer sex are less susceptible to meningococcal infection, but during pregnancy the danger of the pathological process increases due to the weakening of the body's defenses. The best prevention of the disease is timely sanitation, vaccination, treatment of diseases of inflammatory origin, and limiting contacts.
Prevention
If this disease is diagnosed in a family or institution, you should definitely report it to the sanitary and epidemiological station. They will take the necessary preventive measures. If an infection was detected in a children's institution, quarantine is established for at least 10 days as part of preventive measures. Vaccination is mandatory.
As for general prevention, in this case there is practically no way to completely eliminate the development of infection. Today, vaccination is the most effective preventive measure.
Signs of an infectious disease
After contact with a carrier of meningococcal bacillus and possible infection, the symptoms of the inflammatory process make themselves felt only after some time. The incubation period of the disease may vary in duration, depending on the age category and general health, but generally it lasts 1-7 days.
Meningococcal viral meningitis and its symptoms manifest themselves as follows:
- migraine attacks;
- meningitis is accompanied by a high temperature of up to 40 degrees, chills, and fever;
- increased sensitivity to irritating factors: tactile, sound, light;
- hallucinations, confusion, dizziness, even to the point of coma;
- loss of appetite, severe vomiting, feeling of nausea;
- meningitis makes itself felt by stool disorder;
- pressure on the eyes, conjunctivitis, lacrimation;
- soreness of the lymph nodes;
- unpleasant sensations in the area of the trigeminal nerve trunk;
- Kernig's symptoms: it is impossible to straighten the lower limbs at the knees;
- a positive reaction to Brudzinski’s sign: unconscious movement of the arms and legs when pressing, tilting the head;
- meningitis is manifested by Pulatov's symptoms: unpleasant discomfort when tapping on the head;
- Mendelian sign: when pressed behind the auricle, painful sensations occur.
In addition to meningococcus, the causative agent of meningitis can be pneumococcus or tuberculosis bacillus
In infants, meningococcal meningitis develops rapidly. Newborns suddenly have a fever, they become lethargic, restless, tearfulness appears, and the babies resist being picked up.
The main sign of inflammation of the meninges in children is swelling of the fontanelle, impaired respiratory function, and convulsions.
Among the uncharacteristic symptoms of an infectious disease are:
- Impaired vision, strabismus, double objects.
- Change in hearing.
- With meningitis, paresis of the facial muscles is observed.
- Catarrhal pathologies: runny nose, cough, pain in the larynx.
- Unpleasant discomfort in the abdominal area, constipation.
- With meningitis, seizures occur.
- Epileptic seizures.
- Bradycardia, rapid heartbeat.
- High blood pressure.
- Constant drowsiness, lethargy.
- Aggression, irritability.
Symptoms of meningitis in children and adult patients can manifest themselves in completely different ways. In preschool age, the disease develops faster, the incubation period is reduced to ½ day.
When an inflammatory process occurs in children under 3 years of age, it is difficult to establish all the signs of the disease; the child is not yet able to talk about his complaints. It is very important to closely monitor the health of your child.
Meningococcal meningitis develops rapidly in infants
What it is?
Disease history
Several centuries BC. e. and in the medieval period a disease with similar symptoms was described. In 1887, Vekselbaum isolated the causative agent of this type of meningitis in liquor cells. In 1889, W. Osler discovered meningococcus infection in the blood.
This led to the conclusion that the microorganism can cause not only inflammation of the meninges, but also other forms of the disease (nasopharyngitis, meningococcemia). In 1973, the last increase in incidence was registered in our country, and today incidence rates remain high.
However, domestic scientists have done tremendous work to study this disease. These are the scientists: Vlasov V.A., Pokrovsky V.I., Lobzin Yu.V., Vengerov Yu.Ya. and others. This significantly improved the outcome of meningococcal meningitis and sharply reduced mortality in the case of a generalized form.
Epidemiology
Susceptibility to the microorganism is low, about 0.5%. The main unfavorable factors for infection are large groups of children, close, long-term communication, the level of meningococcus in the air, and disturbed temperature and humidity levels in the room.
Reference! Children under 5 years of age are most often susceptible to infection. The disease is characterized by seasonality: in winter and spring there is an increase in incidence.
This is due to unfavorable weather conditions. Researchers say there are cyclical rises in the occurrence of infections. They appear every 10-12 years, lasting about 4-6 years. They are associated with periodic replacement of the pathogen by serogroups.
Pathogens and transmission routes
The causative agent of the disease is called meningococcus – Neisseria meningitides. This is a gram-negative microorganism that is immobile, overly variable, but extremely unstable to environmental factors: it dies in a short time at low temperatures or temperature fluctuations, as well as under UV rays.
Meningococcus has the shape of a coffee bean with a capsule, which is a pathogenicity factor.
Ways of transmission of infection:
- Airborne: during sneezing, coughing, talking. The most dangerous distance is within 0.5 m. A person inhales contaminated air.
- Contact: unlikely due to the rapid death of the microorganism.
Incubation period and developmental stages
During meningococcal meningitis, the following stages of infection development are distinguished:
The incubation period is the time from the bacteria entering the body to the appearance of symptoms of the disease. It most often lasts about 2-7 days.- The prodromal period is the period of time that occurs before the height of the disease. A specialist may notice it before clinical signs of infection appear. There is weakness, sweating and a slight increase in temperature. The duration of this stage is several days.
- Stage of pronounced manifestations of the disease : characterized by the appearance of typical symptoms and the development of adverse consequences.
- Stage of outcome of the disease : taking into account the timeliness of treatment, correctly chosen treatment tactics and the presence of complications, the outcome of meningococcal meningitis can be different - complete recovery, relapse of the disease, the appearance of complications, death.
Diagnostic methods and course of therapy
The initial examination of the patient is to identify clinical signs of meningitis and the presence of certain rashes. For a correct diagnosis, which will make it possible to establish the presence of a certain type of pathogen, it is necessary to take a test for bacteria, puncture the cerebrospinal fluid, and study the nasopharyngeal mucosa.
Meningococcal viral meningitis, treatment of which is carried out only in a hospital setting, requires special attention from doctors. The sooner a patient sees a doctor, the greater his chances of recovery and the absence of possible problems in the future. Methods and duration of therapy depend on the form, severity of the pathology, as well as the presence of concomitant diseases.
Treatment of meningitis consists of the following principles:
- the patient is prescribed antibiotics - intravenous and intramuscular;
- detoxification treatment of meningitis is carried out;
- vital functions of the body are supported with the help of B vitamins, ascorbic acid, cocarboxylase;
- it is possible to use plasma expanders and glucocorticoids;
- to prevent cerebral edema during meningitis, diuretics are prescribed;
- For medical reasons, medications are prescribed to increase blood pressure and oxygen therapy is provided.
Meningococcemia is a generalized form of infection of meningococcal origin, characterized by bacteremia with massive death of pathogenic microorganisms, manifested by symptoms of advanced septicemia with thrombohemorrhagic syndrome and toxic shock. This type of disease requires special and long-term treatment, just like meningococcemia.
What are the risk factors for meningococcemia?
Children and adolescents ages 5 to 19 are at greatest risk for meningococcemia. Newborns receive antibodies from their mothers through the placenta, although these antibodies disappear several weeks to months after birth. Toddlers are not immune, and there have been several infections in everyday settings. As children age, they gradually become immune to meningococcal strains by coming into contact with weaker strains of the bacteria. However, since this immunity is imperfect, adults can get meningococcal meningococcemia.
The immune system is critical when fighting bacteria. Patients who have a history of a specific genetic deficiency in the complement system (a set of complex proteins constantly present in the blood) are at high risk of severe illness. The spleen is also essential for an effective immune response, so people are at higher risk of severe illness if they have had their spleen removed or if it is not functioning well.
People who have been in close contact with an infected patient are at increased risk of infection. People who live in close proximity, such as military personnel in barracks, are at particular risk of the disease because one infected person can spread the disease to many others. One study found that transmission rates within households were 500 times higher than between the general population.
In some parts of the world, outbreaks of meningococcal disease occur regularly. This refers to a group of countries in sub-Saharan Africa known as the "meningitis belt". Since pilgrims from this area visit Saudi Arabia during the Hajj, there have been outbreaks associated with the pilgrimage. Saudi Arabia now requires proof of meningococcal vaccination before accepting pilgrims. Preventing such outbreaks is entirely possible; for example, many US universities now require proof of meningococcal vaccination before students can attend classes.
Auxiliary therapies
In combination with drugs that are active against “provocateurs” of pathology, symptomatic drugs are prescribed. These include:
- Anti-swelling medications for meningitis: Mannitol, Furosemide.
- Anticonvulsants: Phenobarbital, Relanium, Seduxen.
- Detoxification methods for treating meningitis: infusions of electrolytes, crystalloids, colloids.
- Nootropics.
Depending on the development of the pathological process or emerging complications, treatment of meningococcal meningitis may include correction of concomitant diseases: cardiovascular, adrenal, and respiratory failure.
Nootropics are an auxiliary part of therapy
What can a patient expect after illness?
Meningitis is a dangerous pathology, both in the process of infection of the membranes of the “gray matter” and the possible consequences.
Complications of an infectious disease include:
- hearing problems;
- epilepsy attacks;
- endocarditis;
- purulent arthritis;
- poor blood plasma clotting;
- mental retardation;
- mood swings, excessive excitability;
- If infected in infancy, hydrocephalus may develop.
The life of the patient depends on timely treatment of meningitis. At the first symptoms, you need to urgently visit a doctor or call an ambulance team. If signs of pathology appear in a baby, diagnosis should be made as quickly as possible - with the rapid progression of the disease in children, minutes count, and this will determine whether therapy will help or not.
Meningitis can lead to mental retardation
Possible complications
The most common complications of acute nasopharyngitis are:
- Development of a chronic form of nasopharyngitis.
- Inflammation of the middle ear often occurs, especially in young children. Such a complication can be suspected when the temperature rises again.
- In rare cases, laryngotracheobronchitis, bronchiolitis and pneumonia occur.
- Viral nasopharyngitis can cause asthma.
Timely, high-quality treatment can eliminate the likelihood of complications from acute nasopharyngitis in children.
How to prevent inflammation
There are no reliable ways to help protect your baby from the disease. An effective vaccine against meningitis has not yet been created. At the first symptoms of pathology, it is better to immediately consult a doctor rather than self-medicate.
Nonspecific methods of protection against meningitis:
- Limit your child’s contact with a potential carrier of the virus.
- During an epidemic, it is better to wear a medical bandage when in public institutions or municipal transport.
- Wash your child's hands thoroughly after going outside.
- You should not visit cities where there is an outbreak of the epidemic.
- Avoid swimming in open water.
By following these simple tips, you can reduce the likelihood of infection. But do not forget that the incubation period for meningitis depends on the type of pathogen and can last from ½ day to 35 days. At the first alarming signs of an inflammatory process, it is better to immediately visit a doctor.
During an epidemic, you should wear a medical bandage
Prognosis for a patient after suffering a pathology
With quick, correct diagnosis of the disease and effective therapy, meningococcal meningitis cannot cause harm to most vital systems and organs - there will be no irreversible consequences in this situation. But in some cases, the patient loses visual functions and hearing, and he may be bedridden for a while.
A large number of deaths due to inflammation of the membranes of the “gray matter” are observed only with the rapid progression of meningococcemia. In other cases, irreversible effects occur in only 1% of patients, but sometimes epilepsy or hydrocephalus may develop.
If a child has suffered from an infectious pathology, he is constantly monitored by doctors, he is undergoing medical examination for some time - 2 years. With inadequate therapy or incorrect diagnosis of the disease, the patient often experiences a relapse 1-4 weeks after the end of the course of treatment.
You should not try to get rid of meningitis on your own; only timely examination and proper therapy will keep your child healthy and prevent the development of serious consequences.